Which psychological factors predict prognosis in CHD?

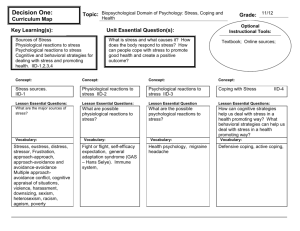
Stress, coping, appraisal & outcome
The basis of Behavior medicine
What is stress for you?
In medicine, reflects “all” psychological states
Used as a “cause” of disease/maladjustment
Used as an “outcome”, reflecting maladjustment
Referring to an event/events (accident)
Referring to an outcome (sweating, depressed)
So what is correct?
In medicine: "if we can't find a physical cause, it must be physiological" wrong!
Can be in parallel, eg. heart attack can occur from anger, but also from atherosclerosis.
confusing cause and effects, giving them the same name.
Any event beyond someone's ability to cope. Everyone rates/appraises this differently.
!!! Stressor <=> stress-response
Definitions of stress
“A negative emotional experience, accompanied by predictable biochemical, physiological, cognitive and behavioral changes, that... are directed either at altering the stressful event or accommodating to its effects”
A. Baum 1990.
“Any event which is appraised as demanding beyond a person’s resources”
(Based on Folkman & Lazarus, 1984)
Problems with the study of stress
Some researchers/clinicians/lay people : stress = an event/trigger
Other researchers/clinicians/lay people: stress = an outcome/response
Solution: distinguish stressor vs. stress-response
Factors inherent in the “event” which affect the stress-response
Intensity (volume, luminance)
Frequency (events/unit of time)
Duration (seconds, minutes, days, months)
Proximity (cm, km, miles)
Valence (positive vs. negative), but...
Ambiguity vs. clarity
1
o Ambiguity: is it clear? Eg you are told to do a b and c, but they expect a b and e, but you don't know this.
Selye’s model of stress
Alarm Resistance Exhaustion
HPA-axis responses following exposure to different stressors => activating the SNS => mobilization
The General Adaptation Syndrome:
Alarm – mobilization to meet the stress
Resistance – confronting the stressor
Exhaustion – failure to overcome the stressor and depletion of physiological resources
Selye's model of stress: everyone, no matter which stressor or species. But, we don't always have a breakdown after every stressor, but his theory said so.
This is actually wrong, it depends on the stressor and multiple factors.
X axis time , y axis resources.
Limitations of Seley’s model
It does not consider psychological aspects of threat: appraisal, personality
It assumes, against evidence, that all stressors lead to the same outcome
2
Factors in the event which depend on “the perceiver”
Importance/relevance to the perceiver
Positivity
Controllability
Predictability
Harmful vs. friendly => These reflect “cognitive appraisal”
Positivity vs negativity: eg pregnancy, it's often positive, but not for a teen.
Appraisal: appreciatie, perceptie, evaluatie
Example of the effects of the APPRAISAL
It is raining while Jo looks through the window
If Jo thinks: “But I wanted to catch some sun”... ⇒ Anger, frustration, disgust
If Jo thinks: “My garden needs water” => Satisfaction, anticipation for growth, etc.
Evidence for the Centrality of the APPRAISAL (Speisman et al., 1965)
Students viewed a film depicting “sub Incision” of a body tissue in a tribe
They were divided into 3 film sound tracks:
Negative appraisal –The kids suffer a lot! Were told it was a horrible film. o it was a horrible film = negative appraisal.
Intellectualization – anthropological focus, was told the facts (old tribe, traditions,...)
Denial/reaction-formation – They like it! Left in denial, they liked the pain, because they would become real men.
During the film they measured the stress response via sympathetic reaction=> DV:
Galvanic-skin response (GSR)
The highest reaction was found in the negative appraisal group. They were led to think about something in a negative way.
The good thing to do for your patients is to look at things in a neutral, objective way.
Not only the negative or positive. This will determine their stress response.
=> An event’s stress-response depends on its inherent nature + one’s cognitive- appraisal
People who see a situation as a challenge react completely differently than those who see it negatively.
What is between stress and adaptation?
(Geen slides van terug te vinden)
Things we do to change the situation, adapt with it, ....
Understanding and solving the situation.
3
Emotion-focused coping: efforts you do to adapt yourself and cope. Not changing the situation.
Problem focused coping: Not all of us go through all the stages, we sometimes fail at some stages. During stress people don't see all the solutions, they have tunnel vision. Serious problem in medicine!
If you only discuss and don't implement the solution, it's not done!
Effects of coping on outcomes depend on context:
Example 1:
Physiological recovery was better in the hospital with high deniers, BUT when we followed them for a year, they did less good than the one's with low denial.
In one situation it was a good thing, but it became bad once they got out of the hospital --> why?
In the hospital: if you're a low denier and stress a lot, your heart rate will rise. A high denier is not thinking so much about the illness and is calmer. He or she thinks the doctors are in charge.
When you release control you do better in the hospital.
Once your out of the hospital, you need lifestyle changes, if you're a high denier you won't change your lifestyle. They still think the doctors are in charge and will Cure them, but they now need to do it themselves.
Example 2:
Many countries were fighting Saddam, one country was told to keep quiet: Israël.
Saddam tried to break this coalition by bombing Israël, in the hope's they would react and the coalition would be broken.
A stress psychologist wanted to see how the children coped during this period.
200kms from you missile is fired and you can't do anything about it but hide in the basements.
The psychologist asked the children what they did once they were in the basement: keep checking everything is closed, the gas masks are one,.... Or telephoning friends and joking around,....
Looked at the psychological symptoms: the one's that did the minimum and then relaxed, joking around etc had less severe symptoms.
Where is the personality?
Studies show that internal impediments and resources also affect the stress, coping and outcome process.
Internal impediments:
Pessimism – negative outcome expectancy
Hostility – Antagonism, cynicism & anger
Negative causal attributions –
“The cause is due to me, it will always be the same cause, and that cause affects everything I do”
4
Where is the person?
Internal resources:
Sense of coherence - SOC: o comprehensibility, manageability & meaningfulness
Self efficacy: “I am capable”
Humour: appreciation & creation
Personality will determine how you will react across situations, quite stable.
Self efficacy: one of the most important predictors for recovery.
Comprehensibility: can i see what happens from year to year?
Social support is very important protector for diseases, help recovery,...
Importance of internal resources for outcome following stress
Example 1:
30 elderly people facing relocation to an old age home were compared to 28 age matched controls.
Movers had lower positive mood and NKCA
But, movers with high SOC had less impaired NKCA than movers with low SOC .
NKCA: natural killer cell activity
To which extent attack the natural killer cells the tumor cells, what is their level of function?
SOC: sense of coherence
Not everyone responded the same, dependent of personal characteristics, eg SOC
Importance of external resources & impediments for outcomes following stress
Categories of social support:
Network size: No. of friends
Function: o emotional support o information support o instrumental support
Example:
1011 US women with breast-cancer were assessed for social support (size & function), and followed for 5 years later.
Those with little emotional support had a higher death-rate than those with much support:
RR = 1.8, CI: = 1.3-2.5
5
Coping = cognitive and behavioral efforts to manage demands that are appraised as taxing or exceeding the resources of a person.
Involves efforts to alter the stressful situation and efforts to regulate the emotional distress associated with the situation
Problem-focused coping (PFC) = Cognitive-behavioral efforts aimed at changing the stressor
Emotion-focused coping (EFC) = Cognitive-behavioral efforts aimed at accommodating to the stressor
Problem-focused coping
(PFC)
Identifying the event/problem
Suggesting solutions
Selecting an “optimal” solution
Implementing a solution
Examining its effects
Types of PFC: planning, consulting, time- management, focusing on a task to be done, implementing active coping
Emotion focused coping
Denial: neglecting existence of stressor
Avoidance - perceptual/cognitive: distraction
Avoidance – behavioral: escape
Humour: Seeing events in different manner
Reappraisal: Changing significance of event
Catastrophizing: Focussing on bad aspects
Support: Seeking emotional support
Effects of coping on outcomes depend on context
45 cardiac patients were assessed for denial in hospital in relation to short-term and long term (1-year) recovery.
IN HOSPITAL, high deniers spent fewer days in ICU & had fewer signs of cardiac dysfunction than low deniers
AFTER DISCHARGE, high deniers complied less and had more rehospitalizations than low deniers!
*Coping and survival from breast- cancer: A prospective study
442 US women with breast-cancer were assessed for coping & followed for 8-9Y
Emotional expression predicted better survival, after controlling for age, tumour stage, study-location and race: HR = 0.6.
Women with low emotional expression AND emotional support were at more risk of death: HR = 2.5.
6
The entire model of stress, appraisal, coping, resources & outcome
Social support is very important protector for diseases, help recovery,...
Graph (niet teruggevonden): people were put in a stressful situation. Some brought a friend, the stress response still went up but a lot less because of the social support.
Model: important!
Event ==> shaping of the event in function of one's appraisal (the way I think about the events will shape it). ==>How do I cope with it? ==>What is the outcome?
