Paediatrics
advertisement

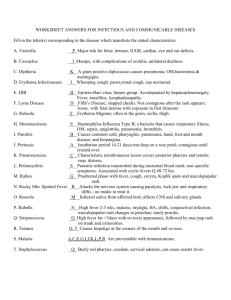
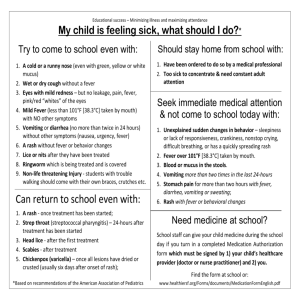
Paediatrics: - common conditions for finals. Dr Katie Green FY2 Paediatrics What we’ll cover • Additional topics – infection, syndromes, miscellaneous, child abuse • Quizes and Questions throughout • Summary of finals topics at end! Cardiovascular Topics • Murmurs- Innocent vs pathological • Congenital heart disease – Down’s syndrome • Kawasaki’s disease • Rheumatic Fever Homework… cardio exam of a child • Wash hands, introduce yourself….play the game! • Look- bedside clues, scars, clubbing, on oxygen? • Feel- pulses, praecordium (heaves), hepatomegaly, peripheral oedema • Listen- heart sounds, lung bases • Thank child and wash hands • Present your findings and summarise • It’s paeds- go with the flow, examine in whatever order you like Innocent Murmurs Can be louder / exaggerated in periods of illness Hallmarks: 7’s inoSSents 1. Soft 2. S1 and S2 Normal (Heart sounds normal) 3. Symptomless 4. Systolic 5. Short 6. Standing / sitting may vary (change with posture) 7. Special Tests Normal (ECG/CXR/ECHO normal) …also commonly Left sternal edge ( no radiation) Acyanotic murmurs VSD > PDA > ASD Left to right shunts No cyanosis (oxygenated blood being shunted) Can all cause pulmonary HTN Eisenmenger’s syndrome Left to right shunts (Acyanotic) VSD •Most Common CHD •Murmur reversely proportional to size of hole Presents – SMALL: asymptomatic. Thrill over the lower sternal edge. Loud pansystolic murmur at lower left sternal edge. Quiet 2nd heart sound. LARGE – HF, Failure to thrive, chest infections after 1 week of age. Soft pansystolic or no murmur. Loud second heart sound Tests – Small: ECHO Large: CXR, ECG, ECHO Management: – SMALL: most close spontaneously – LARGE: HF with diuretics and captopril. Definitive surgical closure. •Dental propylaxis controversial – not these days but still in books! Left to right shunts PDA • “Continuous Machinery murmur” beneath the left clavicle = Burrrr Durrrrrr •Tests: Echo •Management – 1. Asymptomatic must close to reduce endocarditis risk. 1 yr done via catheter. 2. Symptomatic: close immediately. •Indomethecin to close the PDA •Prostaglandin E keeps PDA open (for TGA’s) Acyanotic = Left to right shunts ASD • May be asymptomatic. If severe HF, Recurrent chest infections. • Signs: wide fixed splitting 2nd heart sound +/ejection systolic murmur. • Investigations : CXR, ECG, ECHO • Management: Surgery • Risk of arrhythmias as adults (AF/SVT) Outflow obstructions • Aortic stenosis (Ejection systolic murmur) • Pulmonary stenosis (Ejection systolic murmur) • Coarctation (radiofemoral delay) Turner’s Syndrome Outflow obstruction Coarctation •Uncommon •Turner’s syndrome (XO)! •Presents – ejection systolic murmur at the L upper sternal edge. High BP in the right arm. •Rib notching on CXR= ‘3 sign’. •Management: Stent if severe. Coarctation Murmurs…in summary Murmur Heard • Wide fixed splitting of S2 “Lub splat” • Pansystolic murmur “Burrrrr” • Ejection systolic murmur “Burr de” • Continuous machinery murmur “BurrrrDurrrrr” Pathology • ASD • VSD, Mitral regurg • Aortic stenosis, Pul stenosis • Patent Ductus Arteriosus Murmurs in summary…. Oh murmur, where art thou…? www.askdoctorclarke.com Cyanotic murmurs TOF / AVSD / TGA Truncus Arteriosus / Pulmonary Atresia / Hypoplastic left heart Right to Left Shunts Cyanosis (de-oxygenated blood being shunted) 4 cardinal features: TOF Pulmonary stenosis (causing Large VSD), Right ventricular Hypertrophy (RVH). Overriding aorta. VSD Ejection systolic murmur – left sternal edge •Present cyanosis on exercise / 2+ days of life. Clubbing. Right parasternal heave •Cyanotic spells when upset •Investigations: CXR – boot shaped heart. ECHO (increased right ventricular size). •Management: •Beta blockers for hypoxic spells. Palliative surgery = blalock-taussig shunt. Total surgical repair around 6 months. Transposition great arteries • Present – cyanosis (only cyanotic condition that can present from birth). • Aorta comes off right ventricle, PA off left ventricle • Profound and life threatening. Less severe if VSD as mixing of the blood. Clubbing. Usually no murmur. PDA. • Tests- x ray shows ‘egg on side appearance’. ECHO • Management – prostaglandin infusion to maintain PDA (allows blood mixing). Balloon atrioseptostomy – tears atrial septum to essentially make an ASD. Graft surgery. Congential murmurs and