Lecture 3 - Home - KSU Faculty Member websites
advertisement

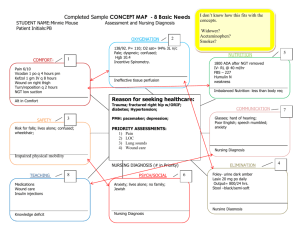
Lecture 3 The Nursing Process in Psychiatric/Mental Health Nursing Assessment Evaluation Implementation Diagnosis Planning Applying Nursing Process Role of the nurse in psychiatry The nurse assists the client’s successful adaptation to stressors within the environment. Goals are directed toward change in thoughts, feelings, and behaviors that are age-appropriate and congruent with local and cultural norms. Diagnosis Diagnosis The Nursing Process The standards of care for psychiatric nursing are written around the five steps of the nursing process. It is a systematic framework for the delivery of nursing care. It uses a problem-solving approach. It is goal-directed, its objective being the delivery of quality client care. The Nursing Process It is dynamic, not static. Within the legal scope of nursing Client-centered Prioritized It is accepted for clinical practice established by the American Nurses Association Standard I. Assessment Standard I. Assessment The psychiatric/mental health nurse collects client health data. Types of Data -Objective data-observable and measurable facts (Signs) -Subjective data-information that only the client feels and can describe (Symptoms) Standard I. Assessment Sources of Data -Primary source: Client -Secondary source: Client’s family, reports, test results, information in current and past medical records, and discussions with other health care workers Standard I. Assessment The data will collect through: Nursing health history (Demographic data, Chief complain, History of present illness, Past psychiatric history, Family history, Life style, Social data, psychological data) Physical examination Mental status examination (Appearance, behavior, speech, mood, affect, intelligence, sensorium, thought) Lab results Review records and literature Nursing health history 1. Demographic data: Client name, address, age, sex, marital status, occupation, religious. 2. Chief complain: The answer given to question "what brought you to the hospital? Nursing health history 3. History of present illness: Basic needs (diet, exercise, sleep, elimination) Eye contact Appearance. Speech Coping patterns Self-esteem Orientation. Nursing health history 4. Past psychiatric history. Childhood illness ,head injury, seizures, and major illnesses. Surgeries Hospitalization. any previous episodes of the presenting complaint The past substance (drug) history. history of abuse sexual history Nursing health history 5. Family history: Genetic component and the biological family history 6. Life style: Personal habits: tobacco, alcohol, coffee, tea. Diet description: high fat diet. High salt. sleep pattern. recreation, hoppies. Nursing health history 7. Social data Family relation ship, friends, support system. Level of education. Occupation history (occupied hazard). Economic status. Home (safety measurement) 8. psychological data: Major stressor, usual coping pattern, communication style. Subjective Data Name and general information about the client Client’s perception of current stressor or problem Current occupational or work situation Any recent difficulty in relationships Any somatic complaints Current or past substance use Interests or activities previously enjoyed Sexual activity or difficulties Objective Data 1. Physical exam 2. Behaviour 3. Mood and affect 4. Awareness 5. Thought processes 6. Appearance 7. Activity 8. Judgment 9. Response to environment 10. Perceptual ability Components of Assessment 1. Appearance Dress, grooming, hygiene, cosmetics, apparent age, posture, facial expression (sad, worried, tense). 2. Behaviour/activity Hyperactivity or hypoactivity, rigid, relaxed, restless, gait and coordination, facial grimacing, mannerisms, passive, combative, bizarre. Components of Assessment 3. Mood and affect Mood (Intensity depth duration):- sad, fearful, depressed, angry, anxious, happy, grandiose, nervous, confusion. Affect (Intensity depth duration) :- appropriate, apathetic, constricted, flat, euphoric. 4. Perception Hallucination, illusions, derealization Components of Assessment 5. Attitude Interactions with interviewer: - Cooperative, resistive, friendly, hostile Speech-Quantity: - poverty of speech, poverty of content, volume. Quality: - articulate, congruent, talkative, repetitious, spontaneous, circumstantial Rate:-slowed, rapid Components of Assessment 6. Thoughts Form and content-logical vs. illogical, loose associations, flight of ideas, blocking, neologisms, obsessions, delusions Hallucinations: sensory perception that occur in the absence of an actual external stimulai. Delusion: fixed falls belief. Components of Assessment 7. Cognition Level of consciousness, orientation, attention span, , recent and remote memory, concentration, ability to comprehend and process information, intelligence 8. Judgment Ability to assess and evaluate situations, makes rational decisions, understand consequence of behaviour, and take responsibly for actions Components of Assessment 9. Insight Ability to perceive and understand the cause and nature of own and other’s situation 10. Psychosocial Criteria Internal:-Psychiatric or medical illness, perceived loss such as loss of self concept/self-esteem External:-Actual loss, e.g. death of loved ones, diverse, job or financial loss, retirement Components of Assessment 11. Coping skills Adaptation to internal and external stressors, use of functional, adaptive coping mechanisms, and techniques, management of activities of daily living 12. Relationships Attainment and maintenance of satisfying, interpersonal relationships congruent with developmental stages, including sexual relationship as appropriate for age and status Components of Assessment 13. Cultural Ability to adapt and conform to present norms, rules, ethics. 