Importance of Graduate Education
advertisement

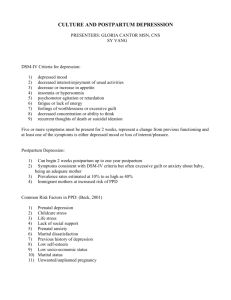
The Influence of Culture on the Development and Detection of Postpartum Depression Cindy-Lee Dennis, RN, PhD Assistant Professor, Faculty of Nursing CIHR New Investigator Career Scientist, Ontario Ministry of Health What are immigrant mothers at increased risk for postpartum depression? Why does postpartum depression often remain undetected? What is screening? What tools can health professionals use to detect postpartum depression? Recommendations for detecting depressive Symptoms Dr.Cindy-Lee Dennis Childbirth represents for women a time of great vulnerability to become mentally unwell, with postpartum mood disorders representing the most frequent form of maternal morbidity following delivery Dr.Cindy-Lee Dennis These affective disorders following childbirth range in severity from the early maternity blues to postpartum psychosis, a serious state affecting less than 1% of mothers Dr.Cindy-Lee Dennis Dr.Cindy-Lee Dennis Within this group of disorders is postpartum depression, a condition often exhibiting the disabling symptoms of dysphoria, emotional lability, insomnia, confusion, anxiety, guilt, and suicidal ideation. Frequently exacerbating these indicators are low self-esteem, inability to cope, feelings of incompetence, and loneliness. Dr.Cindy-Lee Dennis The inception rate is greatest in the first 12 weeks postpartum with duration frequently dependent on severity and time to onset of treatment Postpartum depression is a major public health issue for many women from diverse cultures Dr.Cindy-Lee Dennis Longitudinal and epidemiological studies have yielded varying prevalence rates, ranging from 3% to more than 25% of women in the first year following delivery These rates fluctuate due to sampling, timing of assessment, differing diagnostic criteria, and whether the studies were retrospective or prospective (6- to 10-fold higher) Dr.Cindy-Lee Dennis A meta-analysis of 59 studies reported an overall prevalence of postpartum depression to be 13% It is noteworthy that the absolute difference in estimates between self-report assessments and diagnostic interviews was small Risk Factors (Beck, 2001) Dr.Cindy-Lee Dennis Prenatal depression Childcare stress Life stress Lack of social support Prenatal anxiety Maternity blues Marital dissatisfaction Previous history of depression Low self-esteem Low socio-economic status Marital status Unwanted/unplanned pregnancy However, preliminary research suggests that immigrant mothers from diverse cultures may be at higher risk to develop postpartum depression Dr.Cindy-Lee Dennis Postdoctoral Research Fellowship Dr.Cindy-Lee Dennis UBC, Faculty of Medicine, Dept. Health Care & Epidemiology Population-based study - 645 mothers completed questionnaires at 1, 4, and 8 weeks postpartum Edinburgh Postnatal Depression Scale (EPDS) Dr.Cindy-Lee Dennis 10-item self-report instrument Designed specifically to assess depressive symptoms in new mothers Cut-off >12 = confirm postpartum depression Cut-off > 9 = community-based screening Translated into diverse languages Sample Characteristics Dr.Cindy-Lee Dennis Mean age was 28.5 years (SD = 5.0) 89% Caucasian 90% married or common-law 39% high school or less, 38% college/trade education, 21% university degree Income: 36% < $30,000, 31% > $80,000 44% primiparous 74% vaginal delivery 69% discharged home within 48 hours Question Who is at risk for depressive symptoms in the immediate postpartum period? Dr.Cindy-Lee Dennis A multifactorial predictive model was developed using sequential logistic regression analysis The outcome was an EPDS score > 9 at 1-week postpartum Socio-Demographic Factors 1. 2. 3. 4. 5. 6. 7. Dr.Cindy-Lee Dennis 8. 9. Marital status Age Education Ethnicity Immigration during the last five years Household income Ability to manage with income Access to transportation Suitable housing Biological/Psychological Factors Dr.Cindy-Lee Dennis 1. Vulnerable personality 2. Self-Esteem 3. Premenstrual symptoms 4. Maternal psychiatric history 5. Family psychiatric history 6. History of postpartum depression Pregnancy Factors Dr.Cindy-Lee Dennis 1. Infertility problems 2. Planned pregnancy 3. Mother’s feelings about pregnancy 4. Partner’s feelings about pregnancy 5. Pregnancy complications Life Stressors Dr.Cindy-Lee Dennis 1. Life events (past 12 months) 2. Job stress 3. Worrying about returning to work 4. Satisfaction with job Substance Abuse and Violence 1. 