View PowerPoint document - New Mexico Highlands University's
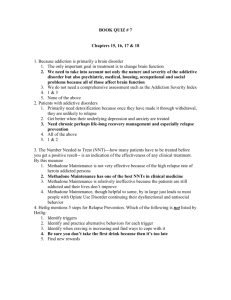
advertisement

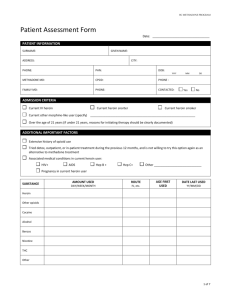
Medically Assisted Treatment For Opiate Addiction 3rd Annual Alcohol and Substance Abuse Treatment Conference May 13, 2014 Bruce G. Trigg, MD Duke City Recovery Toolbox Albuquerque, NM Faculty Disclosure I am employed as a contractor by a faith-based, for-profit opioid treatment program in Albuquerque, where I prescribe methadone and buprenorphine. I do not receive any funding from pharmaceutical companies Goals of this talk: • What is MAT? • What is the scientific evidence supporting MAT? • What are the barriers keeping millions of people who are addicted to opiates from benefiting from these therapies? • What is harm reduction and how does this fit in with treatment of addiction? What is Medication Assisted Therapy? MAT combines pharmacological intervention with counseling and behavioral therapies to treat addiction. Currently three treatments approved in US • Methadone • Buprenorphine (Suboxone) • Naltrexone Overdose Deaths in New Mexico • Second highest rate in US • In 2012 – 486 deaths – 7% decrease from 2011 • More than half of 2012 deaths were from prescription medications New Mexico Profile 2010 Other Public Health Impacts of Opiate Addiction in NM • Estimated 23,000 IV drug users – mostly heroin • 10 to 20% of people living with HIV acquired their infections from injecting drugs • High rates of hepatitis C – more than 32,000 on NM Department of Health registry – at least 60% acquired from injecting drugs Social consequences of drug use in NM • High rates of incarceration and criminal justice sanctions impacting mostly young people of color Public Health Approaches to the Opioid Overdose Epidemic 1- Providing prescribers with the knowledge to improve their prescribing decisions and the ability to identify patients’ problems related to opioid abuse 2- To reduce inappropriate access to opioids 3- To provide substance abuse treatment to persons addicted to opioids 4- To increase access to effective overdose treatment Less Opioid Prescriptions • NM Depart of Health announced last week a 13% decrease in prescribed opioids from 2010 to 2013 • Impact of media, provider education programs, NM Prescription Monitoring Program, increased vigilance by professional licensing boards and DEA “The key driver of the overdose epidemic is underlying substance abuse disorder.” Medication-Assisted Therapies — Tackling the OpioidOverdose Epidemic 4/24/14 NEJM Dopamin e Picture of opiate addiction: heroin Picture of opiate addiction: pain pills What is addiction? • A term referring to compulsive drug use, psychological dependence, and continuing use despite harm. • Addiction is frequently and incorrectly equated with physical dependence and withdrawal. Physical dependence, not addiction, is an expected result of opioid use. NIH Consensus Statement 1997 • “Whatever conditions may lead to opiate exposure, opiate dependence is a brain-related disorder with the requisite characteristics of a medical illness.” Effective Medical Treatment of Opiate Addiction. NIH Consensus Statement 1997 Nov. 17-19;15(6):4 NNI Addiction to heroin is a chronic, relapsing disease with high morbidity and mortality • 33 year follow up of 581 male heroin addicts in Los Angeles found: – – – – Nearly half had died 20.7% of those living tested positive for heroin 40% reported using heroin in past year High rates of disability, hepatitis, mental health disorders, and criminal activity – Fewer than 10% were in methadone maintenance Rx. “Methadone Maintenance and Other Pharmacotherapeutic Interventions in the Treatment of Opioid Addiction.” April 2002, Vol.III, No. 1 History of Methadone • Synthesized in Germany during WWII • In 1960s at Rockefeller University in New York City, Drs. Vincent Dole and Marie Nyswander, performed studies showing effectiveness for treatment of heroin addiction • First clinics opened in NYC in mid-1960s Medication Assisted Therapy • The substitution of an opiate-like medication to prevent withdrawal and minimize craving for opiates. • A medical model for the treatment of opiate dependence. Treats opioid dependence as a chronic, relapsing disease. • Effective medications – Methadone or Buprenorphine Medication Assisted Therapy (MAT) The primary goal of