syndromes Downs: AVSD, VSD, ASD. Turners: Atrial stenosis and Coarctation Trisomy 13 + 18 : complex septal defects Williams: elfin features + supravalvular aortic stenosis Noonans : tricuspid stenosis and septal defects William’s Syndrome • Elfin features • Supravalvular Aortic stenosis Down’s Syndrome • Trisomy 21 • 50% have cardiac abnormality • AVSD, ASD, VSD, MR, TR Increased risk of: – – – – – – Duodenal Atresia Squint Hypothyroidism Leukaemia Hirschprung’s disease Deafness Kawasaki’s Disease • • • • • 6m to 4 years More common in Japanese children Unknown aetiology ? superantigen Systemic vasculitis – small and medium vessels Clinical features – Fever for >5 days – Four of: conjuncivitis, red mucous membranes, cervical LNs, rash, palm changes • Complications in 1/3 of cases; follow-up echos (risk of coronary artery aneurysms) • Prompt treatment with IVIGs and aspirin for 6 months (↓ thrombosis) Homework 2…the fetal heart Diagrams from (the amazing) www.askdoctorclarke.com Rheumatic Fever • 2-6 weeks after strep pyogenes infection (Group A Beta haemolytic strep) • >50% get ACUTE CARDITIS = pericardial rub • Often get Mitral Stenosis or Aortic Regurg years later as teen / adults • Diagnosed by strep positive throat swab/ASO titre and Duckett Jones major/minor criteria Sore throat / Arthralgia / Fever / Erythema Marginatum / Arthritis / Nodules / Chorea / New mitral diastolic murmur Rheumatic Fever Diagnosis requires: • 2 major criteria OR • 1 major criteria and 2 minor criteria Eisenmenger’s syndrome • SHUNT REVERSAL • Initially (large) left to right shunt • Due to blood shunted right, develop pulmonary artery hypertension to the point of right pressure exceeding left = shunt reversal = cyanosis • “Acquired Cyanotic Heart Disease” = acquired R L shunt • Poor prognosis – no management /reversal options • Heart-lung transplant is only hope Cyanosis • Cyanotic from birth = TGA’s • Cyanotic without murmur = TGA’s • Cyanotic on crying / day 2-3 of life = TOF • Cyanosis with Down’s syndrome = AVSD • Acquired Cyanotic heart disease = Eisenmenger’s syndrome CARDIO RECAP 1. What are the murmurs of: – – – – VSD PDA ASD Aortic stenosis 2. Classification of Congenital Heart Disease – Acyanotic – Cyanotic 3. Cardiovascular abnormalities of Down’s syndrome? 4. 5 diagnostic criteria of Kawasaki’s ? Respiratory • Infections • Cystic fibrosis • Asthma Bronchiolitis • Nearly always <18m • Viral infection (RSV) → small airway obstruction – Wheeze, harsh cough, fever, ↑hr and rr, nasal flaring, s/c & i/c reccession – Fine insp. crackles and expiratory wheeze – 9 day illness: 3 stable, 3 worse, 3 better – resolved! • Those at risk (prem, chronic resp conditions, CHD cardiac pts) = PAVALIZUMAB monoclonal antibody • Investigation only needed in severe cases – Capillary blood gas, CXR, nasopharyngeal aspirate (RSV) • Essentially Supportive Management : humidified oxygen, saline / bronchodilator nebs if severe. Management of Bronchiolitis Assess the clinical severity!! 1.Mild: feeding well, minimal RD, no RFs, no O2 needed – HOME with advice on when to return 2.Moderate: ↑ work of breathing, poor feeding, low sats, RFs – admit for feeding support +/- O2 3.Severe: worsening RD, respiratory acidosis, apnoea, dehydration, RFs – HDU, CPAP, ventilation, IV fluids Pneumonia • Up to 1/3 are viral (RSV, parainfluenza, adenovirus, rhinovirus) – wheeze more common • Usual Signs and symptoms • Mild – home with oral Abs and advice • Moderate to severe (unwell child, RD, needs O2, poor fluid intake) – admit, O2, IV Abs/fluids Croup and epiglottitis • Croup = Acute viral laryngotracheobronchitis – – – – Hoarse voice, barking cough, harsh stridor, possible RD Age 6m to 6y Parainfluenza virus Mx: mild (RD disappears at rest)/moderate/severe • Epiglottitis (H. influenzae): very unwell, drooling, leave alone and ask ENT to r/v immediately. Leave alone! Croup .vs. Epiglottitis Croup Epiglottitis Onset Over days Over hours Preceding cold Yes No Cough Severe, barking Absent/slight Able to eat and drink Yes No Drooling saliva No Yes Appearance Unwell Toxic, very ill Fever <38.5°C >38.5°C Stridor Harsh, rasping Soft, whispering Voice and cry Hoarse Muffled, reluctant to speak Bronchitis • Inflammation of the bronchi • Cough and fever are the main Sx ?wheeze • Lasts for approx. 