Assessing Risk from Medical Radiation
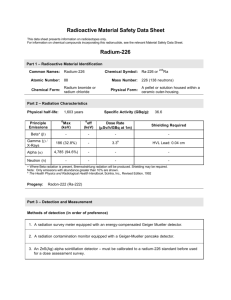
advertisement

Elizabeth H. Ey, M.D. Medical Director Radiology Dayton Children’s Medical Center Content of presentation and pictures courtesy of Thomas Slovis, M.D. and The Society for Pediatric Radiology Survey Has anyone here read a news report of radiation exposure from medical imaging? Survey Has anyone had a patient or family member ask them about radiation exposure from medical imaging? Survey Has anyone had a test question in medical education (or CME) regarding radiation exposure to patients from medical imaging tests? Questions What is our natural background level of radiation? What is the radiation dose of a 1 view chest radiograph? What is the radiation dose of a 1 view abdomen radiograph? What is the radiation dose of a CT scan? Head CT dose? Abdomen CT dose? Answers Natural occurring background radiation Chest, one view, child, skin dose Abdomen, one view, child, skin dose CT Head, child, minimal dose, CTDI CT Abd, child, CTDI 1 mrad/day 3-15 mrad 50 mrad 2000 mrad >1000 mrad What is the increased risk of death from cancer from 1 CT scan performed in a child? A B C The increased risk of cancer death from a CT scan is 0. The increased risk of cancer death is between 1 in 1000 to 1 in 5000 over a lifetime. The increased risk of cancer death is 1 in 1 million over a lifetime. Answer B It is estimated that an abdominal CT scan results in 1/1000 to 1/5000 excess risk of cancer at a later date. What is the current lifetime risk of developing cancer (US)? dying of cancer (US)? Lifetime risk of cancer (US) Developing Dying Male Female 44.05% 37.6% 23.24% 19.65% N Engl J Med 2007: 357:2277-84 USA Today Nov 29, 2007 USA Today Nov 29, 2007 Medical Radiation in Medicine When indicated it can diagnose illness Noninvasive, painless, fast, extremely accurate But like any medication or therapy Too much radiation can lead to deleterious effects DETERMINISTIC effect –linear, direct, ex: skin reddening Any radiation dose can cause lethal effect – cancer STOCHASTIC effect – non-linear, random, takes time to see Think of radiation as a medicine Effects are lifelong and cumulative Particularly severe effect in infants and children Especially when adult doses are used in children Age dependent – younger patient more severely effected No dose of radiation can be considered completely safe Linear non-threshold effect Oath of Hippocrates “Above all, do no harm.” ALARA Concept for Pediatric Radiation Dose As Low As Reasonably Achievable Medical Radiation in Children 1. History of Radiology 2. Basic dosimetry 3. Biology of radiation effects 4. Unique issues with radiation in children 5. Use of appropriate techniques 6. Joint efforts with healthcare providers History Dec 28, 1895: Roentgen submits manuscript describing his discovery of “x-ray” to the Physical Medical Society of Wurzburg: manuscript printed and distributed in 3 days Jan 9, 1896: manuscript appears in Vienna Press Jan 23, 1896: manuscript appears in Nature, in England Jan 23, 1896: Roentgen presented paper to Physical Medical Society of Wurzburg By mid 1896, fluoroscopy was in widespread practice From clinical bench to widespread use in 6 months Wurzburg Medical-Physics Society 1896 Dr. Kohler, famous anatomist, having hand X-rayed by Roentgen at the meeting. Level of Radiation Safety Circa 1896 First Pediatric Radiograph 14 minute exposure Roentgen received the first Nobel Prize in 1901 for his discovery Application of Radiation Sciences for Medical Diagnosis: Tremendous benefits Risks became evident with increasing use Side Effects of Radiation in Humans Started being reported within months of discovery of x-ray Public Spectacle: Side Effects Deep sunburn Hair loss Bloodshot eyes, vision impaired Transient effects Transient Hair Loss 40 min fluoro 18 inches from head Practitioners in X-ray techniques were the first to show the long term effects of radiation exposure Radiologist with Skin Carcinoma Monument to Martyrs in X-ray and Radium Physics – 1936 Hamburg Albers Schonberg Madame Curie Caldwell Codman Br J Radiol 2001; 74: 507- 519 Berrington A, Darby SC, Weiss HA, Doll R Research on 100 years of data on health of radiologists in Great Britain 1897-1954 – 41% excess of cancer deaths in practitioners of radiology 1954-1997 – zero excess mortality from cancer in the practitioners of radiology Learned biologic effects of radiation Applied what we learned to protect ourselves It worked But have we done enough? Have we protected our patients enough? 