Hypothalamus & Pituitary
advertisement

Hypothalamus & Pituitary
Felix E. Grissom, Ph.D.
Department of Physiology & Biophysics
2219 Adams Building
Tel (202) 806-4512
Figure 11-3: Autonomic control centers in the brain
Hypothalamus
• Integrates functions that maintain chemical
and temperature homeostasis
• Functions with the limbic system
• Controls the release of hormones from the
anterior and posterior pituitary
Hypothalamus
• Synthesizes releasing hormones in cell bodies of
neurons
• Hormones are transported down the axon and
stored in the nerve endings
• Hormones are released in pulses
Hypothalamic Releasing Hormones
Seven releasing hormones are made in the
hypothalamus
–
–
–
–
–
–
–
Thyrotropin-releasing hormone (TRH)
Corticotropin-releasing hormone (CRH)
Gonadotropin-releasing hormone (GnRH)
Growth hormone-releasing hormone (GHRH)
Growth hormone-release inhibiting hormone (GHIH)
Prolactin-releasing factor (PRF)
Prolactin-inhibiting hormone (PIH)
Hypothalamus Releasing Hormones:
Secretion
• Is influenced by emotions
• Can be influenced by the metabolic state of
the individual
• Delivered to the anterior pituitary via the
hypothalamic-hypophyseal portal system
• Usually initiates a three-hormone sequence
Anterior Pituitary
Is also called the Adenohypophysis
Secretes tropic hormones in a pulsatile fashion
Synthesizes various hormones in various specific cell
populations
Anterior Pituitary Hormones
Each of anterior pituitary hormone is synthesized
by a cell population.
Corticotropes
-
ACTH
Lactotropes
-
Prolactin
Somatotropes
-
GH
Thyrotropes
-
Thyrotropin
Gonadotropes
-
FSH, LH
Anterior Pituitary Hormones
Growth Hormone (GH, Somatotropin): primary
hormone responsible for regulating body growth, and is
important in metabolism
Thyroid-stimulating Hormone (TSH): stimulates
secretion of thyroid hormone & growth of thyroid gland
Adrenocorticotropic Hormone (ACTH): stimulates
cortisol secretion by the adrenal cortex & promotes
growth of adrenal cortex
Anterior Pituitary Hormones
Follicle-stimulating Hormone (FSH): Females:
stimulates growth & development of ovarian follicles,
promotes secretion of estrogen by ovaries.
Males: required for sperm production
Luteinizing Hormone (LH): Females: responsible for
ovulation, formation of corpus luteum in the ovary, and
regulation of ovarian secretion of female sex hormones.
Males: stimulates cell in the testes to secrete testosterone
Prolactin: Females: stimulates breast development and
milk production. Males: involved in testicular function
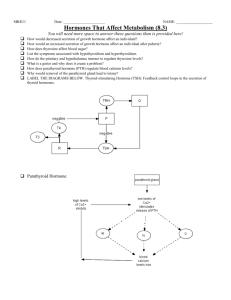
HYPOTHALAMIC
HORMONE
Thyrotropin-releasing hormone
(TRH)
Corticotropin-releasing hormone
(CRH)
Gonadrotropin-releasing
hormone (GnRH)
Growth hormone-releasing
hormone (GHRH)
Growth hormone-inhibiting
hormone (GHIH)
{Prolactin-inhibiting hormone
(PIH)
EFFECTS ON THE
ANTERIOR PITUITARY
Stimulates release of TSH
(thyrotropin) and Prolactin
Stimulates release of ACTH
(corticotropin)
Stimulates release of FSH and
LH (gonadotropins)
Stimulates release of growth
hormone
Inhibits release of growth
hormone
Stimulates release of prolactin
Prolactin-inhibiting hormone
(PIH)
Inhibits release of prolactin
Growth Hormone Activity
Increases plasma free fatty acids (FFA) - source of
energy for muscle tissue
Increases hepatic glucose output
Decreases insulin sensitivity in muscle
Is protein anabolic hormone
Growth Hormone Activity
Exerts its growth-promoting through interactions
[mainly induction of Insulin-like Growth Factor I (IGFI)].