Current health also important: if you're sick you give another appraisal to a situation. Also time, money, support and your personality.
Brain – immune communications
7
General biology of stress
Two arms of the stress response:
1) Hypothalamic pituitary axis
2) Sympathetic adrenal medulla: acts faster
Negative feedback loop to turn off the hypothalamus, so you wouldn't keep being stressed.
Modulation of the stress. In a lot of physiological diseases, eg burnout of posttraumatic stress: negative feedback doesn't work anymore.
==> behavioral changes, limited in time.
==> physical changes to stress: oxygen to brain, increase heart rate,...
The 2 arms activate each other
Autoregulatory inhibitory loops via CRH receptors (for CRH) & α-II noradrenergic receptors (for NE)
Both receive o Activating input from serotonin and acetylcholine o Inhibitory input from GABA, opioides and cortisol
Fast response:
– Hypothalamus => Pituitary => SNS => Adrenal medulla => Adrenaline (fight-
Flight)
Slow response:
– Hypothalamus => Pituitary => Adrenal cortex => Cortisol
Internal modulatory circuits
8
From stimulus to response: a neuropsychological model
Brain-to-immune communications: How to study it?
1. Nerve innervation of lymph nodes
2. Receptors for neurotransmitters or neuropeptides on immune cells.
3. Quantitative/Functional changes in immune parameters by CNS & PNS
"Neuroendocrien immuunsysteem": communicatie!
Morphological substrate of brain-to- immune communication
Many studies have documented that immune cells express receptors for neurotransmitters:
Anatomical substrates of brain-to- immune communications
Lymph nodes and organs (e.g., spleen) are innervated by SNS-nervous
These can influence cytokine production and lymphocyte proliferation
CNS Innervation of lymph organs
Samples from 36 lymph nodes of patients were stained for presence of sympathetic nerve fibers
Sympathetic fibres were found in all samples, and in locations suggesting modulation of lymphocyte traffic as well
Functional neuroendocrine modulation of the immune res ponse
Peripheral neutrophils were challenged with tetanus AND EPI OR NE
EPI (and to a lesser extent NE) led to a shift from Th-1-cytokines (lower IFN) to a higher
Th-2-cytokine response (IL-4, IL-5, IL-10)
The SNS influences immune regulation when it faces pathogens!
Norepinephrine can INHIBIT NKCA
Mediated by β2-adrenoceptors
Epi: epinephrine
NE: norepinephrine
--> changed their profile!
Mental state can influence the recovery because the profile of T-cells shifts!!
9
Effects of cortisol on immunity
Cortisol:
Reduces numbers of lymphocytes, monocytes, eosinophils
Reduces trafficking of neutrophils to inflamed sites
Reduces T-cell proliferation & CTL
Reduces monocyte-chemotaxis
Cortisol binds to its GPCR and influences the DNA of the immune cells.
Cortisol supresses the immune system.
The role of higher regions on I/I
The difference between the two hemispheres in relation to the peripheral immune system?
Left hemisphere enhances immunity, the right hemisphere is a neural/immune supressor.
Example:
Two ptns have epilepsy--> laesions.
Purpose: To determine the effects of hemisphere lesions on immunity
Method: 22 epileptic patients underwent left (N=11) or right (N=11) hemisphere resection, and cellular immunity was tested (The needed the surgery in any case...)
Right: left lesions <> red: right lesions
Left: enhancing <> right: less supression
=> The data suggest that an intact left hemisphere is important for intact cellular immunity
=> This is interesting since positive emotional states activate the left hemisphere!
Immune-to-brain communication
Why do you need communication in this direction:, ==> induce fever, enhances immune system and slows down bacteria. Fever is produced in the hypothalamus, which has to learn there is an infection through raised cytokin levels in the blood.
The hypothalamus detects this with a sensor: nervus vagus!
Three ways in which the brain is informed that there is an infection
1.
Places lacking BBB provide opportunity for immune-to-brain influences
2.
On both sides of the BBB, there is a “domino-like response” mediated by prostaglandins
(PGE2), allowing immune information to “influence” the brain
10
3.
The vagus provides an immune-to-nerve conversion of immunological information
Nervus vagus goes to all the visceral regions and has receptors for IL1.
It's main NT is acetylcholine.
Infection producing of cytokines nervus vagus picks this up translating it to a signal in
Ach brain learns there is an infection.
If you vagotomize someone, they don't develop a fever anymore, because they lack this communication.
Fig: amount of IL1 found in the brain following injection of IL1. Hardly any activity in the brain following vagotomy.
Effects of peripheral IL-1 on vagus activity
The role of the amygdala
Another important region is the amygdala.
Why is the amygdala, a region important in processing & in remembering emotional threat, crucial for immune-to-brain communication?
Regulates emotions: anger, anxiety, depression,...
If the amydala was not intact, there was no neuroimmune communication.
11
Hypothesis:
Since the amygdala “remembers” fear ? remembering psychological AND physical threats (fearful faces, antigens)
Subjects getting a vaccine + stress had stronger immune-responses to the pathogen later?
Future studies need to examine whether activity of the amygdala during antigen exposure predicts better immune memory to the same antigen at a later time!
The role of the vagus in neuroimmune relations
Measuring the vagal influence on heart rate by the HRV ( heart rate variability ): look at the Rtops on an ECG.
Divided people in low and high HRV.
Very low HRV can cause sudden death in healthy people. o It is a predictor of it.
If they put these two groups in a stressor, the one's who recovered faster were the one's with high vagal activity --> moderates multiple systems in the body.
The neuroscience of illness: A new avenue in brain-immune communication
How does the brain “learn” about disease? Does this learning modulate disease? Can it be done by CNS-immune pathways?
Vagus keeps inflammation in control, so that it doesn't become systemic.
When vagus reaches a monocyte: monocyte has receptors for Ach, stops producing cytokines.
If you have low vagal activity, you have more severe inflammation.
You can influence the vagus by breathing very slowly, holding you breath for 1-2sec.
12
Predictors and interventions to increase medical adherence
What is adherence?
“the degree to which patients follow the recommendations of their health professionals”
Prevalence of non-adherence
25-50% depending on the medical condition and context.
How to assess patient adherence?
• Drug metabolites
But: half-time life
• Half time life of all medications.: metabolites dissappear, you conclude there is non-adherence, falsely!
• Self-report
But: memory, unawareness, not being honest
• Older people don't remember taking it, too confused.
• Pill count
But were pills taken?
• Disease outcome
Disease may not only be affected by medication! Could be affected by medication, but also by other changes in life.
==> take two or three of these options for different point of views.
Assess patients’ adherence (Morisky, 1986)
– Do you sometimes forget to take medicaiton?
– Are you sometimes careless about medication?
– Do you sometimes decide not to take the medication, when you feel bad after it?
– Do you sometimes decide not to take medication when you feel better?
3 Yes => non-adherent patient
Includes some of the reasons why people don't take their meds
Sometimes: makes it easier to answer yes or no.
Patients generally want to say yes.
Factors that affect non-adherence
• Physician behavior:
Communication content & style
• Disease:
13
Severity, symptomatology, chronicity
• Hypertension: no symptoms, very hard to convince patients to make lifestyle changes
• Diabetes: chronic, you have to be attentive to it all the time, always prepared.
• Patient:
SES, Traits, states, age, gender, education, support
• Treatment
Simple/complex, side effects, costs
Doctors’ communication & patients ’ BP ( Naik et al., 2008)
Purpose of study
To test if doctor-patient communication factors predict BP-control in diabetic patients
Method
N = 212 diabetic hypertensive patients
They completed a measure on their interaction with their doctor
Analyzed words reflecting control, during doctor-patient communication meetings
More words reflecting patient-control predicted better control of hypertension & of diabetes 6 months later!
The more the doctor used the collaborative communicating style (eg what is the BP you first want to reach? What can you reach next time?): patients share control ==> better BP afterwards when doctor had left the room and BP was measured.
Decision control
Doctors who had a lecture on compliance wrote more about compliance in the medical file and their patients were more adherent then those who didn't follow the lecture!
Recorded conversations and counted how many words reflected control by the patients and doctor.
The more words of control of the patient: lower BP!!
14
Health Belief Model (Rosenstock, 1966)
Culture: eg when it is fasting period and they don't want to take meds
Theory of Planned Behavior from Dillon & Morris (1996)
Belief in the treatment: (do they work, do I think it will help).
Normative beliefs : How does my family think about it? What do my surroundings do and think?
Beliefs, perceived control: can I? Can I change or be compliant? Do I have the resources to do this? ==> strongest predictor of outcome.
15
Intentions, brain functions & healthy behaviors (Hall et al.,
2008)
Lower frontal capacity, low planning and behavior control: can't move from intention to planning.
Omgekeerd wel.
Depression, self-efficacy & adherence in HT (Schoenthaler et al., 2009)
Method
Assessed adherence in 167 Black American Hypertensives
Assessed depressive symptoms & self efficacy
Self-efficacy: The belief that you can do a behavior (adhere), despite barriers!
