Perioperative Care of the Bariatric Patient
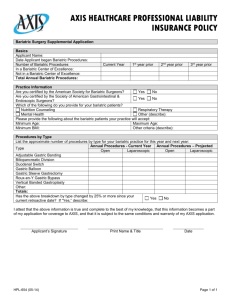
advertisement

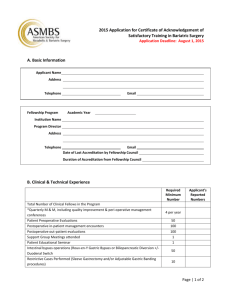
Perioperative Care of the Bariatric Patient Mark Kadowaki, MD, FACS Wellmont Surgical Services Kingsport, Tenessee Objectives Be familiar with the perioperative concerns that face the bariatric patient Be aware of the signs of complications after bariatric surgery Plan for initial management and stabilization of the patient suffering postoperative complications Bariatric Procedures WWW.ASMBS.ORG Bariatric Surgery: Postoperative Concerns http://s3.amazonaws.com/publicASMBS/GuidelinesStateme nts/Guidelines/asbs_bspc.pdf Emergency Care of the Bariatric Patient http://s3.amazonaws.com/publicASMBS/ASMBS_Store/ ASMBS_ER_Poster9-20-10.pdf Download the poster for your Emergency Department or Acute Care Clinic Pre-Surgical Psychological Assessment Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient http://s3.amazonaws.com/publicASMBS/GuidelinesStatements/Guideli nes/PsychPreSurgicalAssessment.pdf http://s3.amazonaws.com/publicASMBS/GuidelinesStatements/Guideli nes/aace-tos-asmbs.pdf ASMBS Allied Health Nutritional Guidelines for the Surgical Weight Loss Patient http://s3.amazonaws.com/publicASMBS/GuidelinesStatements/Guideli nes/bgs_final.pdf Non-Emergent Concerns RNY Gastric Bypass and Dumping Syndrome Common “side effect” (85%) Essentially a known result of the anatomic changes associated with the surgery Can range from mild to severe Rapid emptying of the gastric pouch of refined sugars (HFCS) or other high glycemic carbohydrates or other osmotically concentrated foods, such as dairy products and some fats such as fried foods “Benefit” of Dumping Syndrome Negative feedback Causative foods will interfere with success of long-term weight loss Patient is less likely to eat the same foods again Bad effects of Dumping Symptomatically uncomfortable Confusion with other etiologies Can be difficult to manage May have short-term physiological consequences Two Types of Dumping Early: 30-60 minutes Duration up to 60 minutes Osmotic symptoms: sweating, flushing, lightheadedness, tachycardia, palpitations, desire to lay down, upper abdominal fullness, nausea, diarrhea, cramping, active, audible bowel sounds Caused by release of gut hormones with vasoactive effects Two Types of Dumping Late: 1-3 hours after eating Reactive hypoglycemia symptoms: Sweating, shakiness, loss of concentration, hunger, fainting and passing out Related to insulin surge overshooting glucose levels Diagnosis of Dumping Syndrome History: Classic symptoms related to food intake Management of Dumping Syndrome Early Dietary compliance with an appropriate diet Late Dietary compliance Intake of a small amount of sugar (1/2 glass juice) 1 hour after a meal Acarbose or Somastostatin in resistant cases Rule out rare causes such as insulinoma Bowel Function after Bariatric Surgery Diarrhea Most common with Duodenal Switch procedures Less common with RNY gastric bypass Uncommon with Sleeve gastrectomy or Gastric banding Caused by FAs, undigested foods and Sorbitol (occurs naturally in fruits) Management of Diarrhea Dietary: Avoidance of fats Identify other trigger foods Evaluate for previously unmasked lactose intolerance: eliminate dairy completely Medical: Imodium or Lomotil Probiotics Cholestyramine to bind bile salts C diff Colitis Can occur up to 3 months after surgery Severe cramping, especially watery diarrhea, extremely foul flatus Treat with Flagyl Relapses common Follow up with probiotics Constipation Common after bariatric surgery Causes: Insufficient intake of water Insufficient intake of fiber Diuretics (caffeine?) Nutritional supplements with Calcium and Iron Narcotics Management: Increased water and fiber intake Avoidance of aggravating agents Bowel Changes after Bariatric Surgery Caveat: Don’t assume that all bowel function problems are related to bariatric surgery Recent changes in a previously stable patient Postoperative Dysphagia Most commonly associated with restriction procedures Symptoms: chest pressure or tightness in the throat May be functional: Eating too fast Eating too much Not chewing well enough Tough foods Breads, rice and pastas Overcooked steak or dry chicken breast Postoperative Dysphagia Treatment Better eating habits Failure to respond or severe symptoms Band adjustment (loosening) or endoscopic dilation Postoperative Nutrition Purely restrictive procedures Gastric Banding, Sleeve Gastrectomy, Vertical Banded Gastroplasty Daily multivitamin Monitor protein intake 1 gm protein/kg ideal body weight/day Postoperative Nutrition Primarily Restrictive