2 weeks (longer if pertussis) • Whooping cough – – – – – – – – Highly infectious form of bronchitis Bordetella pertussis Catarrhal phase – coryzal Sx Paroxysmal phase – cough followed by inspiratory whoop Apnoea in infants Epistaxes and subconj. Haemorrhages can occur Ix: nasal swab, lymphocytosis Immunisation crucial - pregnant women Cystic Fibrosis • Autosomal recessive inheritance (gene on chromosome 7 codes for CFTR) • 1 in 25 are carriers in the UK – Mutation (ΔF508) → abnormal ion transport → thick secretions • Pancreatic insufficiency – DM and malabsorption (FFT, steatorrhoea – low elastase levels) • Recurrent chest infections and bronchiectasis Most present with malabsorption and FFT from birth Cystic Fibrosis • Clinical features – Newborn – screening (IRT/genetic testing) – Infancy – meconium ileus, jaundice, FFT – Child – rectal prolapse and nasal polyps – Older child – ABPA, DM, cirrhosis and portal hypertension, obstruction, pneumothorax, sterility. • Investigations – the sweat test (pilocarpine-PNS) – High Chloride levels (>60) – Usually high Na+ levels too • Managment – MDT – mostly respiratory and nutrition Asthma • Not diagnosed until >4 yrs • Reversible airway disease • Tends to be worse in mornings and at night = “diurnal variation” • Triggers- exercise, allergens, cold weather, stress / emotion. • Assoc with eczema and rhinitis (Atopy) • Tend to have: generalised expiratory polyphonic wheeze, tachypnoea, hyperinflated lungs on CXR • Rule of 3’s: 1/3 grow out of it, 1/3 improve in teens for it to return in adulthood, 1/3 have asthma throughout life. Asthma Management 1. Acute Management: – – – Oxygen, nebulized salbutamol + ipratropium, IV hydrocortisone, IV magnesium sulphate (need senior r/v by now) 10 puffs of salbutamol with spacer is as effective as nebuliser = “just get salbutamol into them however and keep giving it” approach!! Be aware of the silent chest – wheeze that disappears without treatment is a disaster and not a miracle!! 2. Chronic Management: – – – – – Avoid allergens, peak flow and symptom diary MDT involvement – specialist nurses are great Stepwise management <2 years: MDI with spacer and mask, 2-7 years: MDI with spacer, >7 years MDI Individual action plan Stepwise management of asthma Steps Treatment STEP 1: Mild intermittent asthma Short acting beta agonist: salbutamol +/- ipratropium STEP 2: Requires >3 puffs of beta agonist per week Inhaled steroid e.g. Budesonide or beclometasone STEP 3: Poorly controlled on inhaled steroids Long acting beta agonist: salmeterol/formoterol STEP 4: Persistent poor control Increase inhaled steroid dose Leukotriene receptor antagonist STEP 5: Chronic severe asthma Daily oral steroids Start where is appropriate, not necessarily from step 1. Causes of Stridor • • • • • • • • Croup, Epiglottitis, Anaphylaxis, Laryngomalacia, Foreign body inhalation, Bacterial tracheitis, Smoke inhalation Obstructive Malignancy. RESP RECAP 1. 2. 3. 4. 5. How are babies with CF likley to present? Which children are at risk of bronchiolitis? Name 4 causative ‘agents’ of pneumonia? How do you manage epiglottitis? Describe the stepwise treatment of asthma Gastrointestinal • • • • • Diarrhoea Abdominal pain Coeliac’s disease Pyloric stenosis Intussusception Growth Charts • • • • • • • • Correct prematurity until 2 years old (<36+6) Plot as dots and not crosses Coeliac- fall off in weight begins as weaning begins (6 months) IUGR- low birthweight baby, may catch up. Early IUGR if head circ and length also affected. May have reduced growth potential. Hydrocephalus = head circ much greater than length and weight and suddenly shoots up. Tumours / IVH Turner’s = poor growth from young age and absence of pubertal growth spurt. Short stature. GH deficiency = fall off in height- can be congenital but if sudden fall off likely to be pituitary deficiency (pit adenoma / tumour?). Aquired hypothyroidism has similar pattern. CF- failure to thrive, difficult to gain weight, weight always on lower centiles. Hx likely to suggest recurrent LRTI’s. Types of Vomiting (yay!) • Bile stained – intestinal obstruction • Blood in vomit – oesophagitis, peptic ulcer, oral/nasal bleed, malrotation • Projectile vomit- pyloric stenosis • Vomiting at end of paroxysmal coughing – whooping cough • Abdo distension- lower intestinal obstruction Gastro-oesophageal reflux • Mainly due to LOS immaturity and inappropriate relaxation. • Usually resolved by 1 year. • Chronic reflux due to diseases of neuro disorders such as Cerebral Palsy, chronic lung disease of prematurity • Symptoms- crying after feeds, vomiting after feeds, not wanting to lie down, reflux, anxious mother • Investigations: clinical assessment. Barium swallow, pH monitoring (24hrs), trial meds • Management: thickened feeds, positioning during feeds, PPIs, Surgery. Reassure mother this is common and usually self-resolves with age. GORD Treatment • GORD = Gaviscon Omeprazole Ranitidine Domperidone. • Surgery (Nissen’s Fundlopication) Pyloric Stenosis • • • • • • • • Hypertrophy of pylorus that causes outflow obstruction. 