2. Basic dosimetry • Dose units • Measures of dose • Conversions Radiation Dose Units Methods of Measuring Radiation Dose Widely varied and difficult to compare Entrance skin dose Exit dose Dose area product (DAP) Organ dose –specific to radiosensitive organ Radiation output measured within a phantom CT dose index (CTDI) Dose equivalent Effective dose Radiation Dose Measurements Used for Risk Assessment Absorbed Dose – Gray or Gy (previous rad) Risk assessment for a specific organ or tissue Difficult to measure and not very useful Effective dose equivalent – Sievert or Sv (previous rem) Non-uniform exposure to organ or region Expression of risk equivalent to whole body exposure CT scanner dose units not useful CTDI vol and DLP determined by phantom Not helpful for assigning risk without conversion CTDI – CT Dose Index Reported on scanner consoles Based on phantom (16 or 32 cm diameter) Only represents the dose to the phantom based on CT parameters selected Does not indicate dose to the child in the CT scanner Conversions of CTDI to effective dose are only rough estimations for children e.g. no age based chest modifications Dose Chart 1 Gy = 100 rads = 1 Sv 10 mGy = 1 rad = 10 mSv 0.01 mGy = 1 mrad = 0.01 mSv Effective Dose It is a radiation dose quantity It is a computation based on: Organ dose and radiosensitivity Weighting factors It is not a risk number Huda, W Pediatric Radiology 2002: 32; 272-279 3. Biology of radiation effects Types of Biological Effects from Radiation Deterministic effects Stochastic effects Deterministic Effect • Seen with high radiation dose • Severity of effect is dose dependent: • There is a threshold below which dose the effect is NOT seen. • Examples: skin burns, hair loss Deterministic Effects AJR July 2001 - Skin burns from cardiac interventional procedures Stochastic Effect Low dose, random effect Non dose dependent: •Risk of the effect is dose dependent but the severity of the effect is not. •Example: Risk of cancer increases with increasing dose but the severity of the type of cancer is not dose dependent •There is “no threshold” to this effect Stochastic Effect Means all or none (random effect) Not based on a particular dose But with higher radiation absorbed dose, the higher the likelihood of genetic damage Mostly concerned with risk of carcinogenesis Incidence – twice the mortality risk Mortality - risks that are quoted here Biological effects of radiation damage to DNA •Reactions are rapid •Induction of cancer takes many years •The damage to DNA may lead to genomic instability Genomic Instability “Persistent enhancement in the rate of which genetic change arises in the descendents …..” Little Stochastic Effect (Random) on Irradiated Stem Cells C. and D. are the effects seen in reality The irradiated cell transmits the genetic defect randomly into future cell generations Cancer may not be seen for several cell generations Little JB: Ionizing Radiation in Cancer in Medicine 2003 4. Unique issues with radiation exposure to children Children are smaller and have more radiation sensitive tissue Have a longer life expectancy in which to express the damaging effect of radiation Is there a threshold for low dose radiation in which no effect will be seen? Debated Breast Cancer and Scoliosis Films Doody et al. Spine 25:2052- 2063 year 2000 Thyroid Cancer after Childhood Radiotherapy Ron, E Pediatric Radiology 2002 32: 232- 237 Infant Radiotherapy for “Enlarged Thymus” … 96 minutes of x rays Fetal Exposure Oxford Study of Childhood Cancer Obituary in New York Times 2002 Cancer risk in fetuses exposed in 3rd trimester The excessive risk is 47% in the fetuses irradiated. Atomic Bomb Survivor Follow Up Pierce and Preston 2000 Original 84,000 survivors followed for 55 years Eventually had 50,000 survivors that were followed (1988-1994) Increased cancer rate even at low dose (0.05-0.15 Sv or 500 mrad-1.5 rad) Excessive cancer deaths were demonstrated Pierce et al; Rad Res 154 pg 183: 2000 .... = cancer death rate for at-risk population (A bomb survivors) __ = cancer death rate otherwise expected Straight lines represent two different starting points to guess at which point radiation dose is a problem. One begins at zero and the other at 0.06 Sv. Is there a safe dose? Linear non-threshold (NLT) dose Dose below which there is no risk of carcinogenesis? NCRP Report – cannot prove safety of any radiation dose Linear No-threshold Principle “There is no need to even consider a linear no-threshold principle when we have direct human evidence of carcinogenesis at doses of <10mSv.” Pierce DA, Preston DL 2000; 154:178-186 Linear No-threshold Principle LNT is NOT the issue! “Other populations” have not had 50 years of meticulous research to detect cancer Sample size – 84,000 people at start of study Age at exposure was known from the start Length of follow-up – over 55 years of f/u AJR Feb 2001 