inde222-09-25-2015-1..
advertisement
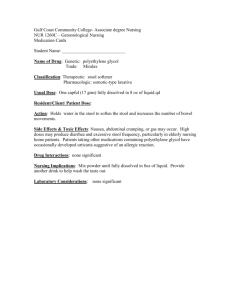
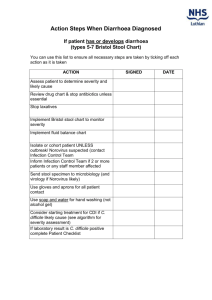
WATER TRANSPORT AND DIARRHEA Anson Lowe Medicine/Gastroenterology September 25, 2015 Understand water transport Understand the causes of diarrhea Understand secretory vs. osmotic diarrhea Water transport; diarrhea Grant’s Atlas, 1972 Ingested Endogenous secretions Salivary glands Stomach Bile Pancreas Intestine Total input Reabsorbed Jejunum Ileum Colon 2000 7000 1500 2500 500 1500 1000 7000 9000 8800 5500 2000 1300 8800 Balance in stool *Moore,EW, Physiology of Intestinal Water and Electrolyte Absorption, 1976 200 Black RE, et al., Lancet 375:1969 (2010) Childhood Deaths 11 million per year ◦ 1 in 5 die before their fifth birthday 70% are secondary to pneumonia, diarrhea, measles, malaria, and malnutrition 2 million die of diarrhea diseases, 90% of whom could have been saved by the appropriate treatment Cholera Death Rates Estimated 1 million cases / year 100,000 - 130,000 deaths / year Case fatality rates: South Africa = 0.22% Other parts of Africa = up to 30% WHO Gary Schoolnik Environmental Degradation Begets Epidemics: Cholera in Bangladesh Medicine Grand Rounds November 21, 2007 url: http://lane.stanford.edu/biomedresources/grandrounds/medgrandrounds-2007.html transepithelial P.D. mucosal resistance passive NaCl movement [Na+] equilibrium conc. Jejunum -3mv low high 133 mEq/l ileum -6mv med low 75 Colon -20mv high minimal 30 What is the implication with respect to stool osmolarity? What is the difference between the nephron and the intestine? www.med.uiuc.edu http://en.wikipedia.org/wiki/Thick_ascending_limb_of_loop_of_Henle Absorption of most solutes from the intestinal lumen is secondary active transport. The major driving force is Na+:K+-ATPase. Unlike the kidney, the intestine does not possess a diluting segment. Thus the intestinal fluid is always isotonic with respect to plasma. Stool Osmolarity In contrast to the kidney, the GI tract cannot dilute or concentrate its contents Stool contents is always isotonic Serum osmolarity is tightly regulated at ~290 mosm. Why do we separate digestion into a lumenal and mucosal phase? Why do we separate digestion into a lumenal and mucosal phase? ◦ Lumenal digestion of a disaccharide would increase intestinal volume two-fold Hypertonic Stool Hypertonic Stool • High stool osmolarity suggests a prolonged period of incubation before processing. Sleisenger and Fordtran, Gastrointestinal Disease, 5th ed. Hypotonic Stool Hypotonic Stool Suggest the addition of free water to the stool Osmotic Gap Osmotic gap = 290mosm - (([Na+] + [K+] ) x 2) A gap of < 40mosm suggests a secretory diarrhea How do we absorb water? How do we absorb water? Beer = 4 mosm/liter Proc. Natl. Acad. Sci. USA93:13367-13370 (1996) SGLT1 and Water Absorption Co-transport of 2 Na+, 1 glucose, and 264 water molecules ◦ Blocking glucose transport with phlorizin will also block water transport SGLT1 and Water Absorption Also able to transport water in response to an osmotic gradient Produces an osmotic gradient that can be used by other water channels such as the aquaporins WHO Oral Rehydration Solution [Na+] = 90 mEq/L [K+] = 20 mEq/L [Cl-] = 80 mEq/L Citrate = 30 mEq/L Glucose = 20 gm/L (111 mM) Alberts et al, Moleculare Biology of the Cell, 3rd ed. CFTR Functions as a chloride channel and also regulates other transport pathways Can mediate water transport Advantage of CFTR mutations? Advantage of CFTR mutations? Knockout CFTR mice have been produced Advantage of CFTR mutations? Knockout CFTR mice have been produced ◦ Mice die of intestinal obstruction Advantage of CFTR mutations? Knockout CFTR mice have been produced ◦ Mice die of intestinal obstruction Homozygous mice are resistant to cholera toxin Advantage of CFTR mutations? Knockout CFTR mice have been produced ◦ Mice die of intestinal obstruction Homozygous mice are resistant to cholera toxin Heterozygote mice are partially resistant to cholera toxin Normal Pancreas, H&E Univ. of Kansas, Dept. of Pathology Secretory Diarrheas E. coli heat stabile enterotoxin Cholera Staph. Aureus B. Cereus Vasoactive intestinal peptide (VIPoma) Secretory Diarrheas Excess secretion Nutrient absorption intact ◦ Therapy? Secretory Diarrheas Excess secretion Nutrient absorption intact ◦ Oral rehydration formula [Na+] = 90 mEq/L [K+] = 20 mEq/L [Cl-] = 80 mEq/L Citrate = 30 mEq/L Glucose = 20 gm/L (111 mM) Secretory Diarrhea due to a VIPoma? (vasoactive intestinal peptide) Somatostatin Source: ◦ Neurons of CNS and PNS ◦ Endocrine cells of the pancreas (D cells) and stomach Actions in the GI tract ◦ Inhibition of transport ◦ Inhibition of secretion ◦ Splanchnic vasoconstriction Somatostatin Clinical Applications ◦ Inhibition of many G-protein mediated processes Secretory diarrhea Pancreatic secretions Gastrointestinal hemorrhage (variceal bleeding) induces splanchnic vasoconstriction Diarrhea-Acid/Base Disorders What disturbances in acid base balance will be seen with significant diarrhea? Diarrhea-Acid/Base Disorders What disturbances in acid base balance will be seen with significant diarrhea? ◦ Non-anion gap metabolic acidosis Anion gap = ([Na] + [K]) - ([Cl] + [HCO3-]) Distal Colon high resistance, high potential difference, low permeability to ions no nutrient dependent absorption (e.g. Na+:glucose) responsive to mineralcorticoids transepithelial P.D. mucosal resistance passive NaCl movement [Na+] equilibrium conc. Jejunum -3mv low high 133 mEq/l~ ileum -6mv med low 75 Colon -20mv high minimal ~30 Metabolic Changes with Diarrhea Hypokalemic, hyperchloremic, non-anion gap metabolic acidosis colonic limit is < 5L/d Stool Characteristics • • • • • consistency of the stool (semi-solid or watery) stool volume presence of blood or pus in the stool nocturnal diarrhea relationship to meals Definitions of Diarrhea Stool consistency Stool volume Frequency (> 2/day) Stool volume > 250 g/day Gastrointestinal Disease, ed: M.H. Sleisenger and J.S. Fordtran (1989), page 1034 Stool fecal volume > 250 g/day fecal fat, fecal electrolytes < 6g fat /day osmotic gap (? secretory or osmotic) yes osmotic stool pH laxative screen no secretory VIP 5HIAA histamine calcitonin thyroid function laxative screen > 6g fat/day, osmotic D-xylose test (check mucosal integrity) normal CT scan ERCP trial of pancreatic enzymes abnormal small intestinal biopsy small intestinal X-ray