Exercise for Dialysis Patients
advertisement

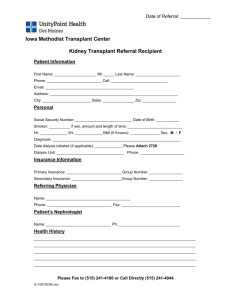
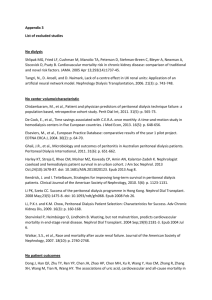
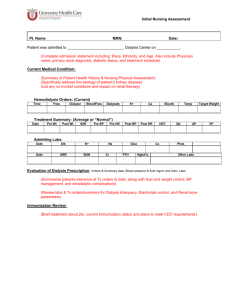
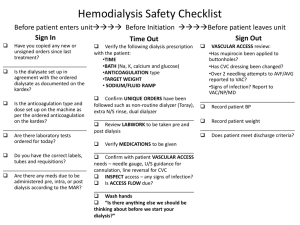
Exercise for Dialysis Patients Amanda Newberry, M.Ed. Exercise Physiologist University of Virginia Renal Services CRN Meeting November 2010 Objectives To provide knowledge and supporting data on benefits of intradialytic exercise To encourage incorporating exercise into routine patient care plan To provide information on beginning a unit based exercise program To describe the procedures and operations of a current unit based exercise program Physical Functioning The ability of an individual to perform activities required in their daily lives. PF of dialysis patients is LOW! Self-Reported Physical Functioning Scale Scores Results from SF-36 Questionnaire 100 84 80 56 60 69 50 50 40 20 0 Gen Pop 1. Ware et al: Health Institute; 1994 COPD CHF Post MI HD maximal oxygen uptake (ml/kg/min) Oxygen Uptake in Adult Hemodialysis Patients* 50 Untrained 40 30 sedentary normal males sedentary normal females 20 10 (*Average VO2peak in 14 studies - pre EPO) 0 20 30 40 50 age Used with permission from P. Painter, PhD 60 70 Measures of Physical Functioning Short Physical Performance Battery • Gait speed (4 meters) • Sit to stand (time for 5 ) • Standing balance tests Other measures • 6 min walk test Sit to Stand to Sit Test 30 p=.004 Seconds* 28 26 24 intervention no intervention 22 20 Baseline Post I nd. Post Inctr. * seconds taken to stand up and sit down 10 times 2. Rex Demonstration Project Painter, et al: AJKD 35(3): 482-492, 2000 Physical Inactivity leads to… Overall decline in physical well-being Poor physical performance Fluid build up in tissues Loss of bone strength Loss of appetite Muscle wasting Hypertension Dependence Fatigue Relationship between sedentary behavior/low CRF and higher mortality among patients with ESRD 3. Johansen K L: JASN Express, 2007 Benefits Physiological Benefits Reduced risk of cardiovascular mortality Decreased use of antihypertensive medications Favorable adaptation of body composition Reduced C-reactive protein/increased albumin Improved removal of toxins by dialysis Improved exercise capacity Improved blood pressure control Improved lipid profile • Esp increased HDL and reduced TG Increased hematocrit • Prior to EPO therapy Improved glucose regulation Psychological Benefits Reduced subjective fatigue symptoms Improved perception of physical functioning Improved perception of general health Reduced anxiety Improved mental health Reduced experience of bodily pain Increased vitality Improved psychological profile • Reduced anxiety, hostility, and depression, and increased participation in pleasant activities Functional Benefits Improved muscle strength Increased 6-min walk distance Reduced risk of falls in the elderly Maintenance of independence Clearance During dialysis: • Urea removed from blood • Urea retained in peripheral body compartments • Urea and creatinine distributed in body water • Muscle water content high • Muscle mass = ~40-45% total body weight • Much of solute mass will be held within muscles • Some body tissue is unexposed to dialysis 4. Kong, et al: Nephrol Dial Transplant. 1999; 14: 2927-2931. Clearance After dialysis: With exercise: • Urea re-equilibrates and a rebound results • Limits the efficiency of dialysis • Muscle blood flow increases • Potential increase from 3-4ml/min per 100g to 80ml/min per 100g • More tissue mass is exposed to the dialysis treatment 4. Kong, et al: Nephrol Dial Transplant. 1999; 14: 2927-2931. Improved urea Kt/V with exercise 4. Kong, et al: Nephrol Dial Transplant. 