2. 3. 4. 5. Dr.Cindy-Lee Dennis 6. Use of alcohol and drugs by the mother or her partner History of physical or sexual abuse Fear of partner History of physical abuse as a child Physical abuse directed towards the subject’s mother by her father Interaction with child protection services Social Support Dr.Cindy-Lee Dennis 1. Global Support 2. Relationship-Specific Support from: – Partner – Mother – Mother-in-law – Other women with children Obstetrical Factors Dr.Cindy-Lee Dennis 1. Induction of labour 2. Mode of delivery 3. Satisfied with pain management 4. Control during labour 5. Labour complications Maternal Adjustment Dr.Cindy-Lee Dennis 1. Ready for hospital discharge 2. Infant feeding method 3. Satisfaction with infant feeding method Dr.Cindy-Lee Dennis In the multivariate analysis, significant variables were tested and retained in the model if the pvalue for the beta-estimate was 0.05 or less Variables were entered into the model in the following chronological order: sociodemographic, biological/psychological, pregnancy, life stressors, substance abuse/violence, social support, obstetric, and maternal adjustment. Risk Factor Dr.Cindy-Lee Dennis Beta OR 95% CI Immigrated within last five years History of depression before pregnancy Vulnerable personality 1.60 4.94 1.00-24.8 0.60 1.82 1.05-3.16 0.20 1.21 1.13-1.31 Life stressors 0.12 1.12 1.01-1.24 Pregnancy-induced hypertension Global support 1.28 3.62 1.05-9.74 -.04 0.96 0.93-0.99 Satisfaction with infant feeding method Ready for hospital discharged .83 2.29 1.13-4.64 1.33 3.78 1.40-10.19 Dr.Cindy-Lee Dennis Dennis, C-L., Janssen, P., & Singer, J. (2004). Identifying Women At-Risk for Postpartum Depression in the Immediate Postpartum Period: Development of a Multifactorial Predictive Model. Acta Psychiatrica Scandinavica, 110, 338-346 Among the few studies that have examined immigration, most have also found this variable to be a significant factor 1. Danaci, A. E., Dinc, G., Deveci, A., Sen, F. S., & Icelli, I. (2002). Postnatal depression in turkey: epidemiological and cultural aspects. Social Psychiatry & Psychiatric Epidemiology, 37(3), 125-129. 2. Dankner, R., Goldberg, R. P., Fisch, R. Z., & Crum, R. M. (2000). Cultural elements of postpartum depression. A study of 327 Jewish Jerusalem women. Journal of Reproductive Medicine, 45(2), 97-104. 3. Glasser, S., Barell, V., Shoham, A., Ziv, A., Boyko, V., Lusky, A., et al. (1998). Prospective study of postpartum depression in an Israeli cohort: prevalence, incidence and demographic risk factors. Journal of Psychosomatic Obstetrics & Gynecology, 19(3), 155-164. 4. Zelkowitz, P., & Milet, T. H. (1995). Screening for post-partum depression in a community sample. Canadian Journal of Psychiatry, 40(2), 80-86. Dr.Cindy-Lee Dennis Unfortunately, scant research has been conducted as to why these women are at-risk postpartum depression Dr.Cindy-Lee Dennis Why are immigrant women at risk for PPD? Dr.Cindy-Lee Dennis Investigations with general non-postpartum immigrant populations have clearly demonstrated a link between the acculturation process and psychological problems When individuals interface with a new host society, they confront many challenges, including adjusting to a new language, different customs and norms for social interactions, unfamiliar rules and laws, and in some cases extreme lifestyle changes (e.g., rural to urban) Dr.Cindy-Lee Dennis Acculturation refers to the process of adjusting to these life modifications, and depending on the disparity between the two cultures, acculturative stress is a common outcome resulting frequently in an increased risk for depression Dr.Cindy-Lee Dennis While considerable attention has been paid to the importance of acculturative stress on depression among non-postpartum immigrant populations and stressful life events on maternal mood, the relationship between acculturative stress and postpartum depression has not been explored Dr.Cindy-Lee Dennis Dr.Cindy-Lee Dennis Research also suggests factors may have a protective effect on acculturative stress, including the provision of social support and socio-economic status This is particularly salient for postpartum depression, given that studies clearly suggest social deficiencies increase the risk of postpartum