2-7 weeks. Boys > girls. Surgical Emergency Projectile vomiting which gets worse overtime. Constant hunger, weight loss, “scaphoid abdomen”, upset baby. Hypokalaemic Hypochloraemic Metabolic alkalosis =low plamsa K+ due to vomit Diagnosis – clinical olive on abdo. Oserve feed for visible peristalsis (mind out for vomit!) Ix = USS or barium meal Tx- correct electrolytes +fluids. NBM. Surgery Gastroenteritis • Infective vomiting and diarrhoea. • Rotavirus commonest in developing world. Worse winter. • Bacteria – campylobacter jejuni commonest but overall rare. Shigella and salmonella cause dysenteric infection. • Have a low threshold for admitting as many things can look like gastroenteritis (DKA) • Look out for dehydration – reduced conciousness, sunken fontanelle, dry mucus membranes, tachypnoea, tachycardia. Prolonged cap refill, weight loss, reduced skin turgor. • Investigations:- nil unless Septicaemia is suspected. There is blood and/or mucus in the stool. The child is immunocompromised. The child has recently been abroad. The diarrhoea has not improved by day 7. There is uncertainty about the diagnosis of gastroenteritis. Gastroenteritis Management = fluids fluids fluids!! •<5% Mild: feed replacement. Glucose + electrolyte until subsides •5-10 severe: 6hr 100ml/kg •>10% IV rehydration •Beware of hypernatraemic dehydration •Rehydration is mainstay of treatment •Beware outbreaks of e.coli O157 (haemolytic uraemic syndrome) Causes of Acute Abdo pain… Your Turn….! Birth-1 year •Medical causes Gastroenteritis, Constipation UTI •Surgical causes: Intussusception, Volvulus Incarcerated hernia •Other causes: Infantile colic Hirschsprung's disease 2-5 years •Medical, Gastroenteritis, Constipation, UTI •Surgical: Appendicitis, Intussusception, Volvulus, Trauma •Others: Mesenteric lymphadenitis, Henoch-Schönlein purpura, Sickle cell crises 6-11 years •Medical: Gastroenteritis, Constipation, UTI •Surgical: Appendicitis, Trauma •Other: Mesenteric lymphadenitis, Henoch-Schönlein purpura, Sickle cell crises, Pneumonia, Functional pain 12-18 years •Medical: Gastroenteritis, Constipation •Surgical: Appendicitis, Trauma, Ovarian/testicular torsion •Other: Dysmenorrhoea, Mittelschmerz, Threatened abortion, Ectopic pregnancy, Pelvic inflammatory disease Appendicitis • Acute appendicitis doesn’t really occur in children under 3 yrs. • Presents- anorexia, vomiting, abdo pain. Flushed face. Oral fetor. 37.2-38 C. Guarding • Watch out- kids can perf suddenly = low threshold for theatre • Treat – NBM, IV fluids, appendicectomy, iv antibiotics. Intussusception • Invagination of the proximal bowel into the distal segment. Commonest involves ileum into caecum. • COMMONEST postnatal cause of intestinal obstruction in infants. 2months-2 years. Presents: paroxysmal, severe colicky pain and pallor. Sausage shaped mass palpable in abdomen. Red current current jelly stool (late sign). Abdo distension + shock. Ix: Xray distended loops bowel. USS diagnosis and checking insufflation Tx - 75% reduced by air insuffation (NG tube). 25% reduced by surgery Malrotation • Ileocaecal and duodenaljejunal flexure are predisposed to volvulus due to short base. • Presents as obstruction +/- compromised blood flow. Bile or blood stained vomit. Perotinitis. Ischaemic bowel. • Usually 1-3 days with Ladds band obstructing duodenum • Surgical emergency = NBM, NG tube, Surgical management Henoch-Schonlein Purpura • Usually occurs post streptococcal infection • Small vessel Vasculitis • Preceded by infections: Group A streptococci, mycoplasma, Epstein-Barr virus. Vaccinations. Environmental exposures: for example, drug and food allergens pesticides, cold exposure, insect bites • Occurs more in the winter usually. • Macular rash is preceded by low grade fever and abdo pain. Can have bloody diarrhoea and swollen painful joints. • The rash is macula that progresses to papulae in a classic buttock and back of leg