MAT is to reduce illegal heroin and other opiate use and the crime, diseases, and deaths associated with opiate addiction and allow patients to live healthy and fulfilling lives. Why is overdose potential low with buprenorphine? Respiratory suppression, death Opioid Effects Agonist: Methadone, Heroin, etc. Partial Agonist: Buprenorphine Antagonist: Naltrexone Log dose Functions of Drugs at mu Receptor Full agonists such as methadone: • Occupy the receptor and activate that receptor • Increasing doses of the drug produce increasing receptor-specific effects until a maximum or toxic effect is achieved • Most abused opioids are full agonists Pharmacologic Properties of Heroin and Methadone Onset of action Heroin Immediate Methadone 30 minutes Duration 4 to 6 hours 24 to 36 hours Route of administration Injection, Snorting, or Smoking Oral What is the abuse potential? • “Methadone’s half-life is approximately 24 hours and leads to a long duration of action and once-a-day dosing. This feature, coupled with its slow onset of action, blunts its euphoric effect, making it unattractive as a principle drug of abuse.” Effective Medical Treatment of Opiate Addiction. NIH Consensus Statement 1997 Nov. 17-19;15(6):14 Treatment Outcome Data: Methadone Maintenance • • • • • • 4-5 fold reduction in death rate reduction of drug use reduction of criminal activity engagement in socially productive roles reduced spread of HIV excellent retention • (see: Joseph et al, 2000, Mt. Sinai J.Med., vol 67, # 5, 6) © Martin, J. 2012 Methadone IS effective • After 1 year, 60% reduction in drug use • After 2 years, 85% • 70% reduction in crime within 4 months • Ball and Ross 1991 • Decreased transmission of blood-borne diseases • Less HIV infection: 5% seroconversion in treated versus 26% non-treatment group – Metzger 1993 Crime Among 491 Patients Before and During MMT at 6 Programs Crime Days Per Year 300 250 200 Before TX During TX 150 100 50 0 A B C D E F Adapted from Ball & Ross - The Effectiveness of Methadone Maintenance Treatment, 1991 Opioid Agonist Treatment of Addiction - Payte - 1998 Note: This shows criminal activity at six different methadone maintenance programs, comparing rates before treatment (pink) to during treatment (yellow). © Martin, J. 2012 HIV Conversion In Treatment 35% 30% 25% 20% IT OT 15% 10% 5% 0% Base line 6 Month 12 Month 18 Month HIV infection rates by baseline treatment status. In treatment (IT) n=138, not in treatment (OT) n=88 Source: Metzger, D. et. al. J of AIDS 6:1993. p.1052 Opioid Maintenance Pharmacotherapy - A Course for Clinicians - 1997 Note: This slide shows protection from HIV sero-conversion by enrollment in MMT: the longer the treatment the more relative protection from HIV. © Martin, J. 2012 How should methadone be prescribed? Best outcomes achieved when patients: • are maintained for long periods of time (at least one year) Relapse rate c. 80% in 1 year. • receive high doses (usually 80 to 120 mg daily) – low dose prevents withdrawal symptoms. – higher doses minimize craving for opiates. Exhibit 5-3. Heroin Use in Preceding 30 Days (407 Methadone-Maintained Patients by Current Methadone Dose) Adapted from Ball and Ross, The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and Outcome, Appendix B, p. 248, with permission Methadone Regulation • Can only be dispensed by licensed Opioid Treatment Programs (OTPs) • Must follow federal and state regs • Requires daily dispensing ( six days a week) for first 90 days • By one year can receive up to 2 weeks of take-home doses • Eventually may receive 14 to 30 day supply NIH Consensus Statement 1997 • “Although a drug-free state represents an optimal treatment goal, research has demonstrated that this goal cannot be achieved or sustained by the majority of opiate-dependent people.” Effective Medical Treatment of Opiate Addiction. NIH Consensus Statement 1997 Nov. 17-19;15(6):5 Should MMT Ever be Discontinued? • Opioid addiction is a chronic, relapsing condition, so long-term treatment is indicated. • Prognosis after withdrawal from MMT is dismal: most patients relapse before 12 mos. (compare this to diabetes, hypertension, epilepsy, etc. – other chronic conditions that require ongoing medication) © Martin, J. 2012 Relapse to IV Drug Use After MMT Should MMT Everwho be Left Discontinued? 