depression Dr.Cindy-Lee Dennis In addition to enhancing social support, another factor that may have a protective effect on the development of postpartum depression is traditional postpartum rituals For example, in many cultures special practices and customs serve to impose structure and meaning in the perinatal period and promote the successful transition to motherhood (Stuchbery, Matthey, & Barnett, 1998) These postpartum rituals have been examined in varying degrees among many cultures (e.g., Arabic, Chinese, Japanese, Malaysian, Taiwanese, Thai, etc. ) and frequently last between 30 to 40 days Dr.Cindy-Lee Dennis While several studies provide evidence that traditional postpartum rituals are followed by the majority of women in their native country, limited research has been conducted related to the practice of these rituals post-migration Dr.Cindy-Lee Dennis Current Research Initiative Systematic Review of Traditional Postpartum Practices Dr.Cindy-Lee Dennis Dr. Cindy-Lee Dennis Dr. Lori Ross Dr. Sarah Romans Dr. Gail Robinson Dr. Ken Fung Traditional postpartum rituals among indigenous/native mothers (including rationale for practices): 1. 2. 3. 4. Dr.Cindy-Lee Dennis 5. 6. organized support (includes who, where, what activities, etc.) dietary practices restricted physical activities hygiene practices celebrations (e.g., naming baby) other rituals Example Among chinese mothers the traditional rite of “Tso-Yueh-Tzu”, translated as ‘doing the month’, is concerned with beliefs and practices associated with the postpartum period When doing the month, women are required to stay indoors and to follow specific dietary, hygiene, and physical activity restrictions for 4 weeks to promote recuperation Additionally, someone (usually a female family member) assumes most of the infant care and household responsibilities Dr.Cindy-Lee Dennis This traditional practice has been investigated in a number of studies and all suggest that many Chinese women still follow the practice and believe that it will improve their health (Cheung, 1997; Davis, 2001; Holroyd, Katie, Chun, & Ha, 1997; Lee et al., 1998) Dr.Cindy-Lee Dennis However, resent research studying Hong Kong mothers found environmental constraints and difficulties in following the proscriptions of the traditional practices and questioned how women could adapt the ritual to fit with modern life (Leung, Arthur, & Martinson, 2005) Dr.Cindy-Lee Dennis Similarly, one Australian study found that 18% of immigrant Chinese mothers felt ambivalent about traditional practices and that the reason they followed the practice was to please their inlaws (Matthey, Panasetis, & Barnett, 2002) Furthermore, two studies suggest adherence to these traditional practices among native and immigrant Chinese mothers may not be protective against the onset of PPD (Leung, Arthur, & Martinson, 2005; Matthey, Panasetis, & Barnett, 2002) Dr.Cindy-Lee Dennis While there are many variables involved in the practice of ‘doing the month’ that may have potential health benefits, research suggests that one salutary aspect may be the provision of organized support and that PPD may be prevented However, it is unknown whether it indeed does have a potential protective effect or whether these rituals simply delay the development of PPD, as preliminary research with Hong Kong Chinese women suggests Postpartum Practices and Depression Prevalences: Technocentric and Ethnokinship Cultural Perspectives Dr.Cindy-Lee Dennis Posmontier, B., & Horowitz, J. A. (2004). Postpartum practices and depression prevalences: technocentric and ethnokinship cultural perspectives. Journal of Transcultural Nursing, 15(1), 34-43. Technocentric Dr.Cindy-Lee Dennis Cultures which use technology to monitor new mothers The infant is the primary focus in the immediate postpartum period Potential danger 24-48 hours Maternal-infant separation Mother discharged home to a social system that does not have formalized traditions or norms Technology is valued over social networks Canada, US, UK, Western Europe, Australia Ethnokinship Dr.Cindy-Lee Dennis Cultures in which the performance of social support rituals by family networks are the primary focus in the immediate and later postpartum period While advanced technology is used to promote safe and optimum postpartum outcomes the family social supports retains primary importance