2.Renal Clearance Concepts
advertisement

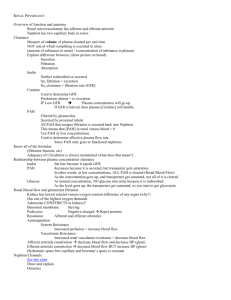
Renal Clearance Concepts Dr. shafali singh Learning Objectives: • To define renal clearance and calculate renal clearance of different substances. Calculate GFR values using inulin clearance. • Calculate renal plasma flow and RBF using PAH clearance and hematocrit. • Characterize tubular transport using solute clearance. • Define the basis for the clinical use of plasma creatinine and urea levels to assess renal function. • List different markers used for measuring GFR, RPF and RBF • Understand fractional clearance of a substance (Na) and its importance • Understand osmolar clearance and free water clearance ASSESSMENT OF RENAL FUNCTION • The principle of renal clearance emphasizes the excretory function of the kidneys; • it considers only the rate at which a substance is excreted into urine and not its rate of return to the systemic circulation in the renal vein. • Therefore, in terms of mass balance the urinary excretion rate of substance x (Ux × V.) is proportional to the plasma concentration of substance x, To equate the urinary excretion rate of substance x to its renal arterial plasma concentration, it is necessary to determine the rate at which it is removed from plasma ;by the kidneys. This removal rate is the clearance (Cx). • Thus, the 2 factors which determine clearance are the plasma concentration of the substance and its excretion rate. • Urine flow (V) is a volume per unit time, and the units of V will become the units of clearance. • Clearance is a volume of plasma cleared of a substance per unit time, mL/min or L/day. Clearance • Clearance refers to a theoretical volume of plasma from which a substance is removed over a period of time. • • • • • • example: If the concentration of substance x is 4 molecules per liter and the excretion of x is 4 molecules per minute, the volume of plasma cleared of x is 1 L per minute. If the excretion of x decreases to 2 molecules per minute, the volume cleared of x is only 0.5 L per minute. If the concentration of x decreases to 2 molecules per liter of plasma and the excretion is maintained at 2 molecules per minute, the cleared volume is back to 1 L per minute. • Renal plasma clearance is the volume of blood that is “cleaned” or cleared of a substance per unit of time, usually • expressed in units of milliliters per minute. • High renal plasma clearance indicates efficient excretion of a substance in the urine; low clearance indicates inefficient excretion Clearance Example • Substance Z has a urine concentration of 100 mg/ml • Urine flow rate is 1 ml/min • Plasma concentration is 1 mg/ml Calculate the Clearance ? Clearance Example • Calculate the Clearance CZ = Uz • V Pz CZ = (100mg/ml) • (1 ml/min) 1 mg/ml CZ = 100 ml/min The clearance of a solute depends on the three basic processes of a nephron: 1. glomerular filtration, 2. tubular reabsorption, 3. and tubular secretion. Consider a substance that is filtered but neither reabsorbed nor secreted. Its clearance equals the glomerular filtration rate because all the molecules that pass the filtration membrane appear in the urine. • This is very nearly the situation for creatinine; it easily passes the filter, it is not reabsorbed, and it is secreted only to a very small extent • Measuring the creatinine clearance, which normally is 120–140 mL/min, is the easiest way to assess glomerular filtration rate. . Creatinine • Creatinine is a byproduct of skeletal muscle creatine metabolism and is released from skeletal muscle at a constant rate proportional to muscle mass. • Creatinine is freely filtered and not reabsorbed by the kidney, although a very small amount is secreted into the proximal tubule. • Creatinine production = creatinine excretion = filtered load of creatinine = Pcr × GFR excreted load of creatinine= Ucr × V CLINICAL ESTIMATION OF GFR • The GFR is equal to the sum of the filtration rates of all functioning nephrons. Thus, it is an index of kidney function. • A fall in GFR means the disease is progressing, whereas an increase in GFR suggests a recovery. • Estimations of GFR rely on the concept of clearance • Thus, if creatinine production remains constant, a decrease in GFR would be reflected by an increase in plasma creatinine concentration, and an increase in GFR would be reflected by a decrease in plasma creatinine. • Plasma creatinine, however, is not a very sensitive measure of reduced GFR. It will only reveal large changes in GFR. • • • • • Any substance that meets the following criteria can serve as an appropriate marker for the measurement of GFR. The substance must Be freely filtered across the glomerulus into Bowman's space Not be reabsorbed or secreted by the nephron Not be metabolized or produced by the kidney Not alter the GFR Stable plasma concentration that is easily measured Ideal substances would include • inulin Alternatives include radioactive iothalamate, iohexol, diethylene triamine pentaacetic acid (DPTA), and the related • sucrose ethylene diamine tetraa-cetic acid (EDTA). • mannitol Even though the clearance of inulin is considered the gold standard for the measurement of GFR, it is not used clinically. Instead clinical estimates of GFR rely on creatinine Q • A 35-year-old woman is being evaluated for renal surgery. Her plasma creatinine concentration (PCr) is 0.8 mg/dL. A 24-hour urine collection has a creatinine concentration (UCr) of 90 mg/dL and a total volume (V) of 1,425 mL. What is her glomerular filtration rate (GFR)? Para-aminohippuric acid (PAH) The clearance of the organic anion para-amino hippuric acid (PAH) is also of clinical importance. After PAH is administered intravenously, it is filtered and secreted in a single pass through the kidneys. Thus, the clearance of PAH is used to measure renal plasma flow, the amount of plasma that passes through the kidneys in one minute. 