(19%) ≤ 21 days Recurrent or chronic osteo Duration of IV therapy
advertisement

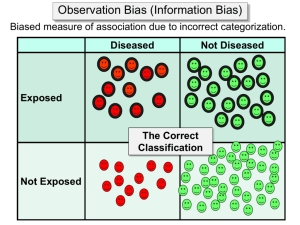
Prolonged IV vs. Early Conversion to Oral Antibiotic Therapy? Is it Time for a Change Theoklis Zaoutis, MD, MSCE Asst. Prof. of Pediatrics and Epidemiology Assoc. Director, Center for Pediatric Clinical Effectiveness Research Overview: Acute Osteomyelitis (AO) Background Study Methods and Results Bias -misclassification AO: epidemiology and risk factors 1 in 5000 each year in US 1% of pediatric hospitalizations 50% occur before 5 years old Twice as common in males 1/3 have preceding minor trauma AO: epidemiology by site Humerus (13%) Vertebrae (2%) Pelvis (7%) Femur (25%) Tibia (24%) Calcaneus (5%) AO: management Traditional management consists of 4-6 weeks of parenteral (IV) antibiotic therapy Duration of Therapy: Dich 1975 Immediate needle aspiration of subperiosteal space and bone. Drainage through bone window if pus found on needle aspiration. Exclusive IV antibiotics Duration of IV therapy Recurrent or chronic osteo ≤ 21 days >21 days 7/37 (19%) 1/47 (2%) Route of Therapy: Tetzlaff 1978 IV until signs of ’d inflammation (mean 7.3 d) Followed by PO (mean 19.8 d) Conditions for conversion to PO: Organism identified (blood, bone, joint) Peak bactericidal titer > 1:8 Hospitalized for duration of treatment (including oral therapy) Only 1/22 developed chronic osteo Route of Therapy: Cole 1982 Minimize surgery: bone aspiration for abscess drainage only (22%) Minimize duration of IV therapy (mean 3 d) Complete oral therapy as outpatient No bactericidal levels measured Cured after 6 weeks of therapy: 44/48 with “early” acute osteo (fever < 48 h) 2/8 with “late” acute osteo (symptoms >5 days, all with abscess) Route of Therapy: Peltola 1997 50 patients with S. aureus AO Surgery (needle aspiration or drilling) Conversion to high-dose 1st generation oral cephalosporin after 3-4 days Serum bactericidal activity and antibiotic concentrations not measured 3-4 weeks total therapy (mean 23 days) Intensive f/u with ESR x 8; CRP x 12 in 30 d. Mean 11 days of hospitalization No complications with 1 year follow-up Route of Therapy: Le Saux 2002 Systematic review Clinical cure rate at 6 months: IV: short course (< 7 d) vs. long-course (>7d) Then switch to PO antibiotics. 12 case series or small observational studies: 7 short-course and 5 long-course therapy. Clinical cure rate Short-course = 95.2% (95% CI; 90.4, 97.7) No Difference Long-course = 98.8% (95% CI: 93.6, 99.8) Safety of Prolonged IV Therapy IV x 5d, then PO AO n=80 No rehospitalization No return to ED n-=5 31/75 (41%) developed complications IV x 2wks with CVC n=75 • 17 (23%) CVC malfunction or displacement • 8 (11%) catheter-assoc bloodstream infection • 8 (11%) fever with negative blood cx • 4 (5%) local skin infection at CVC site Ruebner 2005 Pediatrics What is the Best Practice? What is currently being done in practice? Is early conversion to PO effective? We cannot perform the randomized, controlled clinical trial because: Certain centers have already changed to practice Clinical trial to find a failure rate of 5% vs. 2 % would require 1200 patients Specific Aims 1. To describe the variability in management of AO in children 2. To compare the clinical effectiveness of long-term IV vs. IV with early PO conversion for the treatment of AO Methods Study Design: retrospective cohort Data Source: Pediatric Hospital Information System (PHIS) database Clinical and billing data on > 6 million hospitalized children 35 free-standing children’s hospitals January 1, 2000 – June 30, 2005 Methods Definition of AO: ICD9-codes for AO and osteomyelitis unspecified Exposure IV group – placement of a catheter PO group – no procedure code for placement of a catheter Exclusion Criteria Hospitalized for chronic osteo in previous 6 mos. Hospitals with data validity issues (35 29) Presence of comorbid conditions on index or prior admissions. Diagnoses suggestive of complicated disease Arthritis, sacroilitis, cellulitis, congenital bone diseases, post-operative wounds, placement of prosthetic devices Length of stay > 10 days Validation of Exposure 10% sample of osteo patients at each hospital 19 of 29 agreed to participate Chart review to confirm classification as PO or IV Primary Outcome Treatment failure within 6 months of diagnosis Chronic osteomyelitis Musculoskeletal surgery Complication of acute osteo (e.g. arthritis, etc) AO as sole readmission diagnosis Secondary Outcomes Any readmission in 6 months Catheter-related complication Adverse effect of antimicrobial therapy C. difficile infection Agranulocytosis Analysis Descriptive Statistics Multivariate Logistic Regression Analysis Propensity Score to adjust for confounding Adjustment for clustering (intrahospital and interhospital variability) Assembly of Study Cohort Osteomyelitis ICD-9 code N=6348 Hospital data issues N=1056 N=5292 Inadequate follow-up N=1136 N=4156 Co-morbid conditions N=1848 N=2308 LOS 10 days N=339 Osteomyelitis cohort N=1969 Demographic and Clinical Characteristics Antimicrobial Therapy 45 40 35 30 25 IV PO 20 15 10 5 0 1st Ceph Clinda Ox/Naf Vanco Variability in utilization of early conversion to oral antimicrobial therapy 100 90 Converted to oral therapy (%) 80 70 60 50 40 30 20 10 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 Hospital Treatment Outcomes of AO Results: Validation Study 19 of 29 hospitals participated in validation 13 of 19 had no missclassification 6 hospitals had patients treated with IV but were assigned to oral therapy Repeated analyses: for 13 hospitals with no misclassification OR 0.74 (0.21, 2.6) 16 hospitals that did not participate or had misclassification OR 0.71 (0.37, 1.4) Strengths and Limitations Strengths Large sample size multiple hospitals validation of exposure Limitations Not randomized Miscoded or inaccurate information Misclassification of outcome Preconditions for oral therapy not evaluated Conclusions Early conversion to oral therapy is safe and effective for the treatment of uncomplicated AO Consideration to developing a clinical practice guideline reduce variation in practice Determine if good clinical outcomes are sustained Types of Error Random (chance) Evaluation by statistics Statistics only deal with problems of chance Systematic Bias Selection Information Information Bias Information (misclassification) Misclassify IV as PO or vice versa Misclassify treatment failures as non-failures or vice versa What is the direction of the bias? Nondifferential misclassification Differential misclassification Implications of Direction of Bias STUDY EFFECT DIRECTION OF BIAS Yes Toward Null No Toward Null Yes Away from Null No Away from Null IMPLICATION Real effect even stronger Might have missed real effect Spurious conclusion Really nothing going on Acknowledgements Ron Keren, MD, MPH Russell Localio, PhD Kateri Leckerman, MS Stephanie Saddlemire, MPH Priya Prasad, MPH Sarah Smathers, MPH