Korean, Chinese, Japanese, Hmong, Mexican, African, Arabic, Amish Dr.Cindy-Lee Dennis Postpartum support structures Mandated rest and assistance with household tasks Maternal vulnerability Social seclusion Recognition of role transition Cultural PPD Risk Factors Dr.Cindy-Lee Dennis Acculturative stress Traditional postpartum practices Why does postpartum depression often remain undetected? Dr.Cindy-Lee Dennis The lack of detection is not just a health professional issue that can be dealt with by just screening Women do not proactively seek help Dennis, C-L., & Chung-Lee, L. (submitted). A review of postpartum depression help-seeking behaviours and treatment preferences. Birth. Maternal Barriers Dr.Cindy-Lee Dennis Reluctant to obtain professional assistance Unwilling to disclose emotional problems especially depression Popular myth equates motherhood with happiness Dr.Cindy-Lee Dennis Do not know where to obtain assistance Unaware of treatment options Perceive health professional role to address physical symptoms not emotional problems Somatization - women translate emotional distress into physical symptoms Dr.Cindy-Lee Dennis Lack knowledge about PPD Not aware they are suffering from the condition Deny and minimize symptoms Difficulty understanding the problems they are experiencing – assume struggles are normal for mothers – reasonable response to adversity Dr.Cindy-Lee Dennis Conversely, some women recognize depression but fear: – having child taken aware – being labelled mentally ill – not fulfilling role as mother – obtaining a more serious mental diagnosis Dr.Cindy-Lee Dennis Also, depression implies weakness or perceived failure Family members may discourage help seeking – in some cultures it is unacceptable to admit to depressive symptoms Some family member lack knowledge about PPD Health Professional Barriers Dr.Cindy-Lee Dennis Limited training in the assessment and management of PPD Feel uncertain about how to effectively assist therefore reluctant to raise such issues Normalize symptoms and dismiss as selflimiting Mothers obtaining professional assistance felt disappointment, frustration, humiliation, and anger Dr.Cindy-Lee Dennis Patronizing attitudes – increased feelings of worthlessness and guilt in inability to cope Dr.Cindy-Lee Dennis Insufficient time in consultations Prefer to prescribe medication that alleviated symptoms but reinforced feelings of inadequacy Not referred to secondary services Language barriers Health Service Utilization Dr.Cindy-Lee Dennis Culture constitutes an important context for affective conditions as shared beliefs, attitudes, and norms for emotional responses influences how mothers experience depression Culture also determines help-seeking behaviours and health service utilization Dr.Cindy-Lee Dennis It is well documented that in Canada, ethnic minorities are less likely than Caucasians to seek mental health treatment and they often delay treatment until symptoms are more severe They are also less likely to seek treatment from mental health specialists, instead turning more often to primary care or informal sources such as clergy, traditional healers, and family and friends While health professionals increasingly emphasize the need for cultural competence and the problem of health service barriers and utilization inequities, no research has been conducted with immigrant women related to specific postpartum depression help-seeking barriers and health service utilization Dr.Cindy-Lee Dennis Clinical Implications: Strategies For Caring For Mothers From Different Cultures Dr.Cindy-Lee Dennis Dr.Cindy-Lee Dennis Education about PPD is important for women as it could enable earlier recognition and helpseeking Information about services and health professional’s roles may be particularly effective in specific cultural groups if it were aimed at family members as well as the mothers Educational programs could be conducted across the perinatal period with a focus on assisting the family in understanding the stresses related to motherhood and identifying specific strategies to help the mother cope with these challenges Dr.Cindy-Lee Dennis Understanding of the different ways in which mothers conceptualize, explain, and report symptoms of depression The term ‘postpartum depression’ may not be acceptable to many mothers and an alternative approach to recognition and management may be required This may