Low self-efficacy: don't follow treatment because they don't think they can keep up with the treatment and are able to do it.
We have to enhance self-efficacy>> how?
Show them other people can do it, bring them in touch. Makes it more real for the patient, talking in their language instead of medical terms.
Talking about the actual situation and how to implement the plans. Identify their barriers and eliminate them.
Barriers for adherence in HT (Vawter et al., 2008)
Main reasons why people had difficulties to take their meds= barriers.
Method
Assessed the reasons (barriers) for non-adherence in 1432 American hypertensives
16
Results
28.4% reported difficulties taking medication
Results – barriers
Forgetting:
Costs:
No insurance:
Side effects
‘There is no need’
32.4%
22.6%
22.4%
12.5%
9.3%
No health provider 4.7%
Do barriers for medication adherence predict non-adherence in cardiac patients? (Wu et al., 2008)
Method
Included N = 134 HF patients
Used an objective measure of adherence:
1.
Dose-count % of prescribed doses taken
2.
Dose-days: % of days the correct number of doses were taken
3.
Dose-time: % of doses that were taken on schedule
Indicator of the MEMS
Significant predictors
P value
R
2
(adj. R
2
)
*
Dose-count a
Barriers < .001 .23 (.20)
Ethnicity .025
**
Dose-day b
Perceived social support
NYHA
.014
.049
Barriers < .001
Financial status .036
†
Dose-time c
Perceived social support
Barriers
.026
.008
Financial status .039
“Our study demonstrated that even after controlling for many other relevant variables, perceived barriers are fundamental to poor adherence.”
Patients’ 5 most frequent barriers:
“forgetting the time of medication”
“not carrying my medication when I am out”
.25 (.21)
.16 (.11)
17
“cost of medication”
“amount of pills that I need to take a day”
“belief that I’ll be fine even though I skip one dose of medication”.
Perceived barriers are fundamental to poor adherence.
Wrong assumption: if we educate people they will change
Exaggerated sentences of people's barriers ==> by amplifying their ideas the people realise their distortion.
Patient have to reject each sentence. You tell them what you'll say is rubbish and they have to reject it.
An intervention to reduce barriers & possibly increase adherence
Psychological inoculation: (PI)
Rationale:
We are exposed to external pressures (& internal ones), for which we often have no reply, and cannot reject!
These pressures form barriers to change behavior!
In Psychological inoculation: (PI) we:
• Expose patients to ‘challenging sentences’ which reflect external & internal barriers, humoristically
• We train patients to refute/reject the sentences!
• We provide them feedback on their refutation
• Voorbeelden:
1.
Cue sentence:
• “Your memory is so poor, you cannot even remember where is your refrigirator at home!”
2.
Refutation sentence:
• “No, no, I know where it is – in the kitchen, of course”
By making the patients reject the exaggerated sentences about the patients' barriers, they realise their own distorted ideas and the cognition changes very fast.
Eg: you don't have 15min a day to work out - but I have 7 children, am a single mother and have a fulltime job...
When they don't reject the sentence, you exaggerate it more (eg 10mins)
Psychological inoculation: Smoking prevention (Evans et al., 1976; 1981)
• Adolescents were forewarned of messages “encouraging” smoking by peers, parents and the media
• They learned and practiced effective counterarguments – refutations
• Received feedback on their performance
• Received booster sessions 25
750 7 th grade children took part in the study
20
15
10
5
0
18
7th grade 8th grade 9th grade
PI
Controls
Smoking was measured
- intentions
- self-report
- nicotine in saliva!
PI: given sentences why they should smoke, they have to reject these and actually learn to say no for themselves'
Controls: normal, smoking is bad etc
The more barriers were changed, the better they carried out their lifestle changed after the treatment.
The stronger the rejection of the sentence, the stronger the lifestyle change.
Study 2: Effects of PI on PA
Method
N= 40 workers in the commune of Zaventem
Randomly assigned to:
HE + SE + PI
Vs.
HE + SE
Exercise for you
Assess patients’ adherence (Morisky, 1986)
• Do you sometimes forget to take medicaiton?
• Are you sometimes careless about medication?
• Do you sometimes decide not to take the medication, when you feel bad after it?
• Do you sometimes decide not to take medication when you feel better?
3 Yes => non-adherent patient
19
Identify patient’s barriers
• What are your reasons for not taking your medication sometimes?
• Internal reasons & external ones
Create “challenging sentences” reflecting those reasons
The sentences reflect the patient’s reasons in an exaggerated humoristic way
Patient Barrier: Side effects:
“So your side effect is surely the WORSE thing you EVER had since you where 4 years old”
Patient Barrier: Memory
“Your memory is so limited, you cannot even remember your phone number!”
Patient refutes sentences and you give feedback
Patient: “Well, no, I remember my phone number, of course..”
Medical trainee: “Good, you refuted my sentence well”.
Guide patient in daily adherence tips
• Put pill reminding stickers on refrigirator
• Put medication near tooth paste
• Ask partner to remind you, sometimes
• Have partner give you “gifts” for full adherence
Stress and immunity
Definitions of stress
“A negative emotional experience,accompanied by predictable biochemical, physiological, cognitive and behavioural changes, that are directed either at altering the stressful event or at accommodating to its effects”
Any event which is appraised as demanding more than a person’s resources
20
The model of stress, appraisal, coping, resources & outcome
(Taylor, 1995)
Overall relations between psychological factors and immunity
Psychological stress is correlated with most immune-factors, especially with activation of viruses
Objective aspects of stress were more strongly correlated with immune factors than subjective aspects
Indirect measurements by seeing how someone projected their own feelings and standards on these photos and situations.
Psychological stress is related to viral activation.
!! What kind of stress, how long,.., --> influences immune system in different ways!!
Example 1: Does prenatal stress affect immunity?
Mothers of piglets were exposed to restraint stress or control at end of pregnancy
T-cell and B-cell proliferations,and morbidity and mortality were tested in neonate piglets
Effect of stress during pregnancy on the baby:
Pregnant pigs were stressed (tied them down for four hours every day, doesn't hurt but immobilizes).
What is the effect on the baby's immune system once they are born?
lower in the babies from the stressed mothers. Disappears afterwards: recovery.
T & B-cell proliferation-indices were lower in prenatally-stressed piglets
Graph: blue= size of thymus gland that produced lymphocytes: smaller in the babies from stressed mothers: anatomical changes!!
21
Effects of pre-natal stress on thymus-weights on neonate piglets
3
2.5
2
1.5
1
Relative Thymus weight (Day1)
Relative Thymus weight (Day 35)
0.5
0
Pre-nata stress Controls
Example 2: Links between psychological stress and immune functioning
Medical students underwent tests for: pro-inflammatory cytokines (IL-6, IFN-γ) and anti-inflammatory cytokines (IL-10).
At 3 time-periods:
Minimal-stress (beginning of term)
High-stress (exams)
Minimal-stress (return from vacation)
How much can they cope with stress:?
Split in high and low stress responding people, looked at pro- and anti-inflammatory levels.
120
100
80
60 Low anxiety
Hi anxiety
40
20
0 mid-term exam vacation
7
6
5
9
8
4
3
2
Low anxiety
Hi anxiety
1
0 mid-term exam vacation
First graph: pro inflammatory
Second graph: anti inflammatory
Different response of immune system in relation to the student life in function of you having low/high anxiety.
22
The effects of uncontrollable stress on immune functioning
The effects of controllable or uncontrollable noise on NK numbers and NKCA and T-cells were examined, as well as the moderating role of personality.
Uncontrollable stress= Harder, because we can't change the situation.
Uncontrollable noise reduced NKCA up to 72 hours after the noise!
Desire to be in control and optimism worsened the effects of uncontrollable noise on
NKCA
Numbers of NK and T-cells were not affected by stressor-type!
People are sitting alone in a room with a box with headphones. You hear a sound trough these, then they turn off. But, there are rooms in which the box doesn't make sound when you press the button, it makes sound based on what the people in other people do with their boxes --> self learned helplessness.
?? What is the effect on the immune system?
Do these people like to have control of give it out of their hands?
Result:
Lower NKCA from uncontrollable noise, worse for the one's with the desire for control and who are optimistic ==> they couldn't cope because they want to be in control but they can't. They try to gain control, but this can't happen.
Example 3: What does home-relocation do to elderly peoples’ immunity?
30 elderly people, before voluntary relocation to old-age homes were compared with 28 age-matched non-moving controls.
They underwent assessment for NKCA, mood and sense of coherence (SOC)
SOC includes 3 components:
Comprehensibility: Ability to understand and predict one’s daily events
Manageability: Ability to meet the demands of one’s daily life tasks
Meaningfulness: Perceiving that one’s effort are worthwhile, justifying one’s investment
Results:
Movers had lower positive-mood and NKCA
Moving=>less positive-mood => less NKCA
SOC buffered effects of moving on NKCA: o High-SOC movers had higher NKCA than low-SOC movers
Thus, positive mood is a MEDIATOR and SOC is a MODERATOR of stress-NKCA
High SOC: protective against major stressor.