1999; 14: 2927-2931. Cramping Timing of exercise Type of exercise Intensity of exercise Start slowly, Progress gradually!!! Exercise: A Vital Sign Exercise Rx Surgeon General’s report: “significant health benefits can be obtained by including a moderate amount of physical activity….on most, if not all, days of the week”. American College of Sports Medicine (ACSM) “Exercise Prescription: every patient, every visit, every time” www.exerciseismedicine.org Exercise is MedicineTM Guiding principles: • • • Exercise and physical activity are important to health and the prevention and treatment of many chronic diseases More should be done to address physical activity and exercise in healthcare settings ACSM and AMA are making efforts to bring a greater focus on physical activity and exercise in healthcare settings Program Implementation New Program Resources Life Options Rehabilitation Advisory Council (LORAC)5 • “Exercise for the Dialysis Patient” • A Guide for the Dialysis Team • Author: Patricia Painter, PhD Staff Responsibility to Exercise • Carlson L, Carey S. ACKD Vol 6, No 2 pp172180, 19996 Steps to developing an exercise program Gaining staff support • Edu/inservice • Case presentations Commitment to developing a program • Group input • Assurance of willingness of staff to participate Assess available resources • Staff interest • Teamwork • Interested patients • Local programs 6. Carlson L, Carey S. ACKD, 1999 Steps to developing an exercise program Develop a program • Smaller working groups (care planning, motivation/education, exercise programming) • Staff responsibilities identified • Facilitate a sense of ownership amongst staff Start program • Start slowly (one shift, one bay, interested pts) • Progress gradually Ongoing evaluation • CQI • Patient reassessment 6. Carlson L, Carey S. ACKD, 1999 • Patient programs UVA SitFit Exercise Program 8 Units 800 patients 50% patient participation 78% exercise compliance UVA SitFit Exercise Program One Exercise Physiologist Exercise Leader at each unit • Technician or RN Monthly QAPI Reports Monthly Compliance Reports Quarterly Exercise Team meetings Beyond the science… Setting expectations Potential for patient to exercise Motivating a non-motivated patient Barriers to Exercise Sickness Fatigue Lack of equipment Lack of motivation Depression Lack of encouragement Most can be resolved through exercise! Influences on Patient Physical Activity Physician Family Patient Physical Activity Health Care System 6. Carlson L, Carey S. ACKD, 1999 Society Health Care Workers Exercise Options Cycle (Monark) Oxystepper Hand Weights Ankle Weights Cycle Arm curls Toe Taps Lower Leg Raises Seated Marching Straight Leg Raises “Rear-End” Squeezes!! Contact Amanda Newberry, M.Ed University of Virginia Renal Services Exercise Program Coordinator • Email: alh9t@virginia.edu • Office: (434)243-6218 1. 2. 3. 4. 5. 6. Ware JE, Kosinski M, Keler SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manuel. 2nd ed. Boston: Health Institute; 1994. Painter P, Carlson L, Carey S, Paul SM, Myll J. Physical functioning and health related quality of life changes with exercise training in hemodialysis patients. Am J Kidney Dis. 2000; 35(3):482-492. Johansen K. Exercise in the End-Stage Renal Disease Population. J Am Soc Nephrol 18: 1845-1854, 2007 Kong C, Tattersall J, Greenwood R, Farrington K. The effect of exercise during haemodialysis on solute removal. Nephrol Dial Transplant. 1999; 14: 2927-2931. Carlson L, Carey S. Staff Responsibility to Exercise. ACKD Vol 6, No 2 (April) pp 172-180, 1999 Life Options Rehabilitation Advisory Council. Exercise: A Guide for the Dialysis Team. 1995; Table 2: pp 7.