involve the use of symptom and context-based terms such as tension, weakness, and difficulties in one’s relationship at home Dr.Cindy-Lee Dennis Health professionals should also be aware of traditional postpartum practices and understand the rationale behind such practices Meaning of traditional practices to the mother Preliminary research suggests that devaluing traditional practices based on a woman’s cultural group could mean devaluing the mother as a person Treatment Preferences Pharmacological Interventions Dr.Cindy-Lee Dennis Women are often reluctant to take antidepressant medication even after receiving education Fear of addiction Potential side-effects or harm related to longterm use Concerns influenced medication compliance Opportunity to Talk about Feelings Women want: 1. to be given permission to talk in-depth about their feelings, including ambivalent and difficult feelings 2. to talk with a non-judgmental person who will spend time listening to them, take them seriously, and understand and accept them for who they are 3. recognition that there is a problem and reassurance that other mothers experience similar feelings and that they will get better Dr.Cindy-Lee Dennis Provision of Peer Support Dr.Cindy-Lee Dennis The ways in which individual women interpreted, negotiated, and experienced social norms of motherhood depends in part on their interpersonal relationships with other mothers Support from other women with children was perceived as particularly important for recovery Among immigrant and ethnic minority women: Dr.Cindy-Lee Dennis Support groups facilitated activities such as shopping and learning English In a phenomenological study with Middle Eastern women living in Australia, ‘Arabic community centers’ provided immigrant women with diverse activities, such as sewing and cooking, that were aimed at relieving their stress by taking them out of their houses and enabling them to interact with other women (Nahas , 1999) Dr.Cindy-Lee Dennis Depressed mothers using these centers reported that they could cope much better when they returned home to meet their husband and resume their traditional roles Similar results with immigrant mothers living in the UK (Templeton , 2003) Women attending a group felt it was a break from housework and childcare responsibilities and that it allowed them to relax and meet people Meaning of Care Dr.Cindy-Lee Dennis US Mothers In a phenomenological study involving US mothers, seven themes emerged that illustrated nurses' caring for mothers experiencing postpartum depression and promoted satisfaction with care received (Beck) Dr.Cindy-Lee Dennis 1. 2. 3. 4. 5. 6. Dr.Cindy-Lee Dennis 7. Having sufficient knowledge about postpartum depression Using astute observation and intuition to make quick, correct diagnoses Providing hope that the mothers' depression will come to an end Readily sharing their time Making appropriate referrals for the right path to recovery Providing continuity of care Understanding what the mothers were experiencing Jordanian Mothers In a qualitative study of 22 Jordanian women living in Australia who had suffered from postpartum depression, three themes focusing on the meaning of care were discussed (Nahas , 1999) Dr.Cindy-Lee Dennis Dr.Cindy-Lee Dennis 1. Care meant strong family support and kinship during the postpartum period 2. Care included preservation of Jordanian childbearing customs as expressed in the celebration of the birth of the baby 3. Care was being allowed to fulfilling traditional gender roles as mother and wife Dr.Cindy-Lee Dennis Health professionals facilitating treatment services should address these issues and ensure that interpreters are available for those women who do not speak or understand English Health professionals need to recognize and take into account mothers’ own explanations of their problem and their ideas concerning what might constitute an appropriate treatment Improve detection and treatment of PPD Dr.Cindy-Lee Dennis Be aware of acculturative stress Acknowledge traditional postpartum rituals Address barriers to seeking help Provide culturally sensitive treatment based on maternal perceptions What is Screening? Screening Dr.Cindy-Lee Dennis A systematic use of tools or procedures applied to a defined population (e.g., new mothers) Purpose is to detect an unrecognized disorder or condition in individuals who