Example 4: Does concealment of an illness affect immunity?
73 HIV seropositive gay men were assessed for concealment of being gay, social support, depression and CD4-counts
CD4 is a major predictor of prognosis in HIV
Results:
23
Concealment predicted CD4 counts
It predicted only among socially-supported patients!
Higher CD4 when there is a lot of social support.
When you have few friends it doesn't matter a lot if you are still in the closet or out of it.
When you have a lot of friends this has a big influence. o They have a lot of friends and they are not telling them something very important.
When they are out of the closet, they benefit greatly from the social support.
Job strain and immunity
= Combination of having a lot of demands (long hours, loads of work, mental work or physical activity), little control over work (little freedom).
Relation between job strain and several immune factors.
116 Japanese men working at a nuclear electric plant were assessed for job-strain & for
T-cells, IgG, IgM, IgA, IgD, IgE & NK.
The effects of age and alcohol were controlled for
Results
1.
High job-strain was associated with LOWER T-cells and HIGHER IgG
2.
Job-strain was INVERSELY correlated with NK-cells
3.
Work-site social support was POSITIVELY correlated with CD8 cells
24
Does stress affect the ability to benefit from vaccines?
Caregivers of Alzheimer's disease (a model of chronic stress) were compared to matched controls in relation to: Antibody- and T-cell responses to the flu vaccine
Caregivers of Alzheimers pts: o Immune system is not very good, they are themselves unhealthy. They don't do well. o They have chronic stress, they care for hours and hours for people who don't respond anymore and aren't grateful. o Caregivers had lower antibody responses o Caregivers had lower IL-2 levels
Compared to people of the same age who don't do this, they saw that the caregivers had a lower antibody response and IL2 response. IL2 triggers the lymphocytes (Th1).
They had less of these: changed profile of T cells.
Does stress affect the ability to benefit from vaccines?
48 Medical students undergoing 3 blocks of 3 day exams were given Hep-B vaccinations and their immune response was tested
Social-support and distress was also tested
Results
Students who seroconverted (good antibody response) were LOWER on anxiety and stress than other students
Students with HIGHER social-support and LOWER distress had stronger antibody and
T-cell responses to Hep-B at the 3 rd exam
More social support and lower distress: stronger antibody and T cell response.
Optimism and immunity
Optimism is positively correlated with cellular immunity in controllable, brief and straightforward situations
Optimism is inversely correlated with cellular immunity in uncontrollable, chronic and complex situations
The latter may derive from optimists’ conscienciousness and over-engagement in tasks, even if complex
Optimists sometimes have better, sometimes badder cell immunity.
Positive correlation in situations in easy, controlable, solvable situations.
Negative correlation when this is not possible. The pessimists then give up, which then helps: positive cellular immunity.
25
!!!! Context
Psychological risk factors in CHD:
Factors, mechanisms & intervention
What is coronary heart disease?
• Coronary heart disease (CHD) is a disturbance in the functioning of the heart because of pathology in the coronary arteries
• Three types of CHD:
• Myocardial infarction (MI): Occlusion that leads to cell-death in the heart
• Unstable angina: chest pain with changing intensity, frequency or duration + at rest! May reflect sudden changes in plaque
• Stable angina: fixed CAD, with predictable angina episodes
• The basis of CHD is ischemia:
• Insufficient blood arriving to the heart.
• Causes of ischemia:
• An atherosclerotic process
• The heart requires too much oxygen
Psychological factors can cause stress on the heart and arteries because these are sympathetically innervated.
What is atherosclerosis?
Gradual narrowing of the inside of the coronary artery, due to:
• Injury of the arterial endothelium
• Dysfunction of the endothelium
• Penetration of LDL-cholesterol & SMC to the intima
• Migration of immune cells into the injured wall
• Chronic repair mechanisms
It is like in cancer, “a never healing wound”
Psychological CHD risk-factors: The rise & fall of the Type-A pattern
A lot of the patients had a similar personality
Very competitive
Impatient
Hostile
Time-urgency
Predicted double the risk of later CHD.
= type A type B who don't have this personality.
26
BUT…
1.
Too many people are “type-A” (up to 70%)
2.
Well-designed studies failed to show a relationship between Type-A & CHD
3.
Most of its components, accept hostility, are unrelated to CHD
False alarm: this personality is widely seen, but with low outcome. Not a real risk factor.
Only one thing was highly predictive: hostility.
Behave disagreeable
Cynically (how are you - why are you asking?!)
Feel a lot of anger
Can be measured in many ways.
Questionnaires: but people don't like to admit that they're angry and hostile.
Interview: you measure the bloodpressure and in the middle of the interview you start by not letting them finish their answers.
Projective test – Rozensweig aggression test
Future implicit tests? Emotional stroop, IAT
Each tool has advantages & disadvantages
Hostility predicts subclinical atherosclerosis
Method:
• 374 young people (age 18-30) were evaluated for hostility (Ho-scale).
• They were followed for 10 years.
• The outcome was calcification, a subclinical marker of atherosclerosis.
• Age, sex and race were controlled for.
Level of hostility at baseline vs level of calcification 10y later?
Results:
• People with a high initial Ho-score were 2.57 times at risk for any calcification than those with low Hoscores.
• People with a high initial Ho-score were 9.56 times at
20
18
16
14
12
10
8 risk for calcification of > 20 than those with low Hoscores.
Evidence for a statistically and clinically-significant riskfactor!
6
4
2
0
< 14 14-19 20-25 > 25
Hostility predicts CHD
• Method:
• 384 non-CHD participants were evaluated for Type-A and all its components, using the
SI.
• They were followed prospectively in relation to CHD-death and non-fatal MI.
• Hostility included:
• Style, content & intensity
DUS:
People are interviewed, focusing on hostility.
Calcification
27
Every question gets a score on: style (how do they react towards you?), content (what they answer) and intensity.
Has been replicated many times.
Results:
1). Only hostility predicted CHD (R.R=1.5).
2). No other Type-A component predicted CHD.
3). The best predictor of CHD was the hostile style, controlling for age, cholesterol, BP and smoking.
The best predictor of CHD = style.
Double correlation between hostility and CHD compared to cholesterol!! Really important risk factor.
Hostility interacts with biological risk-factors in relation to
CAD
73 Israeli patients with suspected CAD underwent angiography
They were assessed for hostility, daily hassles & hopelessness, and CHD risk factors
(e.g., family history, smoking, HT)
Effects of hostility & family-history on
4.5
CAD-severity (Gidron et al., 2002)
4.0
3.5
3.0
FAMILY HISTORY
2.5
2.0
LOW HIGH
ABSENT
PRESENT
HOSTILITY
When there is a family history of CAD, there is a more severe CAD than when there isn't a family history. Also, high hostility correlates with higher severity, but mostly has effect when there is a family history, when there isn't it has almost no effect.
Hostility & CHD
Meta-analysis= if you want to know whether a certain medicine works efficiëntly. You look for a meta-analysis: the entire literature was screened by someone and brought together. Also tells you in which subpopulation this is the most important.
In a meta-analysis of all studies, hostility was found to be a significant predictor of CHD, independent of typical risk-factors (e,g, smoking, BP, cholesterol)
Other Psychological predictors of CAD onset
• Depression has been shown to predict onset of CAD in healthy individuals
• Jobs high on demand and low on control (job strain) are “ coronary-prone ”
28
• Nurses
• Jobs with effort-reward imbalance are coronary-prone
• A lot work but little reward (eg if you get lag for every client you get, but you call 50 people before you get 1 client and everyone's pissed at you for calling them).
• Unfairness
• How fair is your boss? (work injustice) ==> dying faster from heart disease if high work injustice.
• Chronic job stress has an effect on the heart.
• Severe acute stress triggers MI
• Acute severe stress
During the first nights of the 1991 Gulf war, incidence of MI in Israel was significantly higher than 5 control periods
Despite continuing attacks, incidence of MI returned to “ normal ” after a few days!
The first nights included much uncertainty about the nature of the threat, its timing and intensity
More heart attacks during the first days of the Gulf war, because of the very high uncertainty and lack of control. Israël was being bombed and they didn't know if it was with chemical weapons or not, they could'nt react, ...
Which psychological factors predict prognosis in CHD?
Psychological predictors of CHD prognosis – appraisal of damage
Draw the heart before and after the heart attack. o All drew a scar after the attack. o They compared how much you drew the scar (size) and the concentration of troponine ( how higher, how more muscle starvation, used to measure the extension of the heart attack).
Was correlated positively with the troponine levels. How higher these were, the bigger the scar was drawn.
When they look at how fast the recovery went, it wasn't correlated with the troponine levels, but with how big the scar was ==> dependent of their appraisal.
Perceived-cardiac damage correlated with:
29
Peak Troponin-T levels (r = 0.41, p< .001).