105 Male Patients Treatment Exhibit 5-3. Heroin Use in Preceding 30 Days (407 Methadone-Maintained Patients by Current Methadone Dose) Adapted from Ball and Ross, The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and Outcome, Appendix B, p. 248, with permission 100 Percent IV Users • Opioid addiction is a chronic, relapsing 82.1 80 72.2 condition, so long-term treatment is 60 57.6 indicated. 45.5 40 • Prognosis28.9 after withdrawal from MMT is 20 dismal: most patients relapse before 12 0 mos. (compare this to diabetes, IN 1 to 3 4 to 6 7 to 9 10 to 12 hypertension, epilepsy, etc. – other Treatment Months Since Stopping chronic conditions Treatment that require ongoing Adapted from Ball & Ross - The Effectiveness of Methadone Maintenance Treatment, 1991 medication) Opioid Agonist Treatment of Addiction - Payte - 1998 Note: When patients taper off of methadone maintenance, relapse is almost universal. There is no way to predict who are the 18% of patients who will not relapse within a year. During medically supervised withdrawal, close © Martin, J. 2012 observation and keeping open the possibility of resuming therapeutic doses promptly is indicated. Myth #1 Methadone substitutes one addiction for another; a patient on methadone is still a drug “addict” Methadone Reality • A patient on methadone treatment is not a “drug addict” because addiction is compulsive use of drug despite knowing it is causing harm. A methadone patient is being prescribed a medication in a controlled environment for treatment of addiction. • Methadone substitutes a legal, long-acting, safe, prescribed opiate-like medicine for an illegal, dangerous, short-acting opioid. Myth #2 Methadone is more “addictive” and “harder to kick” then heroin Kosten & O’Connor, NEJM 2003 Myth #3 Higher doses of methadone are harder to “kick” therefore patients should be only low does of methadone Methadone Reality • Patients need to be on methadone for a minimum of one to two years, and many will need to be on MMT longer. • Therefore they should aim for a dose that enables them to be free of withdrawal symptoms, cravings for opiates, and that will block use of illegal opiates. For most this will be 80 to 120 mg. Myth #4 Patients should get off methadone as quickly as possible Methadone Reality • Most patients need a minimum of one year of methadone to stabilize their life and their health. • Treatments for other chronic diseases; high blood pressure, diabetes, high cholesterol are long-term. • Relapse carries with it the risk of overdose death, infection with HIV and hepatitis, incarceration, and violent death from a life of crime Myth #5 Methadone is a form of social control used by the government Methadone Reality • Methadone is the standard of care in at least 75 countries and is endorsed by US public health and medical organizations and international public health organizations such as WHO and UN • The patient should decide when to start and when to discontinue treatment. Patients should be involved in all decisions about lowering and raising doses unless their safety is at stake • The patient can decide to taper off methadone (detox) any time they wish. • A safe taper should be slow (10% dose reduction every 5 to 10 days) and under the control of the patient; the patient is allowed to stop a taper or to resume a higher dose if they wish. Myth #6 Patients on methadone relapse because they are weak, immoral, or unreliable A Chronic, Relapsing Disease… • Similar to other chronic, relapsing diseases, such as diabetes, asthma, or heart disease, drug addiction can be managed successfully. • As with other chronic diseases, it is not uncommon for a person to relapse and begin abusing drugs again. • Relapse ≠ failure. It means that treatment should be adjusted, alternative treatment considered, and psychosocial support increased to help the individual regain control and recover. NIDA InfoFacts: Understanding Drug Abuse and Addiction, June 2008 Percent of Patients Who Relapse Relapse Rates Are Similar for Drug Dependence And Other Chronic Illnesses 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Addiction Treatment Does Work Drug Dependence Type 1 Diabetes Hypertension Asthma Source: McLellan, A.T. et al., JAMA, Vol 284 (13), October 4, 2000. Compliance rates for chronic illnesses McClellan AT et al, JAMA 2000, 284:1689 Myth #7 Methadone causes damage to the teeth, the