do not yet perceive that they are at risk of, or suspect that they are affected by, a condition or its complications Dr.Cindy-Lee Dennis Screening tools do not diagnose a condition Only identifies individuals who are: – at risk of developing the condition – are displaying potential symptoms of the condition In the case of PPD, health professionals could use screening procedures to identify women with depressive symptoms who may require additional intervention Screening has the potential to improve the quality of life through early diagnosis of a serious condition Screening is not perfect – false positive – false negative Dr.Cindy-Lee Dennis individuals wrongly reported to have the condition individuals wrongly reported as not having the condition What tools can health professionals use to detect postpartum depression? Dr.Cindy-Lee Dennis The diagnosis of PPD can only be accomplished through the application of diagnostic criteria such as the popular and progressively evolving Diagnostic and Statistical Manual [e.g., DSMIV] Measures used to assess for depressive symptoms include standardized interviews and self-report questionnaires Self-Report Dr.Cindy-Lee Dennis The most common and clinically useful way to screen - administer a self-report questionnaire Women rate the frequency or severity of their own depressive symptoms Edinburgh Postnatal Depression Scale (EPDS) The most widely used instrument to assess for PPD and identify high-risk mothers Advantage It has been translated into various languages and tested in samples from a variety of countries Disadvantage Most investigations involve Caucasian or homogenous samples in native countries Dr.Cindy-Lee Dennis Few studies have psychometrically assessed the EPDS using clinical diagnostic interviews among recently immigrated women Accurate Assessment and Detection While screening procedures may significantly assist in the detection of PPD, these tasks are complicated when assessing women from different cultural groups Dr.Cindy-Lee Dennis For example, somatization may be a prominent expression of depression among Asian and African cultures, while complaints of sadness and feelings of guilt are more characteristic of depression in Western cultures Dr.Cindy-Lee Dennis Unresolved problems related to appropriate cutoff scores for specific ethnic groups For example, while a cut-off score of 12/13 has been repeatedly validated and recommended for detecting PPD and 9/10 for community based screening, validation studies have highlighted that scores from translated versions should be interpreted cautiously as different cut-off points have been suggested Dr.Cindy-Lee Dennis In particular, Lee et al. recommended a cut-off of 9/10 was most appropriate at 6 weeks postpartum for detecting PPD in a Hong Kong population Okano et al. reported that a cut-off of 8/9 was suitable for screening Japanese mothers In an Australian study of Vietnamese and Arabic mothers, fewer Vietnamese mothers met the criteria for depression However, detailed comparisons between EPDS and Diagnostic Interview Schedule (a diagnostic measure) questions suggested that these lower rates were possibly due to the social undesirability of verbally reporting negative emotions and a cut-off of 9/10 was suggested for Vietnamese women Dr.Cindy-Lee Dennis Similar response patterns were found by Lee in their Hong Kong study It is possible that these Chinese women, like their Vietnamese counterparts, were reluctant to concede unhappiness or distress in the early postpartum period to an interviewer However, the women seemed less constrained in responding to a self-report questionnaire Dr.Cindy-Lee Dennis In contrast, Yoshida found similar depression rates in Japanese women residing in England and Japan using a clinical diagnostic interview However, depression was not detected when the translated EPDS was used as a screening instrument In particular, a 12/13 cut-off resulted in a sensitivity of zero, rendering the researchers to conclude that Japanese women may be reluctant to disclose depressive symptoms via a self-report measure They also commented that the difference might be due to the exclusion of somatic symptoms in the EPDS since Japanese women tend to refer to physical problems and concerns about their infant rather than expressing feelings of low mood directly These results suggest that if health professionals are to implement accurate yet culturally-appropriate screening procedures, additional research is required among diverse cultural groups to determine: 1. PPD prevalence rates Patterns of inception EPDS accuracy 2. 