Days to return to work at 3 mo (r=.37, p< .05)
Psychological predictors of CHD prognosis – Type-D personality
Type D personality
• Type-D personality refers to increased neuroticism and social inhibition
• Type-D was repeatedly shown to predict prognosis in CHD, independent of prognostic factors
• This takes into account a more stable psychological factor, while depression may result from or change as a function of CHD!
• Patients who went on to die later from disease were characterised with a similar personality.
• They were very closed, very anxious but don't say anything.
• They die much faster.
• Type D is an independent prognostic factor in heart disease.
Psychological predictors of CHD prognosis – Social support
Need of more tangible support at home predicted death in post-MI patients, independent of initial health and age
People who need more support and have little social support have a badder prognosis. Having more friends and support protects you against the effects of the disease and benefits the survival.
Psychological predictors of CHD prognosis – Hostility
A recent study found that hostility significantly predicted recurrent CHD events, in post-MI patients o But only in men!!
These effects were independent of various biomedical factors (e.g., age, BP, diabetes) and depression!
Model of stress:
JDC: job demand control
30
The model of stress, appraisal, coping, resources & outcome applied to CHD
A PNI model of the acute coronary syndrome
The field of psychoneuroimmunology (PNI) tries to understand the biological mechanisms linking psychological factors with disease
This is scientifically AND clinically important
? Why do arteries respond to anger?
Psychoneuroimmunology:
Acute coronary syndrome ACS
ACS include unstable-angina + MI.
The etiology of ACS includes 3 stages:
• 1. Instability of the coronary plaque
• 2. Rupture (breaking) of the plaque
• 3. Thrombosis at the broken area => Severe occlusion => ACS
People suddenly have a heart attack: cardiologists concluded that if people came several times to the hospital, they found that the patients had come a few weeks or months before and didn't
31
have 80% occlusion, but only a little plaque. What had happened so that the plaque got so big so fast?
The small plaques had ruptured. It was an unstable plaque. Trombosis occurs to heal it.
Acute Coronary Syndrome ACS:
CD40-40L & MIF increase adhesion molecules (VCAM, ICAM) on endothelium o These recruit monocytes to the plaque which further increase MIF (positive feedback) o Macrophages in the plaque then secrete MMPs that disintegrate the plaque!
The process happens happens so fast because of metallomatrixproteases (MMPs) o Destabilizes the plaques by recruiting monocytes. o They are related to psychological factors.
We can see that people with depression have higher ICAM( glueing molecules for the monocytes).
Another test looked at blood measurements at uptake in the hospital. o The day after, they were questioned about hostility,.... o The monocytes mirrored the mental life from the patients the best : more hostility=more monocytes, more social support= less monocytes,... (zie verder)
Instability of the coronary plaque o Stress, depression & hostility are correlated with recruitment of leukocytes
(M Ø ) o M Ø => release MMPs o MMPs disintegrate coronary plaque matrix
coronary plaque instability
Factors leading to plaque rupture o Elevated BP o Vasoconstriction o Shear stress o Intra-plaque hemorrhage from microvessles that developed in the plaque o Active platelets o Pro-inflammatory cytokines increase BP
Coronary plaque rupture o Hostility/anger are strongly correlated with vasoconstriction (r = .82) o Hostility may contribute to high-BP o Vasoconstriction & BP can break a plaque
Coronary plaque rupture
What causes the plaque to break? o The plaque breaks because inside there is an accumulation of MMPs and monocytes. On the exterior: high blood pressure, vasoconstriction and stress factors. o r=.82, strong correlation between vasoconstriction when retelling their story of
ACS and the anger and hostility while doing so.
After the rupture: trombosis= aggregation of platelets.
People with high depression or anger have too much platelet aggregation
Leads to trombosis and ACS!
Factors leading tot trombosis o M Ø & SMC => secrete TF o Fibrinogen => Fibrin
32
o active platelets => von Willebrand factor => 3 dimensional platelet-fibrin network
Thrombus!
Thrombosis o -Hostility, anger-out & depression are positively correlate with platelet aggregation o Platelet aggregation => Thrombosis => Severe coronary occlusion => THE
ACUTE CORONARY SYNDROME!
PNI mechanisms play a role in:
– Plaque instability (M Ø recruitment)
– Plaque rupture (BP, spasms)
– Thrombosis (platelet aggregation)
severe coronary occlusion => ACS
Psychological predictors of cancer prognosis
A brief introduction to cancer pathophysiology
• Tumors begin with mutations that accumulate over time in several genes (multi-hit multi-step theory)
• Some mutations are in tumor-suppressor genes (P53)
• Pro-oncogenic changes can occur without constant alterations to genes - by methylation (temporary silencing of tumor suppressor genes)
• Inflammatory signals (e,g., TNF) in the microenvironment of such mutations promote their growth and proliferation
• If you knock out TNF, mutations don't evolve to cancer.
Tumors of most kind have 6 characteristics:
1.
Self-sufficient in growth signals
2.
Insensitive to anti-growth signals
3.
Escape from cell-death (apoptosis)
4.
Unlimitted replication potential
5.
Continuous angiogenesis
6.
Invasion & metastasis
90% of death from cancer occurs in stage 6 (metastasis).
We should prevent metastasis to lower deaths.
Linking psychological factors with basic tumor biology
• Stress can cause DNA-damage
• Especially in women, mostly from work-stress.
33
• There can even be conditioning (Pavlov) in which DNA damage occurs in a conditioned situation.
• Stress is associated with elevated pro-inflammatory cytokines that promote early tumorigenesis (e.g., TNF)
• Stress is manifested by increased stress hormones (cortisol, NE) which promote tumor metastasis by receptors on cells
!! Little evidence that psychological factors predict the beginning of cancer. No evidence that psychological factors can cause the cancer. A lot of evidence that they do predict the
prognosis!!
Psychological factors and cancer-onset
• Psychological factors were found to correlate with and cause DNA-damage
• I hypothesize:
psychological factor x DNA-damage => cancer
This needs to be tested
Reviewing 70 prospective studies, looking at:
Hopelessness,
Depression,
Denial,
Fighting spirit,
Stoic acceptance,
Social support,
Life-events,
Negative emotional states
Active coping,
Personality,
Locus of control;
Only hopelessness, repression and little denial seemed to consistently predict poor prognosis!
Little denying: worst prognosis!
A recent meta-analysis of 120 studies found: Several psychological factors including
Stressful events
Little social support
Depression
Significantly predicted prognosis, independent of known prognostic factors
Experiment 1:Do psychological factors predict prognosis in breast cancer?
Method
578 women with early-stage breast cancer
Were followed for 5 years
Measures:
Fighting spirit,
34
Stoic acceptance,
Hopelessness,
Denial,
Anxiety,
Depression
Emotional control
Biomedical prognostic factors were considered
Results
Hoplessness predicted survival, but
not after controlling for tumor stage
People with high fighting spirit: being realistic, fighting spirit <=> stoic acceptance: also fighting, but unrealistic (I survived an earthquake, I'll do this).
Best: fighting spirit.
Worst: hopelessness.
Chance of surviving: higher survival with low hopelessness. Significant predictor of prognosis.
You can induce faster dying of a tumor by inducing helplessness.
Experiment 2: HH & prognosis in women with cancer: New data from UK
In over 60,000 British women,
Over 8000 who had cancer, we examined The effects of HH on prognosis
Higher hopelessness: lower survival.
The women who are young and hopeless without family support: strongest effect.
35
Experiment 3: Example of a implicit optimisim word search test
R G H Q W D T A Y P O N T
T R G U H O P E B D Z G Z Y
R Z A Q G S A D T Y L M B H
E Z S O P T I M I S T Z S R V G
T G B P E S S I M I S T V R N R
T H E R T C V Z S A X S T P K B
Implicit op score = No. Op words – No. Pes words
Late diagnosis because the symptoms get confused with something else.
Eg lung cancer often found by mistake, people think they just think they have a cough.
Ovarian cancer: mistaken for menstrual symptoms.
The patients with lung cancer got questionnaires (positive).
Also word search test to measure optimism. o 5 words that were optimistic and 5 pessimistic, hidden. o There is a list with all the words and you get 1 min to find them. o How many optimistic words minus pessimistic words were found? o What was the correlation with survival?
The more positive words, the better the survival was.
The relationship between implicit optimism & survival in lung cancer
Experiment 4: Significant independent psychological predictors of death in melanoma patients
Melanoma:
Patients who perceived or reported:
• that the aim of their treatment was curative
• who minimized their illness
• reported more anger about their illness
• that their illness was easy to cope with
• were married
• Reported better QOL
Survived longer!
reflected hope.
36
Relation between perceived aim of treatment and survival in melanoma patients
Patients who were optimistic about their treatment (it will CURE them) and who were angry enough to motivate them to perhaps do something about the cancer, but also put it all in perspective (minimization) and continued their other life domains, lived longer!
Experiment 5:Psychological factors & lung cancer
Method
103 lung cancer patients, stages 3-4 were followed for 10 years
Measures
Depressive coping: Self-pitty, taking it out on others, distancing oneself from others
Active coping: seeking information, planning, problem-solving, intending to live intensively
Age, sex, stage, histology, performance and treatment were considered
Results
Pts who are depressive copers die faster!