location. • Renal involvement in 50% of older but only 10% significant with 1% going to ESRF • Supportive management – steroids of really severe and if renal and joint involvement Purpuric rash! Abdo pain - Tips • • • • • • • • In females always consider gynaecological disorders and pregnancy-related disorders (you may need to speak to the patient alone) Male patients - always consider torsion of the testes Consider illicit drug use Is there a possibility of child abuse? In exams children being abused invariably have abdominal pain!!! Refer patient if you are unsure or concerned Repeat physical examination may help Use analgesia as required - it does not affect diagnostic accuracy Exclude medical causes such as pylenephritis, DKA, pneumonia, UTI Malabsorption Presents : –abnormal stools. –Failure to thrive. Or poor growth in most, not all cases = dropping centiles. –Specific nutrition deficiencies. –Difficult stools to flush and that have offensive pervading odour. • All must have diabetic assessment Coeliac Disease • Autoimmune disease- HLA B8. • Gluten causes damage to the villi in the intestinal mucousa causing it to become flat = crypt hypertrophy. • Presents: Failure to thrive in first few years (commences at 6 months when weaning begins). Irritable. Loose stools. Abdo distension. Wasting esp buttocks. Dermatitis herpetiformis. • Diagnosis: transglutaminase ab and anti-endomysial antibodies. Check IgA levels. Jejunal biopsy is gold standard (when eating gluten!!!) • Management: remove gluten from the diet. It before 2 years then must do a gluten challenge later in life to see if still susceptible to damage. • Free prescriptions for gluten free food! Diarrhoea • ‘transient dietary protein intolerances’ – usually presents with diarrhoea, eczema. • Acute colitis. • Abdominal Migraine. • Toddler diarrhoea – carrots and peas diarrhoea. Grow out of by ~5 yrs. NORMAL! Constipation This is common in breast fed children. Again in young children constipation and painful stools. Can follow febrile illness or superficial fissure causing refrainment from defecation. Bad potty training. Psychological stress. This causes faecal loading, reduced sensation of internal sphincter and finally soiling as the internal sphincter is overcome. Organic causes. Constipation. Hypothyroidism. Hypercalcemia. UTI. Hirshsprung Management. •Mild – increase dietary fibre. Stool softners (lactulose, docusate). stimulate ( senna). •Severe – evacuate the overload. Followed by 1-2 weeks of stool softners. Large doses of powerful laxatives. Encouragement by family is essentially Enemas are best avoided Hirschsprung’s Disease • Absence of of ganglion cells from mysenteric and submucosal plexuses. Results in narrow contracted segments. Abnormal bowel from rectum progressing upwards until you get a dialted uninnervated bowel. • Presents – failure to pass meconium and bowel distension. Later bile stained vomit. • PR – narrow segment and gush of poo and flatulence on removal. Temporary removal of obstruction can delay diagnosis • Can get associated hirschsprungs enterocolitis in first couple of weeks of life. Later life you get chronic constipation without overflow soiling • Diagnosis – demonstrate ganglion absence. Large acetyl-cholinesterase – ve positive nerve trunks on a rectal biopsy. Anorectal manometry or barium studies may be useful for surgery. • Tx surgery – remove bad section and reattach normal bit to the anus Misc Paeds • • • • • • • DKA Meningitis Imms Rashes Safeguarding / child protection Child with a limp Kidneys and UTIs • Triad: DKA 1. Hyperglycaemia 2. Ketosis (urine and serum ketones) 3. Acidosis (pH <7.3) • 30% of new diabetics present this way = Commonest new presentation • Risk factors = fhx diabetes, poor social circumstances, <5 yrs, adolescent girls, previous DKA • Serious = hypokalaemia, hypoglycaemia, dehydration, hypovolaemia, renal failure, cerebral oedema. • Be aware of gastroenteritis, dehydration with excess urine output and resp distress with no chest signs DKA Child abuse Risk Factors Physical – Bruises, bites, lacerations, burns, #, fabricated illness – Accidental, osteogenica imperfecta, coagulation disorders, SSS, mongolian blue spot (melanocytosis) Emotional – Aggressive behaviour, poor self esteem Sexual abuse – Involve senior paediatrician and avoid repeated examinations Neglect – Often manifests in developmental delay Management: SMACK Safety of the child is the