3. Dr.Cindy-Lee Dennis A Few Points to Consider When Using the EPDS Dr.Cindy-Lee Dennis Some researchers and clinicians have identified common misperceptions about how to use and interpret PPD screening tools “A score below a cut-off confirms that the mother has no mental health disorder.” Dr.Cindy-Lee Dennis Using the EPDS, it is unlikely that a mother scoring below 10 has clinically significant levels of depression However, it is possible, particularly when the tool is administered to multicultural populations Furthermore, health professionals need to recognize that a low score on the EPDS does not rule out symptoms of other mental health conditions or problems of concern (e.g., anxiety disorders or psychosis) “The screening tool makes the decision to treat, so a score above the cut-off point means a referral to a service provider.” An EPDS score is only one factor to consider when deciding on whether or not to initiate treatment and preventive strategies Clinical judgment also plays a critical role Dr.Cindy-Lee Dennis Finally, it is important that the decision be a collaborative one between the mother and her health professional When would be the most effective time to screen for postpartum depression? Antenatal Screening Dr.Cindy-Lee Dennis An excellent systematic review (Austin & Lumley, 2003) summarized 16 studies that included antenatal screening No screening instrument met the criteria for routine application in the antenatal period The unacceptably low positive predictive values in all these studies make it difficult to recommend the use of screening tools in routine antenatal care However, approximately 12% of women are depressed during pregnancy, and the EPDS can detect depressive symptoms antenatally Therefore, when the health care system criteria described are met, a health unit or organization might decide to use the EPDS to identify pregnant women for current depression, so that these women receive treatment as soon as possible Dr.Cindy-Lee Dennis So long as the goal is to detect current rather than future depression, the EPDS can be useful during the antenatal period Postnatal Screening Dr.Cindy-Lee Dennis Traditionally, experts have proposed that screening tools be administered between 6 to 8 weeks postpartum The rationale for waiting to screen until 6 weeks postpartum is that the maternity blues will have resolved by this time Screening earlier in the postpartum period might result in a high false positive rate Dr.Cindy-Lee Dennis In the Canadian health care system, a benefit of screening at approximately 6 weeks postpartum is that most women will attend a follow-up appointment with their obstetrical health professional around this time, and therefore may be relatively easy to access Immediate Postpartum Period Dr.Cindy-Lee Dennis More recently, some researchers have suggested that even despite the high false positive rate, screening during the immediate postpartum period (i.e., the first 2 weeks postpartum) may be preferred to waiting until 6 to 8 weeks postpartum Strong research evidence suggests that low maternal mood in the immediate postpartum period is highly predictive of the development of PPD Disadvantage Dr.Cindy-Lee Dennis A significant proportion of the women who screen positive for depression at 1 to 2 weeks postpartum may not meet diagnostic criteria for depression Women who do not actually require treatment for PPD might consume substantial resources Two-Stage Screening Dr.Cindy-Lee Dennis Where resources permit, a two-stage screening process, in which mothers who score positive during the first screening assessment are readminister the EPDS again later, may be the most effective way to implement a screening program Research has not determined exactly how much later to administer the screening tool again RNAO Best Practice Guideline Development Panel Members Cindy-Lee Dennis (Team Leader) Stephanie Lappan-Gracon (Program Coordinator) Dr.Cindy-Lee Dennis Sue Bookey-Bassett Barbara Bowles Marilyn Evans JoAnne Hunter Karen McQueen Lori Ross Sharon Thompson Bonnie Wooten Donna Bottomley Judi De Boeck Denise Hebert Elizabeth McGoarty Phyllis Montgomery Marcia Starkman Ulla Wise