IGF-I synthesis is stimulated by GH
Major source of IGF-I is the liver; IGF-I is also locally
produced in other tissues
Endocrine Control: Three Levels
of Integration
• Hypothalamic stimulation–from CNS
• Pituitary stimulation–from hypothalamic trophic Hs
• Endocrine gland stimulation–from pituitary trophic Hs
Endocrine Control: Three Levels
of Integration
Figure 7-13: Hormones of the hypothalamic-anterior pituitary pathway
Multiple Stimuli for Hormone
Release:
Nervous & Endocrine
• Stimuli
– Stretch
– Glucose
– Insulin levels
• Reflex
– Lower blood glucose
– Reduces stimulus
– Reduces insulin release
Multiple Hormones Can Target a
Cell/Tissue
• Growth Hormone
• Somatomedins
• Thyroxin
– All have receptors
on many tissues
– Stimulate pathways
for growth
Figure 7-17: A complex endocrine pathway
More Impacts on Target Cells
• Synergism: multiple stimuli more than additive
–
–
–
–
Cortisol +5
Glucagon +10
Epinephrine +20 (added = +35)
Synergistic effect + 140
• Antagonism: glucagons opposes insulin
• Permissiveness: need 2nd hormone to get full
expression
More Impacts on Target Cells
Figure 7-18: Synergism
Posterior Pituitary
Comprised of the endings of axons from cell bodies in
the hypothalamus (supraoptic and paraventricular)
Axons pass from the hypothalamus to the posterior
pituitary via the hypothalamohypophysial tract
Posterior pituitary hormones are synthesized in the
cell bodies of neurons in the supraoptic and
paraventricular nuclei
Posterior Pituitary
Hormones synthesized in the hypothalamus are
transported down the axons to the endings in the posterior
pituitary
Hormones are stored in vesicles in the posterior pituitary
until release into the circulation
Principal Hormones: Vasopressin & Oxytocin
Secretion of Posterior Pituitary
Hormones
Figure 7-12: Synthesis, storage, and release of posterior pituitary hormones
Oxytocin
Is synthesized as the precursor hormone: preprooxyphysin
Acts primarily on the mammary gland and uterus
Increases contraction of smooth muscle of the vas
deferens
Oxytocin
Secretion is increased during labor
May also act to facilitate sperm transport in uterus
(non-pregnancy state)
Posterior Pituitary: Regulation of Osmolality
Plasma osmolality is monitored by osmoreceptors in the
hypothalamus
Increases in plasma osmolality stimulates secretion of
vasopressin
Small changes above the normal plasma osmotic pressure
(285 mosm/kg) stimulate release of vasopressin
Vasopressin (ADH)
Is also known as antiduretic hormone (ADH)
Participates in body water regulation (Water is lost
from lungs, sweat, feces and urine on a daily basis)
Osmolality
• Refers to the amount of solutes in a solution
• Loss or gain of water without solutes (free water
gain or loss) changes the osmolality of ECF
• Must be regulated to maintain normal cell activity
Vasopressin (ADH) Secretion
Secretion is Stimulated by:
1.
Large decreases in blood volume
2.
Decreases in blood pressure
3.
Pain, fear, trauma, and stress
Vasopressin Activity
Decreases water excretion by kidneys (V2 receptors)
Constricts blood vessels (V1 receptors)- arteriolar smooth
muscle
Increases adrenocorticortropin hormone (V1B receptors)
secretion from the anterior pituitary
Negative Feedback Controls:
Long & Short Loop Reflexes
Figure 7-14: Negative
feedback loops in the
hypothalamic-anterior
pituitary pathway
Negative Feedback Controls:
Long & Short Loop Reflexes
Figure 7-15: Control pathway for cortisol secretion
Pathologies: Over or Under
Production
• "no bad hormones – just too much or too little"
• Exogenous medication
– Replaces & exceeds normal
– Cause atrophy of gland
• Hypersecretion: too much
– Tumors or cancer
– Grave's disease- thyroxin
• Hyposecretion: too little
– Goiter – thyroxin
– Diabetes – insulin
Pathologies: Over or Under
Production
Figure 7-19: Negative feedback by exogenous cortisol
Pathologies: Due to Receptors
• Downregulation – hyperinsulinemia
• Transduction abnormalities
– Testicular feminization syndrome
– Pseudohypothyroidism
• Abnormalities of control mechanisms
Pathologies: Due to Receptors
Figure 7-20: Primary and secondary hypersecretion of cortisol