Tell a patient with cancer that they have to have a positive attitude towards the treatment to cure them and advise them on how to live their normal lifes without stopping it because of having cancer, so a good QOL is maintained.
We can't tell them they'll die, that they'll die faster if they are hopeless.
If your patient is a depressive coper, you can't tell them they'll die faster, but also on the positive side we can't tell them they'd live longer if they would be optimistic. o This because we can't guarantee this and also, scientifically the studies were observational, NOT experimental studies, which are the only one's that can show causal relations!!
We can suggest to change the lifestyle because it predicts longer survival, but note that it cannot be guaranteed.
37
Social support – the concept
Quantity – network size
Function:
- Emotional – receive empathy, love, etc.
- Instrumental – movement, etc.
- Informational – about illness, coping, etc.
So what do we know ?
• Hopelessness seems to be important
• Minimizing seems to be important
• Problem-solving/active coping is importat
• Self-awareness of body is important
So what do we not know?
• Do psychological factors predict prognosis in pediatric cancer (child, parent factors)
• What about interactions with biomedical factors -> locate highest risk group
• Do implicit measures, unaffected by presentation biases, predict prognosis (IAT, AMT, word-search; emotional stroop)
• There is nearly NO evidence for causal relations between psychological factors and prognosis in humans!
• Many intervention trials have negative findings!
• No study has shown that REDUCING HH improves survival yet! Thus, we CANNOT tell people to be hopefull so they will live longer!!!
Experiment 6: Does intra-marital communication predict levels of CA125 in women with ovarian cancer?
Background
Ovarian cancer is among the most fatal femal cancers, also as it is often discovered late
It has a biomarker – CA-125, of high prognostic value
It would help to identify modifiable predictors of the prognostic marker CA-125
Optimism, the tendency to expect positive future events, was an independent predictor of declines in CA-125 in a follow-up of 15 weeks
Unknown issues
- Ovarian cancer can affect couples’ intimacy & relationship
- Marital discommunication can negatively affect women’s mental well-being
Can marital communication affect prognosis?
Purpose
To investigate whether marital communication predicts CA-125 levels, independent of known prognostic factors?
Hypothesis
Level of marital communication will be inversely related to CA-125 levels at follow-up
38
Method
N = 72 British women with ovarian cancer
Assessment:
General marital communication
Illness-related marital communication
Confounders: Baseline CA-125, age, stage, time from diagnosis/treatment, recurrence, treatments, group (exp/cont.)
Measuring of overall and illness-related communication.
Conclusions
1.
Illness-related marital communication predicted declines in CA-125, independent of confounders
2.
Men’s perceptions of illness-related communication was a better predictor of women’s
CA-125 than women’s perceptions!
The more they communicated about the illness, the lower the CA125 levels.
The more the husband stated to have communicated, the lower the levels were in the wife.
Experiment 7: From behaviour to cells: IL-1 as a possible mediator between hopelessness & cancer-progression
Identify a marker to show the relation between hopelessness and helplessness (HH) and prognosis of cancer.
HH includes = pessimism + helplessness:
1.
Perceived lack of control (helplessness)
AND
2.
Anticipating a negative future (pessimism)
This is among the common reactions to cancer (20%), which affects also psychological outcomes.
HH and its cognitive aspects are precursors of depression.
Meta-analysis: HH had “ promising ” evidence for a prognostic role!
39
ES: escapable shock
IS: inescapable shock
PS: did not get a shock, but were forced to see how others were shocked. Had the biggest tumors.
Clear cause of relation between helplessness and dying of cancer in mice.
Mice al got the same carcinogen.
Mice who were given an escapable shock vs mice who couldn't escape it. o Both groups got the same frequency, duration,...of shocks.
One week later, the tumors were significantly greater in the group with inescapable shocks.
Effects of uncontrollable stress on lymphoma in animals
The purpose of our model
• To identify a mediator at all relevant levels:
Brain, systemic, tissue
• To show that is it POSSIBLE to link HH to cancer-progression
• NOT to claim for THE model, but A model!
Hypothesis
IL-1 may mediate the epidemiological relationship between HH and cancer progression
link between the psychological factors and the biological effects.
40
IL1: lymphocyte proliferation, participates in many 'good' processes.
If IL1 is blocked in the brain, mice do not develop helplessness!
If put in a new situation with controllable stress: o The mice who could escape the shock will learn the fastest o The one's with learned helplessness just sit at the side.
They don't try to stop it, they believe they can't.
When they are given a IL1 blocker, they started to behave as if they came from the IS group could be entirely reversed!
What does brain IL-1 do to cancer?
Animals were injected with a peripheral tumour:
Half were given IL-1 in the brain, half placebo
Brain-IL-1 led to more metastases in the lungs than placebo.
DUS: more IL1: more metastasis, aside from more HH!
This was blocked by a beta-blocker, Nadolol
Is helplessness associated with peripheral IL-1?
A few studies showed that uncontrollable stress caused elevated levels of peripheral IL-1.
More than other cytokines, IL-1 responds to this type of stress!
If it causes more metastasis, it could be an important factor!!
Is IL-1 associated with cancer-promoting events?
Angiogenesis
IL-1 plays a role in increasing IL-8 and VEGF
Helplessness was positively correlated with VEGF in ovarian-cancer patients
IL-8 & VEGF are central to angiogenesis
Metastasis
In a study on IL-1 and melanoma cells:
IL-1 increased VLA-4 on melanoma cells
IL-1 increased VCAM-1 in lungs
IL-1Ra REDUCED metastasis in liver
IL-1 plays a causal role in metastasis
IL1 puts glueing molecules(VLA, ICAM,..) on the tumor AND on the site where the metastasis will come.
41
Limitations of our model:
1). It is based on corroborative evidence
=> Test directly HH-IL-1-Cancer progression
2). What about other mediators
=> IL-6, TNF-alpha, Oxytocin
3). What about other psychosocial factors such as social-isolation, hostility, etc.
Neuro-immuno-modulation of cancer:
Does the vagus nerve have a role in tumor-modulation?
Three major triggers of cancer onset and prognosis
Oxidative-stress & DNA damage : molecules loose electrons and seek to refill the empty orbits. o More oxygenation, more oxidative stress ==> more
DNA damage and less survival.
Eg. Hepatocellular carincoma HCC: less survival if more oxidative stress. (Figuur)
Inflammatory signals : An excessive recruitment of leukocytes to an injury to “stressed” tissue – lacking oxygen, evolving tumor, etc Tumours express cytokines
(e.g., IL-1, IL-6, IL-8) o Tumour-associated cytokines (TAC) promote
Escape from apoptosis
Angiogenesis
42
Metastasis
Thus, TAC promote cancer progression
Tumor-associated cytokines TAC promote the tumor characteristics. o Study where they genetically blocked the IL1 receptors: did not develop metastasis!
Inflammation clearly plays a role in tumors.
Exessive sympathetic nervous system (SNS) activity
Study showed that if you take tumor tissue and put norepinephrine next to it: the tumor metastasizes towards the NE.
Most cardiologists and immunologists have no clue about this, very sad!
Women with breast cancer who took beta blockers by chance lived longer then the one's who didn't.
The vagus & visceral information
The vagus receives afferent information from multiple visceral regions including the colon, lungs, esophagus, pancreas, etc.
Sites of common cancers.
Does the vagus modulate patho-physiological processes leading to cancer?
Three major triggers of cancer onset and prognosis:
Oxidative stress and DNA damage
Inflammatory signals
Excessive sympathetic nervous system SNS signaling.
How can we stop these processes?
Activating the vagus nerven blocks all these three.
Nervus vagus
How may the vagus modulate inflammation?
43
Receives information from multiple regions. o 80% go to the brain, o 20% is efferent.
Infrastructure is there for communication between tumor and the brain
Indeed, vagal activity is inversely related to oxidative stress.
It also informes the brain about inflammation and then reduces it by releasing Ach, for which the monocytes and macrophages have receptors. Because of this, a reduction in inflammation occurs.
Heart Rate Variability HRV
HRV: heart rate variability, this is a vagal index.
More vagal activation = less inflammation
Rechterfig: HRV and inflammation in CDH
HRV & sympathetic hormones
Vagal activity and SNS activity
HRV correlates inversely with epinephrine
Cancer patients experience uncertainty & threat SNS
Beta blockers reduce metastasis
Hypothesis:
1. The vagus may “teach” the brain about visceral tumours because it transmits information about tumor-associated cytokines
2. The vagus may modulate tumours by inhibiting:
- Oxidative stress
- Inflammation
- Exessive SNS activity
Vagal activity can inform the brain about an ongoing tumor.
The brain doesn't know it has cancer,....but knows there is inflammation.
Low vagal activity in chronic diseases.
Better prognosis if these mechanisms are blocked by vagal activity.
Experimental evidence
Cancerpatients can be recognized by cachexia and pain.
The vagus nerve is also controlling this!
