PBL+BloodOnTheRoad final
advertisement

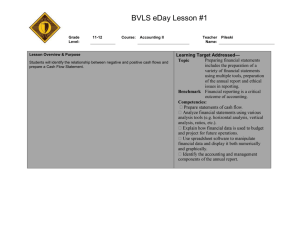
Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL ONE TUTORIAL 1 : TRIGGER 1 PRESENTATION It is 10.30 pm on a Friday night, when two medical students see the car ahead of them run off the road and crash into a tree. They stop and run to the scene. A young male, covered in blood, is struggling to get out of the driver's seat of his wrecked car. There is blood spurting from a wound in his left thigh. "What should we do?" Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL ONE TUTORIAL 1: TRIGGER 2 FIRST AID & INITIAL EXAMINATION The students have moved the driver, Mark B., away from the wrecked car. He is bleeding profusely from the wound in his left thigh. One of the students manages to control the bleeding by pressing on the open wound with his hands. Throughout, Mark is conscious and complains of feeling thirsty and cold. An ambulance and the police arrive soon after. On examination, he is conscious but confused, groaning in pain and complaining of difficulty breathing. Other observations are: - systolic BP 70 mmHg (diastolic too low to measure) - Pulse 135/min, thready - respiratory rate 30/minute - airway intact - chest extensively bruised and tender - deformity of the left thigh with substantial bleeding - numerous bruises and lacerations of both lower limbs - extreme pallor - pale face, conjunctiva and palmar creases - and cold, sweaty extremities - no obvious head injury, no neck pain, pupils equal and reactive to light. Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL ONE TUTORIAL 1: TRIGGER 3 INITIAL TREATMENT The ambulance officers provide oxygen therapy and begin an intravenous infusion. One of them says “This is the fourth accident we’ve been called out to this week.” They set off on the twenty minute journey to the nearest country hospital. One of the medical students accompanies the patient in the ambulance. "What is the best IV fluid to start with? Is he going to bleed more if we give him a lot of fluid?" asks the student. Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL TWO TUTORIAL 2 : TRIGGER 1 EMERGENCY DEPARTMENT History &Assessment Mark’s brother, Paul, arrives at the hospital shortly after Mark is brought into A&E. Paul states that Mark is 19 years old. He usually works as a barman but is currently unemployed. He smokes 30 cigarettes a day. He is a binge drinker, taking as much as 200 grams of alcohol (20 standard drinks) in a single sitting, once or twice weekly. Mark’s father also has a history of heavy alcohol consumption. On assessment in Emergency, Mark is found to have a compound fracture of the left femur with partial laceration of the left femoral artery. His blood alcohol level is 0.18 g/dl. He has no significant past medical history and subsequently proves negative for HIV, hepatitis B and C. Y1W1&2_ Blood on the Road What we know Trigger 1 (above) Admitted to ED (Paul’s brother arrived) Mark, 19 Worked as barman, now unemployed Smokes 30 cigarettes Binge drinker (200 g/20 standard drinks per session, once or twice a week) Father has history of heavy alcohol consumption On assessment in Emergency – compound fracture of left femur, partial laceration of left femoral artery Needs to go to the OR BAL 0.18 g/dl Normal alcohol level 0.05 Can’t anaesthetise (alcohol CNS depressant) No significant past medical history Negative for HIV, Hepatitis B &C Trigger 2 Vital signs not improving Haemopneumothorax seen on erect CXR What we need to know Trigger 3 Open chest surgery – repair lac to left main bronchus & a TRIGGERS MED 1000 Hypotheses How BAL relates to risk of having MVA (RTA – Driver Qualification Test) http://www.rta.nsw.gov.au/licens ing/downloads/driver_qualificatio n_handbook.pdf exponential relationship between relative crash risk & BAC Age & sex related risks to having MVA In above website Does he abuse other illicit drugs? Is alcohol hypo/hyper/isotonic The effect of alcohol on the body E.g. immune system (chemotaxis), cardiovascular system, etc Can we control bleeding & wait? At what BAL can we do Sx (surgery)? Should we give antibiotics or tetanus immunisation? Alcohol impairs immune system Chest X-ray (CXR) GCS score Abdominal assessment What is a haemopneumothorax? Different opacities in CXR Darkest thing is air (black – lungs are nearly black) Grey (darker grey is fatty tissues, lighter grey is muscles) Calcified tissues or bones Very white – metal objects CXR Right side of patient is your left side Normal – lungs, should be able to count 9 ribs (taken with full inhalation) Pt – darker due to compressed air Emphysema – lungs will be darker (air trapped in the lungs, blood/air contact surface area destroyed, i.e. alveoli) Gastric bubble – normal on left side, always abnormal on right side (liver) Could patient have a different type of shock? (e.g. septic shock) Septic shock (infection) – does he Ribs have punctured the lung Septic shock How it happens? Y1W1&2_ Blood on the Road pulmonary vein Large intravenous fluid replacement (plasma expander, blood), not stabilised before surgery (accumulating blood & air in pleural space, ongoing blood loss) Profound hypotension in surgery (fluid replacement unable to keep up with losses) Surgery also included stabilization of fractures Anaethetist says – not keeping ahead of this guy’s losses Pulse 120 Systolic BP (SBP) 90 Peripheral perfusion is poor Have we missed something? TRIGGERS have a fever? Compensatory mechanisms in shock Detected by baroreceptors Renin-angiotensin-aldosterone cycle Not working! From a certain level onwards, compensatory mechanisms can damage the body Mechanisms of shock How do we assess adequacy of fluid replacement? Vital signs – HR, resp rate, skin colour Urine output – normal/increased/decreased? Prophylactic (preventative) antibiotics? Generally not used, unless there are specific requirements (e.g. orthopaedic surgery – high risk of infection) Not used if surgery is completely clean/sterile Prophylactic antibiotics will increase antibiotic resistance Losing fluid – from where? Check urine for blood? Bleeding from abdomen? Pt doesn’t have clinical signs Oedema? What is affecting blood pressure? Is it affecting contractility of the heart Cardiogenic shock Preload & afterload Is the preload affected or not? Afterload is probably not enough (BP low, pulse high) Look at pressure inside veins – JVP JVP high – cardiogenic shock MED 1000 What is it? More third spacing? Blood not returning to heart – blockage? Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL TWO TUTORIAL 2 : TRIGGER 2 EMERGENCY (cont’d) Investigations Despite extensive fluid replacement, Mark’s vital signs are not improving. A chest X-ray taken in the supine position is hard to interpret. He is propped up and another film taken in the erect posture. X-ray shows a haemopneumothorax Y1W1&2_ Blood on the Road (see below for a normal chest x-ray for comparison) TRIGGERS MED 1000 Y1W1&2_ Blood on the Road TRIGGERS MED 1000 Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL TWO TUTORIAL 2 : TRIGGER 3 SURGERY Mark requires open chest surgery to repair lacerations to his left main bronchus and a pulmonary vein. Despite being given large volumes of intravenous fluid replacement (plasma volume expander and then blood as soon as it was available from cross matching), he could not be stabilised before surgery because of accumulating blood and air in the pleural space, and ongoing blood loss. During surgery, he continued to experience episodes of profound hypotension as fluid replacement was unable to keep up with the losses. As Mark is recovering consciousness after the surgery, which also included stabilisation of his fractures, the anaesthetist says "We are still not keeping ahead of this guy's losses. His pulse is about 120, systolic BP only 90 and his peripheral perfusion is poor. Have we missed something?" Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL THREE Tutorial 3 : Trigger 1 POST-OP Mark's central venous pressure is monitored while his fluid replacement continues. The anaesthetist, who is also the hospital's intensivist, says "That is about as high as we dare bring up the CVP. I wish we had a pulmonary wedge pressure (PWP) to get the left ventricular filling pressure!" Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL THREE TUTORIAL 3 : TRIGGER 2 PROGRESS Mark's arterial blood pressure comes up to around 105/85, with pulse rate of 96 per min. "Is he out of the woods now?" asks the student. "After such a long period of hypotension, the worry is that he will deteriorate from now on into irreversible shock no matter what we do..." Echocardiography does not show any mechanical damage to the myocardium or heart valves, but indicates that his left ventricular ejection fraction is down to 31%. When asked how bad this was the anaesthetist comments: "It could be worse, but much below that they don't make it." Y1W1&2_ Blood on the Road TRIGGERS MED 1000 TUTORIAL FOUR TUTORIAL 4 : TRIGGER 1 Eight hours after his crash, Mark is in a serious but stable condition. He is transferred to a metropolitan hospital. Arterial pressure: measure what the pressure is on arterial vessels- so what the pressure is that the ventricles feel when ejecting blood. This will drop from the aorta to the capillaries. Filling Pressure: Pressure in the right atrium- Differential only relevent when there is low volume. When the heart pumps normally – need to have blood to pump from the atrium. Low filling pressure – not much blood Measure CVP in the right atria: Pressure of the blood returning to the heart. How the veins get pressure- big veins taking a breath (intrathoracic pressure), some have their own arteries that are contracting, muscle pumps, valves. Central venous pressure – not peripheral – final stage = right atrial pressure. Atrioventricular (Mitral and Tricuspid) Valves open because attached to the heart muscles and will contract when the heart contracts- doesn’t happen due to pressure. Even if the heart was empty the valves would still open. Valves are in the lower vena cava but not in the superior vena cava. Don’t need valves in the superior vena cava because of gravity. No valves between the inferior vena cava and the right atrium because there are valves within in the vein itself. If everything is working properly there should be the same pressure in the superior and inferior vena cava but when considering CVP we measure from the right atrium. CVP: The pressure of the blood within the superior and inferior vena cava, depressed in circulatory shock and deficiencies of circulating blood volume, and increased with cardiac failure and congestion of circulation. Mean circulatory filling pressure a measure of the average (arterial and venous) pressure necessary to cause filling of the circulation with blood; it varies with blood volume and is directly proportional to the rate of venous return and thus to cardiac output Heart is at more risk during shock than other organs because it is working harder (tachycardia) and therefore needs more O2 but there is less available. – A reason why shock can become irreversible. Heart can suffer ischaemia because works harder but there is not enough oxygen to keep up with needs. Ischaemia= reversible Y1W1&2_ Blood on the Road TRIGGERS MED 1000 Necrosis= ireversible 6 hours to cause permanent damage through to the whole wall. PE can be an explanation of irreversible shock- many different explanations of irreversible shock.