priority Manage the medical problem Always discuss concerns with senior Contact social care Keep clear notes Non-accidental injury: NICE guidelines LISTEN and observe: history, examination and investigations. Seek an EXPLANATION: is it plausible, adequate and consistent? RECORD exactly who said what and when. DISCUSS the case with a senior experienced in child protection. Are you CONSIDERING or SUSPECTING child maltreatment? CONSIDERING: maltreatment is included in the differential diagnosis. Look into past history, talk to other agencies, arrange a prompt review of the situation. SUSPECTING: serious level of concern about maltreatment but no proof. Refer urgently to social services. Immunisationsgood old parrot fashion: learn and regurgitate! Age Vaccines 2 months Diphtheria, tetanus, pertussis, polio and Hib + pneumococcal 3 months Diphtheria, tetanus, pertussis, polio and Hib + meningitis C 4 months Diphtheria, tetanus, pertussis, polio and Hib + pneumococcal + meningitis C 12 months Hib + meningitis C 13 months MMR + pneumococcal 3 years and 4 months – 5 years Diphtheria, tetanus, pertussis, polio and Hib + MMR Girls 12-13 years HPV 16 and 18 13-18 years Tetanus, diphtheria and polio Case: The febrile child Mikey is a 4 year old boy who is rushed straight into resus because his parents are unable to rouse him. They tell you that he has had a fever for a few hours, then complained of a headache and vomited. On the way to the hospital they noticed a rash on his tummy, and he then started to become drowsy. Questions 1. 2. 3. 4. 5. What is the most likely diagnosis? What is a septic screen? What is the most likely organism in this case? How would you manage this condition? Is this a notifiable disease? Answers 1. Meningitis 2. Septic screen: blood cultures, urine culture, chest x-ray and lumbar puncture. 3. Neisseria meningitidis – Neonates: Group B strep, e.coli and Listeria. – 1 month- 6 years: Neisseria meningitidis, Strep pneumonia and Haemophilus influenzae. – More than 6 years: Neisseria meningitidis and Strep pneumoniae. 4. Call for senior help, IV fluids, IV cefotaxime/ceftriaxone, rifampicin for close contacts and check immunisation history. 5. Yes! Notifiable Diseases… Acute encephalitis Acute infectious hepatitis Acute meningitis Acute poliomyelitis Anthrax Botulism Brucellosis Cholera Diphtheria Enteric fever (typhoid or paratyphoid fever) Food poisoning Haemolytic uraemic syndrome (HUS) Infectious bloody diarrhoea Invasive group A streptococcal disease Legionnaires’ Disease Leprosy Malaria Measles Meningococcal septicaemia Mumps Plague Rabies Rubella SARS Scarlet fever Smallpox Tetanus Tuberculosis Typhus Viral haemorrhagic fever (VHF) Whooping cough Yellow fever Child with a limp • Perthe’s Disease- 4-8yrs, often boys, avascular necrosis femoral head. • SUFE’s – Obese, young teen, often boys, often have assoc groin pain. • Septic Arthritis- needs Abs ASAP = SAUPO • Juvenile Idiopathic Arthritis – erythematous, swollen joint, limited mobility, often fixed in position. • Fracture / Trauma • NAI • Osgood Schlatter Disease – usually young teens, athletic (gymnasts!) • Developmental dysplasia of hips The Child With a Limp Septic arthritis Features of septic arthritis: • Systemically unwell child • Erythematous warm joint • Pseudoparalysis due to pain Management: • Give IV antibiotics NOW • Initiate basic investigations: FBC, CRP, U+E, x-ray of the affected limb • Aspirate under US guidance and do cultures • Look for an underlying cause e.g. immunodeficiency Duchenne Muscular Dystrophy • Proximal muscle weakness • Affects boys • Life limiting (most die in teens) • Gower’s sign Epilepsy & Seizures A clinical event in which there is a sudden disturbance of neurological function due to an abnormal/ excessive neuronal discharge. • Largely a clinical diagnosis Classification of epilepsy: 1. GENERALIZED (ONSET in both hemispheres): absence, myoclonic, tonic, tonic-clonic, and atonic. 