Purpose and Scope Dr.Cindy-Lee Dennis Confirmation, prevention and treatment of mothers with depressive symptoms in the first postpartum year Recommendations for Detecting Depressive Symptoms (application to mothers from different cultures) Dr.Cindy-Lee Dennis Dr.Cindy-Lee Dennis EPDS is the recommended self-report tool to confirm depressive symptoms in postpartum mothers The EPDS can be administered anytime throughout the postpartum period (birth to 12 months) to confirm depressive symptoms Dr.Cindy-Lee Dennis Encourage mothers to complete the EPDS by themselves in privacy Dr.Cindy-Lee Dennis An EPDS cut-off score greater than 12 may be used to determine depressive symptoms among English-speaking women in the postpartum period. This cut-off criterion should be interpreted cautiously with mothers who (1) are non-English speaking, (2) use English as a second language, and/or (3) from diverse cultures Dr.Cindy-Lee Dennis The EPDS must be interpreted in combination with clinical judgment to confirm mothers with depressive symptoms Dr.Cindy-Lee Dennis Provide immediate assessment for self harm ideation/behaviour when a mother scores positive (e.g from 1 to 3) on the EPDS self harm item number 10 Many unanswered questions remain Dr.Cindy-Lee Dennis New Mothers in a New Country Understanding Postpartum Depression among Recent Immigrant and Canadian-Born Chinese Women Principal Investigator: Dr. C-L Dennis Dr.Cindy-Lee Dennis Research Objectives Dr.Cindy-Lee Dennis 1. To determine the prevalence of postpartum depression (PPD), patterns of inception, and psychometric properties of the Edinburgh Postnatal Depression Scale (EPDS) among recent immigrant Chinese mothers 2. To examine the relationships between recent immigrant status, PPD, acculturation, acculturative stress, social support, income, and the practice of traditional postpartum rituals 3. Dr.Cindy-Lee Dennis To determine patterns of PPD help-seeking behaviours and barriers to health services among recent immigrant Chinese mothers Study Design Dr.Cindy-Lee Dennis A longitudinal design where recently immigrated Chinese mothers will be followed for the first year postpartum A Canadian-born cohort of Chinese mothers will also be followed as a control group for comparisons Following a comprehensive recruitment plan, a research assistant (matched on maternal language ability) via telephone will provide all potentially eligible women with a detailed study explanation and ensure eligibility Dr.Cindy-Lee Dennis Participating mothers will complete baseline information within 4 weeks postpartum All mothers will be followed–up at 12, 24 and 52 weeks postpartum via telephone by trained research assistants The study results will make substantive contributions in seven areas: Dr.Cindy-Lee Dennis 1. Provide information about PPD prevalence and inception rates among recently immigrated and Canadian-born Chinese women 2. Establish the sensitivity and specificity of the Edinburgh Postnatal Depression Scale (the most widely-used international measure to assess depressive symptoms in postpartum women) in detecting PPD among these Chinese mothers 3. Advance our understanding of the relationship between recent immigrant status, the acculturation process, and PPD Dr.Cindy-Lee Dennis 4. Determine which traditional postpartum rituals are maintained post-migration and the effect of these practices on the development of PPD 5. Investigate health service utilization barriers and help-seeking behaviours related to PPD 6. Promote cultural sensitivity among health professionals 7. Guide the development of a randomized controlled trial to evaluate a culturally-sensitive PPD intervention Postpartum Depression Peer Support Trial RCT to evaluate the effect of telephone-based peer (mother-to-mother) support on the prevention of PPD among high-risk mothers Screening for high-risk mothers across the province – – Dr.Cindy-Lee Dennis – – Peel Halton York Toronto - Windsor - Ottawa - Sudbury Relevance for Screening Dr.Cindy-Lee Dennis PPD prevalence rates for a multicultural population Accuracy of screening for PPD at 1 week postpartum Maternal acceptance to screening Inability to screen due to language barriers Cost of screening for PPD Referral of mothers with clinical depression at 12 weeks postpartum Reassessment of these mothers at 24 weeks to determine treatment preference and effectiveness Questions