bones, the liver, and …. Methadone Reality • Methadone does not damage the liver (many patients have chronic hepatitis C) • Methadone does not damage the teeth (many patients have not taken care of their teeth) • Methadone does not “get into the bones” rather some patients may be experiencing withdrawal due to being on an inadequate dose of methadone Methadone in NM • More than 2,000 patients • Clinics in 4 cities: ABQ (5 programs, 6 clinics), Santa Fe, Espanola, Belen, Las Cruces • Soon to open in Farmington, Gallup, Roswell • Also a methadone maintenance program at Bernalillo County Metropolitan Detention Center (MDC) for persons on methadone at Buprenorphine: Newer Medication for Treating Opiate Addiction • First synthesized as an analgesic in England, 1969. • Recognized as potential addiction treatment by NIDA researchers in 1970s. • NIDA created Medications Development Division to focus on developing drug treatments for addiction, 1990. • NIDA formed an agreement with the original developer to bring buprenorphine to market in the U.S., 1994. Buprenorphine Drug Addiction Treatment Act of 2000 allows qualified physicians to prescribe Schedule III-V drugs for treatment of opiate dependence (Buprenorphine is Schedule III) Approved by the FDA, 2002 Requires physicians to complete 8 hours of training/certification Designed for treatment in primary care practices Buprenorphine Nurse practitioners and Physician Assistants cannot prescribe buprenorphine Registered physicians can treat up to 30 patients at one time with buprenorphine After one year may apply to increase to 100 patients at one time Physician must be able to refer for counseling services Buprenorphine in use Suboxone: buprenorphine + naloxone (Narcan) Naloxone lowers abuse potential → causes withdrawal if other opiates are present Naloxone not active when taken by sublingual route – Subutex: just buprenorphine (no naloxone) – used most commonly with pregnant women • Suboxone sublingual film approved by FDA in 2010 (no Subutex film) • Zubsolv is a generic buprenorphine/naloxone sublingual tablet that is equivalent to Suboxone Why is overdose potential low with buprenorphine? Respiratory suppression, death Opioid Effects Agonist: Methadone, Heroin, etc. Partial Agonist: Buprenorphine Antagonist: Naltrexone Log dose Why isn’t buprenorphine abused? • Most drugs of abuse are full agonists • Drugs of abuse are injected, smoked, “snorted”, not taken orally/sublingually • Except for in pregnancy, most patients receive a combined buprenorphine and naloxone form of the medication (Suboxone and Zubsolv) • When taken under the tongue, the naloxone is not absorbed and so is not active • When injected, the naloxone is active and causes withdrawal Suboxone 8/2 mg and 2/.5 mg sublingual tablets Buprenorphine and heroin overdose Increasing use of buprenorphine in France associated with 1,2 – Decrease in arrests for heroin (77% decline since 1995) – Decrease in overdose deaths (81% decline since 1995) 1. Auriacombe 2004, Am J Addict;13. 2. Lepere 2001, Ann Med Interne (Paris);152 Suppl 3. Buprenorphine vs Methadone Like Methadone… • Reduces IVDU • Retains patients in treatment • Decreases craving • Stops withdrawal • Costs $ 5-13 per day Unlike Methadone…. • Low potential for OD • Prescribed in MD office • Less sedation • Easy taper/detox Why People Switch from Methadone to Buprenorphine? • • • • • • • • Cost, insurance coverage Safety –risk of fatal overdose for kids! Stigma Ability to receive take-home doses and other lifestyle, transportation, and confidentiality concerns Personal preference: “I like how I feel on buprenorphine” Medical issues Legal issues (Drug Courts may prohibit methadone) Inaccurate information Transitioning Stable Methadone Maintenance Patients to Buprenorphine Maintenance • J Addict Med 2010;4: 88-92 • Methods: Retrospective study, 104 patients on low methadone doses (5 to 80mg) offered conversion to buprenorphine - 25 accepted • Results: all succeeded. Found low-moderate association between pretransfer methadone dose and posttransfer bupe dose. Buprenorphine induction • Buprenorphine will cause withdrawal if given to an opiate-dependent patient • Must wait until patient is in mild-moderate withdrawal before starting buprenorphine • Dose adjustment over the first week to find most effective dose • Usual dose is 16 mg buprenorphine and recommended range is 12 to 16 mg. Higher doses generally discouraged. RCT of buprenorphine • 40 Heroin addicts • Buprenorphine 8mg/day vs taper + placebo • All received counseling, groups • Followed for 1 year Buprenor -phine Retained at 1 yr Placebo 70% 0 0 20% % died Kakko et al, Lancet 2003 Percent of Patient Sample Buprenorphine Patient Outcomes: Specific Criminal Activities “In the past 30 days were you involved in any of the following activities…?” 