120 mL/min by filtration and 480 mL/min by secretion. As such there would be no PAH in the renal venous blood Effective RPF = renal plasma flow (mL/min or mL/24hr) CPAH = clearance of PAH (mL/min or mL/24 hr) [U]PAH = urine concentration of PAH (mg/mL) V = urine flow rate (mL/min or mL/24 hr) [P]PAH = plasma concentration of PAH (mg/mL Measurement of renal plasma flow (RPF)— clearance of para-aminohippuric acid (PAH) Clearance of PAH measures effective RPF and underestimates true RPF by 10%. • PAH clearance at low plasma concentrations is referred to as effective renal plasma flow (ERPF) because some plasma perfuses the renal capsule. This flow (about 10%) is not cleared of PAH. • Thus, PAH clearance is only 90% of the true renal plasma flow. True RPF Q • A healthy 22-year-old man volunteers for a research study evaluating the effects of a new drug on renal blood flow (RBF). • The protocol required a urinary catheter to measure kidney output while infusing paraaminohippuric acid (PAH) intrave-nously. PAH concentration (PPAH) stabi-lized at 0.025 mg/mL. Urine flow rate (V) was then measured at 1.2 mL/min, and urine PAH concentration (UPAH) was 18 mg/mL. • Hematocrit (Hct) was 48%. What was the subject’s RBF? Clearance curves General pattern of clearance • Glucose: The normal clearance of glucose is zero. • Sodium: Always appears in the urine, thus sodium always has a positive clearance • Urea: Is freely filtered but partially reabsorbed • Inulin: is freely filtered and there is no transport. its clearance always equals GFR regardless of its plasma concentration • Creatinine: Since with creatinine everything filtered is excreted plus a small amount secreted, it has a clearance slightly greater than GFR. • PAH: The greatest clearance via the kidney is renal plasma flow this is the clearance of PAH at low plasma concentrations,. Fractional Excretion (FExx) • Another way of using Clearance to assess how kidney handles a substance is to compare Clearance of substance to clearance of creatinine or inulin. FEx = [(Uz)(Volurine)]/Pz [(Uin)(Volurine)]/Pin = (Uz)/Pz (Uin)/P in Clearance ratio • If C z/C in=1 the substance is filtered, but not reabsorbed nor secreted. • If C z/C in<1 the substance is not filtered, or filtered and subsequently reabsorbed • If C z/C in >1 the substance is filtered and secreted. Q 1. What does aldosterone do to clearance of Na? 2. What does PTH do to clearance of Ca and PO4? 3. Clearance of urea during dehydration and diuresis? question Q Which of the following substance is cleared the most by the kidneys? • Inulin • PAH • Creatinine • Urea Q • What is the term used to describe the amount of pure water that would be added or removed from urine per unit time in order to make it have the same osmolarity as plasma? Free Water Clearance • Free water clearance is the best measure of the balance between solute and water excretion. • Its use is to determine whether the kidneys are responding appropriately to maintain normal plasma osmolarity. • Free water clearance is how much solute-free water is being excreted; it is as if urine consisted of plasma (with solutes) plus or minus pure water Q What kidney ability is free water clearance actually a measure of? FWC is measure of the ability of the kidney to excrete water • Q What kind of urine generate a value of zero for free water clearance? • iso osmotic urine • Positive-free water clearance tends to cause increased plasma osmolarity; • negative free water clearance causes reduced plasma osmolarity. Q. What kind of urine generate a negative value for free water clearance? Hyperosmotic urine Q. What kind of urine generate a positive value for free water clearance? Hypo osmotic urine • If urine osmolarity was 300 mOsm/L (isotonic urine), free water clearance would be zero. • If plasma osmolarity is too low, urine osmolarity should be lower still(positive free water clearance) in order to compensate. • Positive-free water clearance tends to cause increased plasma osmolarity; • negative free water clearance causes reduced plasma osmolarity. • CH2O (+) = hypotonic urine is formed (osmolarity <300 mOsm/L) • CH2O (–) = hypertonic urine is formed (osmolarity >300 mOsm/L) • FWC = 1 – urine osmolarity × V plasma osmolarity Where V is volume of urine per unit time Q • V = 3.0 mL/min • Uosm = 800 mOsm/L • Posm = 400 mOsm/L What is the free water clearance? Free water reabsorption( FWR) • Opposite of FWC = urine osmolarity –1 × V plasma osmolarity • During the production of hyperosmotic urine FWR will be +ve,--ve or Zero?