2. FOCAL (ONSET in one hemisphere): • simple partial seizure (consciousness unimpaired), • complex partial seizure (consciousness impaired), • partial seizure with secondary generalisation. Seizures Seizures Non-epileptic: febrile convulsions, metabolic , head trauma, meningitis/encephalitis, toxins/poisons. • • • Reflex Anoxic seizures- non-epileptic, syncope due to sudden drop in cerebral perfusion due to shock eg. bump to head, falling over etc. May go pale. Rapid recovery. Breath Holding Attacks- episodic apnoea, most common 12-18 months, frightening but reassure parents not dangerous. Child will outgrow. Pseudoseizures (exclude safeguarding issues). Diagnosis exclusion. Epileptic: idiopathic (70-80%). Also consider congenital cerebral abnormalities, encephalitis/meningitis, cerebral tumour, neurocutaneous syndromes. • • • Absence seizure- 3Hz spike and wave. Treat with Ethosuximide! (NOT VALPROATE). Can be bought on by hyperventillation. Grand Mal seizure- Tonic clonic (ask about tongue biting, incontinence, noises, pre and post-ictal phases, triggering activity). Partial Seizure- Focal seizures – simple = no unconsciousness, complex = loss of consciousness General Epilepsy Management – – – – – – – – MDT Involve the parent and child in decision making Family education Drug treatment: valproate for generalized and carbamazepine for focal seizures. Monitor levels and for side effects. Rescue medication (buccal midazolam/PR diazepam). Consider tapering off medications if patients are seizure free for 2 years. Remember DVLA for older teens Surgery for refractory epilepsy Cerebral Palsy Developmental Assessment Rashes The child with a rash: Name the rash…….. A long-standing rash in a 6 year old girl with asthma and a peanut allergy. The child with a rash: Name the rash….. Eczema Case: The child with a rash: Name the rash… A 5 year old boy develops small red macules that then develop into blisters. Case: The child with a rash: Name the rash Chickenpox Case: The child with a rash: Name the rash….. A 1 year old boy develops blisters on his face that burst and form erythematous areas with honey-coloured scabs. Case: The child with a rash: Name the rash…… Impetigo ADHD • Attention deficit hyperactivity disorder • Inattention, poor impulse control and motor overactivity. • Management: 1. Exclude other causes of the behaviour: chronic illness, sleep disorders, depression, problems at home. 2. Behaviour rating scales to establish severity 3. Psychosocial interventions: educate the family about ADHD and coping strategies 4. Behaviourally oriented treatments: to rectify problem behaviours 5. Medications: methylphenidate or dextroamphetamine (stimulants). Monitor growth and blood pressure. The Kidneys Kidney Abnormalities: Solitary kidney- unilateral renal agenesis. No treatment necessary if other kidney is normal Ectopic kidney- abnormal migration during embryogenesis = pelvic kidney or horse-shoe kidney. Associated with Turner’s. DMSA scan detects Multicystic dysplastic kidney- ureteric bud abnormality or proximal ureteric atresia. kidney non-functioning and usually disappears Autosominal dominant polycystic kidney disease-small cysts throughout kidney. Associated with tuberous sclerosis, ovarian cysts, cerebral artery aneurysm Autosomal recessive polycystic kidney disease- large cystic kidneys don’t produce adequate urine = reduced amniotic fluid and pulmonary dysplasia. Develop renal failure early childhood. Associated cystic liver disease. Detected fetally usually. UTI’s • • • • • • Girls > Boys Can present very vaguely- any unwell child potentially has UTI! Dip urine of ALL unwell children Can cause nocturnal enuresis Always think diabetes (polyuria) May have underlying vesico-ureteric reflux = kidney “scarring” Leukaemia • ALL is the commomest malignancy of childhood • Proliferation of immature white blood cells (blasts) • Symptoms due to bone marrow failure = bruising, anaemia, lymphadenopathy, bone pain, hepatosplenomegaly, neutropaenic infection • Diagnosed by bone marrow aspiration = replacement of normal cells by blast cells • Features of good prognosis = common subtype, female sex (males get 2 yrs chemo, females 1 yr), low WCC count, • Overall Good prognosis - >65% cured Cleft Lip & Palate Neural Tube Defects Autism S Y N D R O M E S I N F E C T I O N S Hot OSCE topics • Explaining – Inhalers, Down’s syndrome, CF, diabetes, screening in pregnancy, DMD. • Examinations – Neonate or child (incl. head circumference and hips), developmental delay (growth charts) • History or examination or management – Common GI/resp/CV conditions, child abuse, Abdo pain, febrile convulsions, seizures, constipation/soiling/bed wetting, recurrent UTIs, reflux • Videos – Developmental assessment, CF, cerebral palsy Questions? That’s it folks! Test Yourself QUIZ!! 1. Would you be concerned if you saw these patients at your GP surgery? QUIZ 2. A 10 month old child is admitted with difficulty in breathing and a cough. O/e they have fine inspiratory crackles and a wheeze and you notice slight intercostal reccession - What is the diagnosis and causative organism? Their mother says that in addition to finding it hard to breathe, and they haven’t been feeding well. Their sats are 93% OA. - Would you admit them? - How would you treat them? Management of bronchiolitis Assess the clinical severity!! 