20% Baseline 16% 30 Day 6 Month 15% 10% 10% 10% 5% 3% 1% 1% 1% 2% 1% 0% Drug Dealing Prescription Fraud Other Crimes n=379 Source: SAMHSA Patient Longitudinal Study, November 2005 Methadone and Buprenorphine • Providers should discuss the advantages and disadvantages of methadone and buprenorphine with all patients before starting treatment • Buprenorphine patients should be made aware that methadone is an alternative Rx if they repeatedly relapse Why People Switch from Methadone to Buprenorphine? • • • • • • • • Cost Safety – death risk for kids! Stigma Lifestyle/transportation/confidentiality “I like how I feel on buprenorphine” Medical issues Legal issues (Drug Court prohibits methadone) Inaccurate information Who May Do Better on Methdone? • Persons with a longer addiction history • Those maintained on very high doses of methadone • People who relapse repeatedly on buprenorphine (especially if at risk of imprisonment or with serious medical problems/mental health). • People who need more structured Rx program with mandatory counseling, drug tests, etc. . Induction to Buprenophine from Methadone • Important to facilitate transfer to a new provider since relapse risk is • Patient should be on 30 mg or less of methadone for at least one week before switching • Discontinue methadone for 48 to 72 hours so patient is in mild to moderate withdrawal (COWS 12 or higher) Special Populations • Methadone approved starting at 18 years old but special waivers can be obtained • Buprenorphine approved starting at 16 years but off-label use in high risk situations not unreasonable • Pregnancy – more experience with methadone but recent study showed safety of buprenorphine and less NAS than with methadone National Institute of Health (NIH) Consensus Statement 1997 “All opiate-dependent persons under legal supervision should have access to methadone maintenance therapy…” Effective Medical Treatment of Opiate Addiction. NIH Consensus Statement 1997 Nov. 17-19;15(6):2 Mortality Rates among Former Inmates of the Washington State Department of Corrections during Study Follow-up (Overall) and According to 2-Week Periods after Release from Prison. N Engl J Med 2007;356:157-65. The dashed line represents the adjusted mortality rate for residents of the State of Washington (223 deaths per 100,000 person-years), and the solid line represents the crude mortality rate among inmates of the state prison system during incarceration (201 deaths per 100,000 inmate person-years). Why MAT in Jails and Prisons? • • • • • • • • Significantly less injecting during incarceration Decreases HIV and hepatitis C transmission Facilitates continuity of treatment Reduces mortality Facilitates post-release treatment Reduces criminal recidivism Positive effect on prison environment Decreases overdoses Evidence for Action Technical Papers INTERVENTIONS TO ADDRESS HIV IN PRISONS DRUG DEPENDENCE TREATMENTS World Health Organization, UNODC, UNAIDS / Geneva, 2007 Untreated Heroin Dependency has the highest Recidivism rate for women at NM Women’s Correctional Facility in Grants No Substance Abuse Alcoholic Only Cocaine Addict* Heroin Addict* Other Addict* Recidivism Rate 100% 80% 60% 40% 20% 0% 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 Time (months) Senate Joint Memorial 29 study from 1997-2000 Countries (+territories) that have Methadone in prison • Australia • Austria (+ buprenorphine, morphine) • Belgium (detox only) • Canada • Denmark • England • Estonia • France (+buprenorphine) • Germany (+ NEX) • Indonesia • Ireland • Iran • • • • • • • • • • • • Italy (detox only) Luxembourg Netherlands N. Ireland (detox only) Poland Portugal Puerto Rico Scotland Slovenia Spain Switzerland (+heroin, NEX) United States (jail only) Sources: Dolan 2001, EMCDDA 2002, updated 2011 Respiratory suppression, death Opioid Effects Agonist: Methadone, Heroin, etc. Partial Agonist: Buprenorphine Antagonist: Naltrexone Log dose Naltrexone for Extended-Release Injectable Suspension (Vivitrol) • Approved by FDA for treatment of opiate addiction in 2010 • Approved for: – treatment of alcohol dependence in patients who are able to abstain from alcohol in an outpatient setting prior to initiation of treatment – prevention of relapse to opioid dependence, following opioid detoxification Opiate antagonist therapy: Naltrexone • • • • Blocks action of opiates Problem: adherence and cravings Only 20% success at 6 months 1 More effective in highly structured situations: >90% success for health care professionals 2 • Long-acting injectable form available but very expensive. 1 2 Rothenberg JL et al, J Subst Abuse Treatment 2002 Roth A et al, J Subst Abuse Treatment 1997 Naltrexone • Must be abstinent for 7 days before starting treatment • More experience now with people leaving abstinence-based rehab programs, incarceration or who discontinue MAT Successful Treatment of Opiate Addiction • MAT in a supportive, structured environment • Balance limit-setting with understanding • Behavioral therapy: counseling and/or group • Address mental health issues Successful Treatment of Opiate Addiciton • Case Management: Assist with obtaining benefits, jobs, housing if needed • Relapse is the rule, not the exception • Staying in treatment for an adequate period of time is best predictor of success; maintenance more effective than detox • Non-judgmental, empathic care • Assurance of confidentiality Paying for MAT in NM • Methadone maintenance therapy and buprenorphine are covered by Medicaid • Buprenorphine generally paid for by private insurance • Methadone not generally paid for by private insurance • VA in Albuquerque has a buprenorphine but not a methadone program TREATMENT OF OPIATE DEPENDENCE Abstinence-based therapy Opiate -replacement therapy methadone Opiate antagonist therapy: naltrexone buprenorphine Abstinence-based therapy Goals: development of recovery skills, ability to deal with emerging mental and emotional issues, sober community • Counseling • Peer support: 12-step, Smart Recovery, Double Trouble • Social services – Housing – Vocational rehab – Childcare A study of heroin overdose deaths in Baltimore between 1995 and 2009 found an association between the increasing availability of methadone and buprenorphine and an approximately 50% decrease in the number of fatal overdoses. Schwartz RP, Gryczynski J, O’Grady KE, et al. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995-2009. Am J Public Health 2013;103:917- 22. The New Mexico Harm Reduction Act (1997) The NM Dept. of Health shall: • Establish and administer a harm reduction program for the purpose of sterile hypodermic syringe and needle exchange. • Compile data to assist in planning and evaluation efforts to combat the spread of blood-borne diseases. This statute makes access to clean injection equipment a right rather than a privilege in New Mexico. What is Harm Reduction? HARM REDUCTION is any intervention or policy designed to reduce the negative consequences of drug use without requiring drug use cessation. Another way to think about it… HARM REDUCTION is a way of working with drug users to improve their health even if they are not ready or willing to quit using drugs. 4 Key Harm Reduction Strategies Needle/Syringe Exchange Overdose Prevention with provision of naloxone Increasing access to MAT Condom availability Why Talk about Harm Reduction at a presentation on MAT? • Relapse is common in people in MAT as with any chronic disease • Useful to discuss the possibility of relapse and precautions to take to decrease harm • All MAT patients should be referred for Harm Reduction services: – Needle/Syringe Program including safer injecting info – Overdose prevention education and naloxone – HIV, Hepatitis B and C testing and education – Immunization for hepatitis B Harm Reduction Program Goals Reduce the incidence of blood-borne infections HIV, HBV, HCV Reduce the incidence of other diseases caused by reusing or sharing syringes abscesses, endocarditis, septicemia Prevent deaths from accidental overdose Educate clients on safer use strategies Assist clients to access drug treatment and other related health services What is Naloxone? Naloxone (brand name Narcan) is a prescription drug that reverses the effects of