Brenner et al AJR Feb 2001 Typical Radiation Doses (mSv) • Average annual technologist dose 3.2 • Natural annual background 3.5 0.09 8.75 • Dental x-rays BE (marrow) • CXR (marrow) • Mammogram (breast) • Airline passenger • Flight crew / attendants annual • CT 0.01 0.5 - 7.0 0.03 1.6 < 1.0 – 30 mSv CT radiation doses can overlap radiation exposure doses calculated for survivors of the A-bomb. Pierce, Preston; Rad Res, 2000; 151 pg 178-186 Brenner; Pediatric Radiology, Apr 2002; pg 230 Brenner et al 2003 “Above doses of 50-100 mSv (protracted exposure) or 10-50 mSv (acute exposure), direct epidemiologic evidence from human populations demonstrate the exposure to ionizing radiation increases the risk of some cancer.” www.pnas.org/cgi/doi/10.1073/pnas.2235592100 AJR Feb 2001 CT Use in the US Increased dramatically in the recent years Estimated that 11% of all CT scans performed in the US are performed in children There is a risk of cancer death from CT radiation dose The younger the patient, the greater the risk N Engl J Med Nov 2007 Brenner and Hall Infants are 10-15 times more vulnerable than middle age adults Brenner et al; Pediatric Radiology, Apr 2002: pg 230 Females are at higher risk. Age at exposure is the most important factor. Hall Pediatric Radiology Apr 2002 pg 226 Important Concepts Greatest effect is on actively growing cells Infant, fetus Cumulative dose, life long effect EDE – Effective Dose Equivalent For the same dose, a child is much more vulnerable because of the way the dose is calculated. When measuring the dose at the midpoint of an adult phantom (32 cm), the beam has already passed completely through the child. Consider the Premature Infant Hepatoblastoma Occurs at a higher rate in premature infants (40%) Infants studied by Alicia Stewart were term infants Our premature infants can now survive at 23-24 weeks gestation The premature infant is at much higher risk to radiation exposure. 5. Use of Appropriate Technique Film screen radiography - using more radiation exposure than needed results in a black image Digital and computed radiography with post-processing – can make almost any overexposed image look diagnostic by manipulating contrast and brightness Shunt Survey Can’t tell technique just by looking at it Dose parameters should be included whenever possible Uncoupling end result from information regarding dose is a dangerous practice When the exam does not include the technique parameters used to acquire the images, The amount of radiation used may be more than needed. Assessing Risk CT related cancer death 1000-5000/million in a life time (not per year) Radiation dose 100-600 times less than CT dose 6. Joint Efforts of Health Care Workers What can be done? What resources are available? We are all responsible Practitioner who orders CT Radiologist who determines CT protocol CT technologist that performs the CT scan How do we respond? Be sure that an imaging test is necessary Use the least invasive modality which gives a high likelihood of correct diagnosis Consider all the options for imaging MR and US use NO radiation Discuss the case with a pediatric radiologist if uncertain which modality to use When CT is used appropriately It saves lives Fast, accurate, comprehensive Especially useful for trauma patients or emergency conditions It has the greatest detail in imaging Sub mm resolution (IAC), high resolution lung detail It is less sensitive to patient motion than MR It is less sensitive to gas than US It creates a volume of data which permits multiplanar reconstruction as well as 3D surface rendering How do we respond? Understand the radiation doses associated with various imaging modalities Order imaging tests on basis of medical indications, not because of parental/legal/insurance pressure Discuss problem cases with radiologist, engage their expertise Inform parents/patients of radiation risk www.ImageGently.com What is the best (most appropriate) imaging exam? What are the alternatives? First febrile seizure First non-febrile seizure Headaches RLQ abdominal pain Acute flank pain with hematuria Unusual head shape Evaluate vascular ring Image Gently One size does not fit all... There's no question: CT helps us save kids' lives. But, when we image, radiation matters! Children are more sensitive to radiation. What we do now lasts their lifetimes. So, when we image, let's image gently: More is often not better. Image Gently When CT is the right thing to do: Child size the kVp and mA One scan (single phase) is often enough Get as much information as possible from the single phase (IV contrast, enteric contrast) Scan only the indicated area ALARA As Low As Reasonably Achievable Their future is in our hands. Questions?