44
Effects of chemical vagotomy on food-intake in animals with/without tumours
25
20
15
10
Control
Capsaicin
5
0
No Tumour Tumour
Animals: how much they eat with or without a tumor.
They eat less if they have a tumour.
If the vagal nerve is inhibited, their eating habits heighten again.
The nervus vagus produces the cachexia because of the tumour activating it. If it is inhibited, cachexia disappears.
Capsaicin in hot peppers: how higher capsaicin, how more blocking of the vagus, it vagotomizes the animal periodically.
Intact vagus, less metastasis. o The more denervated, the more tumour growth. o More metastasis if the vagus is cut.
A vagal-dependent anti-inflammatory drug reduces tumor volume
Drug doesn't work if there's a vagotomy
Human evidence:
What happened to vagotomized patients?
Three prospective studies found that vagotomized ulcer patients died more in general, & specifically from cancer, than non-vagotomized controls (but not all studies show this!)
Our VUB evidence: HRV & prognosis
A historical prospective design
Exclusion of no ECG, no tumor marker, cardiac diseases, cardiac medication, thyroid disease, inflammatory disease
Cancer
Colon (N=72)
Outcome
CEA, survival
45
Prostate (N=113)
Pancreas (N=348)
PSA
Survival
Lung (N=120) Survival
Confounders: Age, stage, gender and treatments (specific per cancer)
ECG was taken…
from patients before operations.
on alive patients: historical perspective.
Taken at time 1, outcome measured at time 2.
Negative correlation between vagal activity and tumor marker later, independent of stage and treatment.
More vagal activity = less tumour marker.
If you look at vagal activity at baseline and you split in a group with high and one wih low vagal activity
low vagal activity: tumour markers grow.
the one's with high vagal activity: didn't change
Especially in the worst stages: high vagal activity, less progression of the tumour.
More vagal activity=longer survival.
Pancreatic cancer: Relation between HRV & survival in pancreatic cancer patients
Looking back at former EKG of stage 4 patients, the HRV was measured.
Then we looked at survival.
Low vagal activity: survived 60 days
High vagal activity: survived more than double this time! Smaller risk of dying.
Does the vagus moderate effects of tumor stage on cancer evolution?
We re-examined our data:
We split them into high (HRV >20ms) & low (HRV < 20ms) vagal activity
We examined the relation between initial tumor stage and tumor markers later, in patients with low and high vagal activity
46
Conclusions:
The worst tumor markers were found in stage 4 ( 2).
Much higher markers one year later, ONLY when low vagal activity.
The higher the stage, the higher the tumor markers one hear later, but only with low vagal activity!
• Vagal activity cancels the activity and effects of the stage.
Thus far…
Vagal activity predicts cancer prognosis
Vagal activity protects (moderates) the negative effects of severe initial tumor stage on long-term tumor burden
In animals, vagotomy accelerates tumorigenesis
In animals, vagal activation reduces tumors
These results are in line with a vagal neuro-immuno-modulation of cancer
Limitations of our model :
47
We did not test mechanisms (inflammation, oxidative stress, SNS)
We have not tested experimentally, whether activating the vagus slows down tumors, in humans!
Effects of HRV-Biofeedback on HRV
More CRP: less survival
SDNN: vagal activity
In long survivors: low correlation between high CRP and low vagal activity (????????Niet zeker van in de les!)
How to activate the vagus?
Breathing techniques
Medication that reduces inflammation via activating vagus : not yet available
Device that stimulates the vagus, used in epilepsy.
Psychosocial predictors of infertility and its mechanisms
How to investigate this topic?
• Psychosocial factors may predict infertility
• Infertility affects psychosocial factors (e.g., depression, anxiety, anger)
• Reciprocal relationship between psychosocial factors and infertility
=> longitudinal studies are needed
48
If you have a pool of people, some of them have a personality "X"--> do they have a lower chance of becoming pregnant with IVF than those with another profile? Or is this personality profile a risk factor for becoming infertile?
Event: infertility
What types of psychosocial factors?
• Prior life events
• Psychological reactions
– Anger, depression, anxiety, helplessness
• Coping: EFC (denial), PFC (planning)
• Social support
• Beliefs & attitudes about pregnancy
• Psychophysiological responses to stress
– HRV, IL-6, TNF, Oxitocin, Cortisol, EPI, etc.
– maybe stronger respons -> less chance of successful fertilisation.
Attitudes towards parenthood and your partner and infertility
In a prospective study, couples had higher chances of pregnancy if:
Before starting treatment: how much do you want to have a child?
– Women had higher positive motherhood expectations
– Men whose wish for a child was integrated with their sexual relation
Life events, lifestyle and infertility
People who had more fobia had interestingly higher chances!
49
Very religious: more chance
Job stress and infertility
Tested the effects of women’s job-strain on fertility (Job strain: High job demand & low control)
Job strain predicts lower fertility (only in idiopathic infertility).
So this is only a risk factor in a subgroup!
Coping and IVF outcome
N = 88 Israeli women took part.
23.9% became pregnant
Measured coping: Compared “letting go” and “problem-focused
Coping as predictors of IVF-outcome
Statistically controlled for: Age, infertility cause, number of cycles
Results:
Letting go (stop trying after trying a lot) and problem focused coping.
People who are low on letting go : teach them to do this
Cardiovascular reactivity to stress and infertility
Stroop test: saying only the name of the colour in which the words are written down.
Participants underwent the stroop test, and their HR & BP responses were measured
Conflict --> BP
Participants with higher cardiovascular reactivity to the stroop stressor had lower chances to be pregnant later!
Heart-rate variability & adverse pregnancy outcomes
Measured autonomic balance in the 1st trimester, in women.
Women who had complications at labour (who were at risk or in IVF) were compared to women with normal pregnancies without complications
The higher HRV, the better: adaptibility
50
Figure: left normal pregnancies, right risk and IVF with adverse outcome.
In the risk group the sympathetic was higher, HF was lower : insufficient vagal and oversufficient sympathetic.
Inflammation, NK cells & IVF outcomes
• Pro-inflammatory cytokines are positively correlated with activated
NK-cells in women undergoing IVF
• NK-cells may have detrimental effects on reproduction
• NK cells attack viruses. NK cells lower during pregnancy so they wouldn't attack the baby.
Pro-inflammatory cytokines in MD-students as a function of academic-stress period
Stress = more inflammation, anti inflammatory response is too small. Vagus supresses this via communication with the brain.
120
100
80
60
40
20
0 mid-term exam vacation
Low anxiety
Hi anxiety
9
8
7
6
5
4
3
2
1
0 mid-term exam vacation
Low anxiety
Hi anxiety
51
A proposed psychoneuroimmunological model of infertility
Pregnancy-specific stress
• Pregnancy-specific stress may be a more powerful contributor to birth outcomes than general stress
• Pregnancy-specific stress = > Gestational age
• Pregnancy-specific stress Smoking Low birth weight
Important! Low infant birth weight is predictive of:
• Poorer cognitive development
• Attention problems
• Risk of adult coronary heart disease (CHD)
• Risk of adult diabetes
Stress is related to lower birth weight, specifically for stress about the pregnancy.
Cortisol, a stress hormone, activates glucocorticoid receptors (GR)
• Changes in the epigenetic regulation of the fetal GR promoter associated with
exposure to prenatal maternal stress
• May be a mechanism by which maternal stress influences fetus development!
52
• Bcl I GR polymorphism is associated with increased glucocorticoid sensitivity, & was
overrepresented in pregnant women with hemolysis, elevated liver enzymes & low platelets (HELLP), a pathological maternal-fetal immune adaptation syndrome (
• Thus, this polymorphism is a vulnerability factor in the context of pregnancy
• HELLP: increased glucocorticoid sensitivity
Prenatal maternal stress x GR polymorphism Infant development
Is there a nature x nurture interaction?
Purpose of the study
• To test whether prenatal maternal stress and maternal attitudes towards pregnancy predict infant birth weight
• To test whether maternal and infant GR polymorphisms predict infant birth weight
• To test whether:
Maternal stress x GR polymorphism => Infant birth weight?
Stress and attitudes:
1.
How stressed were you during the pregnancy?
(1= Low, 2=Medium, 3=High, 4=Very High)
2.
Select a word best describing your attitude towards the pregnancy from the words:
Happy, Satisfied, OK, Tired, Sad, Stressed, Angry, Other
Glucocorticoid receptor polymorphysm
From matched samples of maternal blood and placenta
The primers used included the Bcl I RFLP C to G mutation, 646 bp downstream of exon
2
Three genotypes were present – CC, GC, GG
Results:
53
Levels of stress as a function of attitude towards pregnancy
Attitudes during pregnancy --> levels of stress higher in negative groups.
Did maternal stress predict infant weight?
No correlation between mother's stress level and birth weight.
Did maternal attitudes towards pregnancy predict infant weight?
Attitude had a correlation! Negative attitude towards pregnancy had significantly smaller babies.
Distribution of maternal GR polymorphism
Fetal distribution of GR polymorphism
54
Fetal and maternal Bcl I polymorphisms were significantly correlated.