an opioid overdose by blocking the opioid’s action on the brain and restoring breathing. Naloxone’s only purpose is to reverse overdose; it is not a “recreational” drug and does not cause a “high.” The use of naloxone, in combination with rescue breathing, can save a life. Naloxone in Action Providing naloxone to IDUs in NM • Participants receive training in recognizing opiate overdose, rescue breathing and naloxone administration • Dispensed by licensed clinicians • Naloxone is prescribed to a specific named individual • The “911 – Good Samaritan Act” NM’s Good Samaritan 911 Law • In 2007, NM passed the 1st Good Samaritan 911 law in the nation. • It allows someone to call 911 or take someone to the hospital for a drug overdose without being charged for possession. • The law covers both the caller and person who OD’d. • The law does NOT protect someone if: – they are on probation, parole, or have arrest warrants – there is evidence of drug dealing → scales, baggies, drugs or money in plain sight – there is evidence of other crimes, including weapons’ possession or DUI Approximately 2,000 opioid overdose reversals were reported to the New Mexico Department of Health Harm Reduction Program through 2012. Data Suggests Naloxone Program Saving Lives, KUNM, 4/5/13 “So without the presence of Naloxone in Rio Arriba, the death rate could have been absolutely astronomical.” (Brad Wharton, NMDOH Drug Epidemiologist) “Consider prescribing naloxone along with the patient’s initial opioid prescription. With proper education, patients on long-term opioid therapy and others at risk for overdose may benefit from having a naloxone kit to use in the event of overdose.” Candidates for naloxone include those who: • take high doses of opioids long-term for pain management • take any dose of opioid for legitimate pain management combined with suspected or confirmed history of substance abuse, dependence, or non-medical use of opioids • recently completed opioid detox or inpatient treatment program • recently were released from incarceration with a past history of opioid abuse • recently experienced an overdose SAMSHA Opioid Overdose Toolkit: Information for Prescribers, 2013 Methadone and buprenorphine are the “nicotine patches” of heroin addiction treatment Of the 2.5 million Americans who abused or were dependent on opioids in 2012, fewer than than 1 million received a medication assisted therapy (MAT) National Survey on Drug Use and Health conducted by SAMHSA What are the barriers to MAT? • Too few trained prescribers • Stigma and misunderstanding by the public, medical, mental health and criminal justice workers • Policy and administrative (ie insurance coverage) Recommendations • Every patient who is addicted to heroin or other opioids should be given accurate and non-judgmental information about MAT and referred for further information or treatment if they wish. • Refer all people who inject drugs to a harm reduction program for needles and syringes and anyone using chronic legal or illicit opioids for naloxone Recommendations • All persons under control of the criminal justice system should have access to the community standard of treatment for opiate addiction – MAT • Drug courts should follow evidence-based standards of addiction care and not exclude people on MAT and encourage people with opiate addiction to seek MAT Recommendations • Peer support (12 Step Programs, NA, etc), should not discriminate against nor ostracize people who receive MAT. People on MAT are in recovery from addiction. • Health insurance companies must be required to pay for evidence-based treatments for addiction as for any other medical condition. Recommendations • Consider how medical and treatment communities contribute to stigma of addiction and of MAT. • Language used in treatment programs (for example “drug free,” as opposed to people on MAT, “drug addicts or junkie,” “detox” instead of tapering for MAT, “dirty or clean” urine tests rather than positive or negative” etc. ) UNM Project ECHO Offers free buprenorphine training courses and physician certification Next scheduled for Farmington, NM on May 31, 2014 Weekly telemedicine conference on Fridays, 12 to 2 pm Training for community health workers to work in treatment of opiate addiction. Contact: Jeanne Block 505-272-8338 Thank you Bruce G. Trigg, MD trigabov@gmail.com