14. Spiritual (Value-belief) Presence of self-satisfying value-belief system that the individual regards as right, desirable, and comforting 15. Occupational Congruent with developmental stages and societal standards (work, school and recreation) Standard II. Diagnosis Standard II. Diagnosis The psychiatric/mental health nurse analyzes the assessment data in determining diagnosis The purpose of this stage is to identify the patient's nursing problem Standard II. Diagnosis Nursing diagnosis: actual or potential health problems that can be managed by independent nursing interventions . Prioritize the problems Not a medical diagnosis Nursing Diagnosis Categories: -Actual -Potential Standard II. Diagnosis It contains three parts: Problem: Name of the health-related issue or problem as identified in the NANDA list Etiology: (its cause) Sign and symptom It called PES system. The name of the nursing diagnosis is linked to the etiology with the phrase “related to,” and the signs and symptoms are identified with the phrase “as manifested (or evidenced) by” Standard II. Diagnosis Writing Diagnostic Statements Problem Related Diagnostic Label To Etiology As Signs & manifested Symptoms By Standard II. Diagnosis Difference Between Nursing and Medical Diagnosis Nursing Diagnosis- statement used to describe the client's actual or potential response to a health problem that a nurse is licensed and competent to treat Medical Diagnosis- physician "clinical judgment of the disease- i.e. diabetes mellitus. Standard II. Diagnosis Example: If a patient is making statements about dying, he is isolative, anorexic, cannot sleep and wants to die. Then the nursing diagnosis can be: 1. Helplessness, related to physical complaints, as evidenced by decreased appetite and verbal cues indicating despondency. 2. Fatigue related to insomnia, as evidenced by an increases in physical complaints and disinterest in surroundings. Standard III. Planning The psychiatric/mental health nurse develops a plan of care that is negotiated among the client, nurse, family, and healthcare team and prescribes evidence-based interventions to attain expected outcomes. Determine problems that require immediate action Standard III. Planning Short-Term Goals Outcomes achievable in a few days or 1 week Developed form the problem portion of the diagnostic statement Client-centered Measurable Realistic Accompanied by a target date Standard III. Planning Long-Term Goals Desirable outcomes that take weeks or months to accomplish for client’s with chronic health problems Standard III. Planning Formula for Writing Goals: Goal statement (long or short term) = patient behavior + criteria + time + conditions (if needed) 1. Subject -patient 2. Verb -action/behavior which pt performs 3. Criteria -acceptable performance 4. Within specified time period 5. Condition (if needed) circumstances under which behavior performed Example: The patient (1) will walk (2) the length of the hall (3) with a walker (5) by the end of the shift (4). Standard III. Planning Priorities are classified: High: nursing diagnosis that if untreated, could result in harm to the client or others have the highest priority Intermediate: nursing diagnosis involves the nonemergency, non-life threatening needs of the clients Low: nursing diagnosis are client’s needs that may not be directly to a specific illness or prognosis Standard IV. Implementation The psychiatric/mental health nurse implements the interventions identified in the plan of care. Nursing interventions are directed at eliminating the etiologies. Carrying out the plan of care Standard IV. Implementation Nursing interventions must be safe, within the legal scope of nursing practice, and compatible with medical orders. The nurse implements medical orders and nursing orders Nurses are accountable for carrying out nursing orders and physician orders. Standard IV. Implementation Direct interventions : Actions performed through interaction with clients. Indirect interventions : Actions performed away from the client, on behalf of a client or group of clients. Standard IV. Implementation Specific interventions: Standard IVa. Counseling: to assist clients in improving coping skills and preventing mental illness and disability Standard IVb. Milieu therapy: to provide and maintain a therapeutic environment for client Standard IV. Implementation Standard IVc. Self-care activities: To foster independence and mental and physical well-being Standard IVd. Psychobiological interventions: To restore the client’s health and prevent further disability Standard IVe. Health teaching: To assist clients in achieving satisfying, productive, and healthy patterns of living Standard IV. Implementation Standard IVf. Case management: To coordinate comprehensive health services and ensure continuity of care Standard IVg. Health promotion and health maintenance: Implements strategies with clients to promote and maintain mental health and prevent mental illness Standard IV. Implementation Standard IVh. Psychotherapy: provides therapy for individuals, groups and families to foster mental health and prevent disability Standard IVi. Prescriptive authority and treatment: provides pharmacological intervention, in accordance with laws and regulations, to treat symptoms of psychiatric illness and improve functional health status Standard IV. Implementation Standard IVj. Consultation: provides consultation to enhance the abilities of other clinicians to provide services for clients and effect change in the system Standard V. Evaluation The psychiatric/mental health nurse evaluates the client’s progress in attaining expected outcomes. The way nurses determine whether a client has reached a goal. Standard V. Evaluation It is the analysis of the client’s response, evaluation helps to determine the effectiveness of nursing care. Examples: The goal met. The goal not met. The goal partially met. Example Nursing Diagnosis: Self-care deficit (grooming, dressing, and feeding) related to hyperactivity, difficulty in concentrating and making decisions, as evidenced by inappropriate dress, and dysfunctional eating habits. Goal: Patient will dress appropriately for age and status Nursing intervention: Offer assistance for selecting clothing and grooming to provide input and direction for appropriateness of dress and hygiene to preserve selfesteem and avoid embracement. Evaluation: Patient dresses self appropriately and maintains hygiene. Documentation of the Nursing Process Documentation of the steps of the nursing process is often considered as evidence in determining certain cases of negligence by nurses. Documentation of the Nursing Process (cont.) Examples of documentation that reflect use of the nursing process Problem-Oriented Recording (POR) Has a list of problems as its basis Uses subjective, objective, assessment, plan, intervention, and evaluation (SOAPIE) format Documentation of the Nursing Process (cont.) Focus Charting Main perspective is to choose a “focus” for documentation. A focus may be a nursing diagnosis a current client concern or behavior a significant change in the client’s status or behavior a significant event in the client’s therapy The focus cannot be a medical diagnosis. It uses data, action, and response (DAR) format. Documentation of the Nursing Process (cont.) APIE method Utilizes flow sheets as accompanying documentation Uses assessment, problem, intervention, and evaluation (APIE) format