1.Mild: feeding well, minimal RD, no RFs, no O2 needed – HOME with advice on when to return 2.Moderate: ↑ work of breathing, poor feeding, low sats, RFs – admit for feeding support +/- O2 3.Severe: worsening RD, respiratory acidosis, apnoea, dehydration, RFs – HDU, CPAP, ventilation, IV fluids QUIZ 3. A child presents to A&E with a likely fractured arm. The X ray shows a fractured radius. You notice she has had multiple fractures in the past so go back to examine the child and find this o/e: What is the diagnosis? If you suspected child abuse, what would you do? S safety of the child is the priority M manage the medical problem A always discuss concerns with senior C contact social care K keep clear notes QUIZ 4. List 5 causes of abdominal pain in children – Which factors would make you suspect a psychological cause? 5. You see a 2 year old girl in A&E who looks extremely unwell. She is holding her throat with her mouth open. You notice she is drooling and has soft inspiratory stridor. She is not coughing. Her temperature is 39°C. Her mother is desperate that you examine her throat as she thinks she is choking. – How would you manage this patient; would you examine her? Case • 6 week old baby boy – Tyrone • Mum’s first child present with episodes of vomiting. And is a little worried as he is not keeping anything down though still eager to eat. • The vomiting has been present for the last week or so and can be quite vigorous, often hitting the wall. No blood. Brings up what is eaten. • O/e Tyrone looks fatigued. He has some dry mucus membranes. And you notice an olive like mass in the LUQ. • Investigations – U+Es, USS, barium swallow • Tx – fluid and electrolyte resus. Pylorotomy Case: The blue baby Kevin is a 3 week old baby who is brought to see the GP because his mum has noticed that he is going a bit purple around the lips. He also has crying spells where he is inconsolable and goes very pale. On examination you note cyanosis and a loud harsh ejection systolic murmur at the left sternal edge, radiating to the back. His chest x-ray Questions 1. What is the most likely diagnosis? 2. What are the key abnormalities in this condition? 3. How do you distinguish between cardiac and respiratory causes of cyanosis? 4. What are the crying episodes, and how would you manage them? Answers 1. Tetralogy of Fallot 2. 4 key abnormalities: a large VSD, over-riding aorta, subpulmonary stenosis, and right ventricular hypertrophy. Answers 3. Put the baby in a chamber with 100% oxygen and if the partial pressure of oxygen remains low then the heart and not the lungs is the problem. 4. Hypercyanotic episodes: there is an increase in cyanosis, inconsolability due to hypoxia, shortness of breath and pallor. If they last more than 15 minutes then urgent treatment is required as the infant is at risk of MI and stroke. Give sedation, morphine, IV propranolol and fluids. Key Revision Topics • Cardiac- basic murmurs (VSD, ASD, TOF, PDA, TGA, coarctation) and SVT • Resp- Asthma, C.F, Viral wheeze, croup, epiglottitis, Anaphylaxis, bronchiolitis, Pneumonias, Ear infections (Otitis externa, otitis media, glue ear) • GI- Coeliac disease, IBD (Crohn’s >UC), Constipation, Gastroenteritis, Intussusception • Psych / Developmental- Autism, Developmental milestones, Cerebral palsy • Infectious Diseases- Kawasaki, Rheumatic fever, Endocarditis, Meningitis • MSK- JIA, Lupus, Perthe’s disease, septic arthritis, SUFE • Hepatic- neonatal jaundice • Haem / Onc- Leukaemias (ALL), ITP, sickle cell, • Paediatric rashes – chicken pox, rubella, mumps, measles, HSP, slapped cheek • Syndromes- Down’s, Edwards, Patau’s, Turner’s, Klinefelter’s, • Neonatal- NEC, streptococcal sepsis, Pyloric stenosis, • NAI and differentials (Mongolian blue spots, osteogenesis imperfecta, scalded skin syndrome) • Emergencies- Anaphylaxis, Meningitis, Choking, DKA, • Immunisations and growth charts • Know how to take a basic structured history, structured examination, and formal developmental assessment.