with some malabsorption Gastric Bypass Calcium, Iron and B-complex vitamins supplemented at higher than daily recommended levels Prioritize protein intake Postoperative Nutrition Primarily Malabsorptive Procedures BPD +/- DS Calcium, Iron Protein Fat Soluble Vitamins (A, D, E, K) Hydration Deficiencies can be resistant to therapy! Nutritional Deficiencies Protein: Calcium Fatigue Zinc Bone pain Iron Hair loss, Fatigue, Leg swelling Brittle nails Vit A Decreased night vision Nutritional Deficiencies Vit E Vit K Easy bruising Vit B1 (thiamine) Poor wound healing Numbness and tingling in hands and feet Vit B12 (Methylcobalamin) fatigue Exercise IMPERATIVE Weight loss will not occur without it 40 minutes per day, 6 days per week, strenuous enough to breathe deeply but still able to converse Light resistance training a benefit Some patients may be “exercise naïve” or even “alienated” Emergent Concerns Emergency Presentations Unstable Vital Signs: Fever > 102 F Hypotension Remember incidence of hypertension Tachycardia >120 bpm X 4 hours Tachypnea Hypoxia Decreased urinary output Emergency Presentations Bleeding Per mouth or rectum or drainage Abdominal pain or colic > 4 hours Nausea + Emesis > 4 hours Emesis + Abdominal pain Principles of Management Critical Time Frames: Diagnosis within 6 hours To OR in 12-24 hours Critical Warnings Alert Bariatric Surgeon Patients typically have less physiologic reserve Avoid blind placement NG tube Avoid NSAIDs, ASA, Plavix, Steroids Use PPIs routinely Be mindful of small volume of gastric pouch Initial Assessment Serial PE and Vitals Labs: CBC, CMP, Amylase Imaging: Chest Xray CT of Chest CT of Abdomen Upper GI Initial Management: FAST HUG Food: establish nutritional support early Analgesia Sedation: if on ventilator Thrombo-embolism prophylaxis Mechanical and Medical Head of Bed: elevated 30 deg (aspiration) Ulcer Prophylaxis: PPIs Glucose Control: <150 Bleeding < 48 hours: staple line > 48 hours: marginal ulcer Oral: gastric pouch Melena or rectal blood: duodenal ulcer, bypassed stomach or bowel source EGD: consider GA in OR Increased risk of perforation with intervention Leaks and Sepsis Presentation: unstable VSs within 72 hours of bariatric surgery Persistent or progressive tachycardia is most sensitive Similar presentation to PE Imaging can be negative Obstruction Presentation: Do NOT place NG tube Diagnostics: Abdominal pain > 4 hours associated with vomiting CT abdo with contrast or UGI Increased risk for aspiration due to small volume of stomach Consider EGD prior to anesthesia to R/O GOO and empty contrast material to decrease risk of aspiration Obstruction Special Concerns: Acute bleed causing obstruction secondary to clots Internal hernias after gastric bypass Evaluation/imaging / PE may be negative Dilated distal stomach or contrast in remnant High risk for closed loop obstruction Bowel ischemic necrosis within 6 hours Immediate surgical exploration Internal hernias A. Transverse Mesocolon B. Petersen Hernia: Beneath Roux limb C. Mesentery defect created by jejunojejonostomy Pulmonary Embolism Extremely high risk patients Unstable vitals associated with chest pain and tachypnea Evaluation with Chest CT Can mimic acute intra-abdominal complication Vomiting + Abdominal Pain Gastric Banding AXR: assess orientation of band Deflate band Huber needle Similar to a Portacath Reassess Does not usually require surgery Adjustable Gastric Band Normal Band orientation 2:00-8:00 Normal orientation but too tight Adjustable Gastric Band Slips Anterior Slip: Band rotated counterclockwise Posterior Slip: Band rotated clockwise Note: enlarged pouch flopping over slip Vomiting + Abdominal Pain Unstable: Immediate surgical exploration Stable: Evaluate per obstruction Barium swallow most useful Abdominal Compartment Syndrome Respiratory failure Renal failure Other end organ failure Elevated bladder pressure (> 25 mmHG) Emergent abdominal decompression “George, how often do you have a leak? “Never had one” “In how many cases?” “Oh, I’ve never done one . . . . .” Surgery for Obesity and Related Diseases 7 (2011) 668 Summary Complications are unavoidable but disasters are often avoidable Be familiar with the perioperative concerns that face the bariatric patient Be aware of the signs of complications after bariatric surgery Plan for initial management and stabilization of the patient facing postoperative complications Early involvement of a Bariatric Surgeon Work with a certified Center of Excellence ASMBS or ACS

![Joel_Bradley_[NCSC_ACS]_Bradley_](http://s3.studylib.net/store/data/007144708_1-61c5732b3c6b9504141b9285237b4b69-300x300.png)