Did GR polymorphism predict infant weight?
• Maternal Bcl I polymorphism was unrelated to infant birth weight (F(2,60) = 0.05, NS).
• Fetal Bcl I polymorphism was unrelated to infant birth weight (F(2,60) = 1.37, p > 0.05).
GR polymorphism did not predict the birth weight.
Is there a nature-nurture relation?
a relation to the genes?
3.5
Neu_Pos
Negative
3
2.5
2
1.5
1
0.5
0
GG GC
Only in the GG group, did maternal attitudes predict infant birth weight
Conclusions
• Prenatal maternal stress did not predict infant weight
• However, negative prenatal maternal attitudes towards the pregnancy predicted lower infant weight, especially in mothers (and infants) with a GG GR polymorphism
• This suggests a nature x nurture interaction and that both factors need to be considered!
• Given the long-term effects of low birth weight (cognitive development, CHD)
55
• And given that both maternal attitudes and GR polymorphism can be easily assessed early in pregnancy
These findings may have preventative value for public health
Maternal stress, pregnancy planning & infant birth weight
• In planned pregnancies:
– Stress predicted infant weight, independent of age & BMI
• In unplanned pregnancies:
– Stress did not predict infant weight, independent of age &
BMI
The inverse stress-weight relation in planned pregnancies only suggests that in unplanned ones, there is no mother-fetal coherence!
Unplanned pregnancies: chaotic, not much room for meaning
PNI of flu and colds
Pathophysiology of URTI
• URTI is caused by a virus in the nose
• > 50% are caused by Rhinoviruses
• More than 100 types exist, and the specific cause depends on the season
• Late fall & winter: influenza, para-influenza, and respiratory syncytial viruses
• All other seasons: Rhinovirus, echosackie virus, and coxsackie viruses
56
What are URI symptoms?
Upper respiratory infections (URI) include:
- Fever
- Cough
- Mucus production
- Swollen tonsils
- Runny nose
- Soar throat
- Stomach pains
- Urinary infections
The flu is similar, but focuses on:
Fever, soar-throat, headaches, muscle-pain & coughing
Symptom peak: 36-72 hours post virus invasion
Prevalence
20% of adults get the flu each year
Most people don't get the flu, but just a cold.
Stress & flu/cold
Nearly 400 healthy volunteers were quarantined and received 1 of 5 viruses
They were assessed for a stress-index (NA, perceived-stress, life-events)
The study considered 18 confouders!
Nearly perfect correlation was found between stress and objective development of the cold,
This remained intact AFTER controlling for all confounding variables (e.g., age, sex, season, initial immunity, personality).
What is it: Chronic or acute stress?
In a following study, they assessed people for acute stressors (< 30 days) versus chronic stressors (> 30 days)
Subjects with chronic stress were at increased risk of the cold:
Especially job- & interpersonal stress lasting 3-6 months
Chronic stress: supresses immunity (<=> acute stress enhances NK cells)
Social support & flu/cold
Social-isolation & the cold:
Volunteers reported the number of social ties they have, before given a virus
Those with 1-3 ties were 4.2 times at risk of developing a cold compared to those with > 6 ties, independent of many confounders.
How many friends do you have? More friends: less risk to get a cold than those with less friends.
They are exposed to more things and get immune, also personal relations form a buffer to stressors.
57
Affectivity and flu/cold
Is it positive or negative emotions?
Testing the predictive validity of positive vs. negative emotional style in relation to the common cold.
Psychological predictors of flu/cold
While positive emotional style predicted objectively verified colds, NES did NOT!
NES was positively correlated and PES was inversely correlated with self-reported colds
High negative (complaining attitude) low positive (low energy attitude)
Positive affectivity gets less colds than those with negative affect.
Negative affect will come a lot to doctors, because they complain.
Only the low positive affectivity get colds, the high negative affectivity don't get colds, they just think they do. They come to the doctor's more often than low positive affect.
Hemispheric lateralization (HL) & immunity
In the recent 2 decades, accumulating evidence showed that:
• The left hemisphere is immune enhancing
• The right hemisphere is immune suppressant
Animal studies show these to be cause and effect.
The sympathetic response may underlie it!
High right hempishere or high left hemisphere ==> who will get a cold?
High right get more colds!
Purpose & hypothesis of this study
Purpose
• To examine whether a neuropsychological index of HL predicts URTI symptoms
Hypothesis
• Greater right-HL, representing immune-suppression, will predict a higher risk of URTI symptoms, independent of confounders
58
Does HL predict the common cold?
80, cold-free participants underwent neuropsychological tests at baseline.
They were followed for up to 10 weeks.
Measuring lateralization by showing pictures, after showing other pictures. Which ones did you see before? --> bepalen lateralisatie
The right hemispheric lateralisation index =
100 x (picture recog. - word recog.)/(picture recog. + word recog.)
Additional confounders
1.
Health behavior using a single-score 13-item scale (diet, activity, leisure, etc.)
2.
Neuroticism using a 2-item scale (Statistical control)
Participants with upper resp infection had higher right lateralization.
Results
Predictors of URTI
• Poor initial Health Behavior
• Right > Left Hemispheric Lateralization
• Neuroticism did not predict URTI
Can we train people to train the other hempishere and so lessen colds? --> no idea yet!
Stress management at work
What are the daily stressor that you face?
All the studying I still have to do but don't have the time for
All the tasks I have to get done on time
How stressful is each?
9.5
7
How uncontrollable is each?
6
4
Stressfulness x uncontrollability
9.5 x 7= 66,5
7 x 4 = 28
Total: 94,5
Problem focused inventions at work
Aims
1.
To identify problems at work
2.
To solve them constructively
3.
To reduce their negative effects
59
Effects of a consultation process interventions in nurses
Method
Head nurses from 13 hospital units were randomly assigned to receive consultations or to serve as controls
Outcomes: Attitude to work, social alienation, job satisfaction and absenteeism
Consultation Intervention
manager-consultant problem-solving meetings for leadership development to improve their staff’s morale, health-care and reduce absenteeism
They were re-trained in problem solving by a process consultation method
Results
Nurses whose chiefs were retrained reported improved work-characteristics and relationship with colleauges
Their bosses were less centralizing power and had more clear expectations!
There was reduced job-alienation
But no effects were seen in absenteeism!
Can a stress management intervention improve health at work?
Method
58 workers in a highly-stressful job in Japan were randomized to stress management
(SM) or control
They were assessed for depression, ERI and job stress
Intervention
Perception of stress
Steps to manage stress
Stress diary
E-mail counselling
Results
The SM significantly reduced depression
The effects were independent of relevant confounding variables
But limited effects were seen for job-stress
Emotion Focused Coping interventions
Aims of EFC interventions
1.
To reduce the stress response
2.
To prevent unhealthy outcomes
3.
To enable better problem-solving
4.
To enable better job-performance
Types of EFC interventions
• Relaxation – PMR, deep breathing
60
• Meditation
• Hypnosis
• Writing
• Social support
How to do progressive muscular relaxation?
• Contract feet towards yourself
• Close legs close strongly (Dutch contraceptive)
• Contract stomach muscles inside
• Contract hands towards yourself
• Bring arms close to chest
• Raise shoulders high up like a Marionette
• Push neck back, with resistance
• Make a forced (American) smile..
• Close eyes strongly
• Raise forehead up!
* Breath normally from your nose, between sets
How to do deep breathing
Meditation
1.
Meditative breathing – put your hand on your stomach, focus on air in/out
2.
4-steps for handling psychological experiences (thoughts, feelings, sensations): a.
Noticing b.
Putting no energy c.
Observing flow d.
Returning to your breathing
* Use metaphors – boats passing in a river..
Mindful attitude:
• Be here now
• Accept things
• Don’t be judgemental!
Problem focused coping
How do we determine to use emotion or problem focused coping? Can I do something about it or not?
During stress we don't see all the alternatives. suggest several solutions and choose the best one, then implement it.
61
Effects of relaxation in the workplace
Purpose
Tested the effects of a brief 3-session relaxation intervention on stress and health-complaints in nurses in Taiwan
N=23 were in the relaxation group
N=23 were in an attention-control group
Results
1.
The relaxation group reported significantly lower nurse stress at 5 weeks
2.
The relaxation group reported significantly lower distress & health complaints at week
2 & 5.
3.
Duration of practice correlated with stress reduction: Dose-response!
A meta analysis of 36 studies on stress management at work
Method
36 RCTs were found (RCT: randomised control trial)
The total sample N = 2847 workers
Mean age = 35.4 years
Mean intervention duration = 7.4 weeks
59% women
Interventions: CBT, relaxation, organisational, multimodal, alternative
Results
1.
A statistically significant medium to large effect was found (d’ = 0.526).
2.
CBT produced the largest effects!
3.
If other components were added, the effects of CBT were reduced!
EXAMEN:
No facts to learn
Knowing the principles and general things.
Knowing what the purpose was in a described study ( not knowing the name of the author, multiple choice ).
62