Force-Plate MSD Meeting September 28, 2005
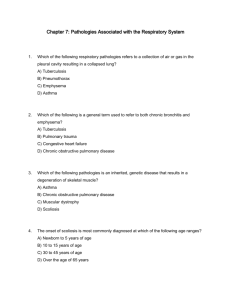
advertisement
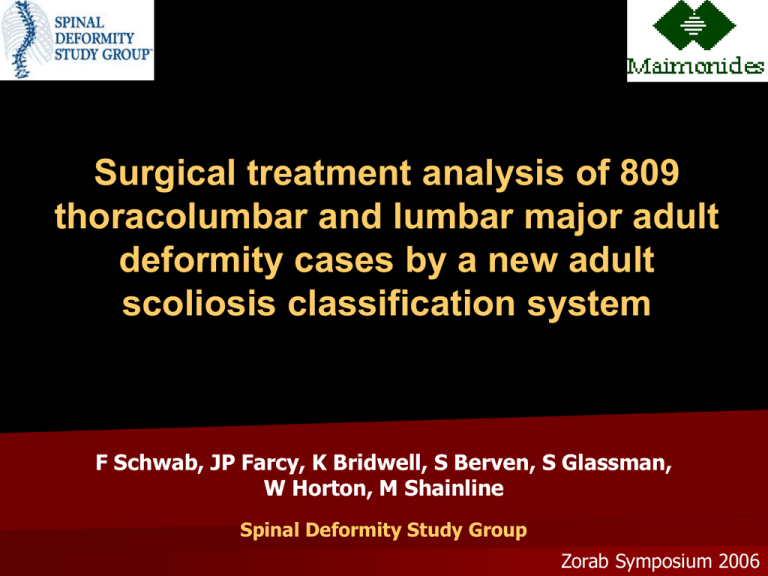
Surgical treatment analysis of 809 thoracolumbar and lumbar major adult deformity cases by a new adult scoliosis classification system F Schwab, JP Farcy, K Bridwell, S Berven, S Glassman, W Horton, M Shainline Spinal Deformity Study Group Zorab Symposium 2006 Background Unlike pediatric and adolescent scoliosis, no accepted classification system exists for adult scoliosis Scoliosis in the adult population – prevalence as high as 60% – significant pain and disability – Quality of life issues Classification systems provide – Common language for communication – Correlation with clinical impact treatment algorithms surgical guidelines Background Adult deformity: Treatment approach Curve severity • Cobb angle • progression Skeletal maturity • Risser sign Cosmesis Pain Disability PT Pain Mgmt Bracing Surgery Background Multi-center prospective study Clinical Group Scoliosis with apex T4 to L4 Degenerative or idiopathic 809 consecutive patients Radiographic analysis full length, standing films Cobb angle, apical level of deformity, sagittal plane lumbar alignment Health assessment questionnaires ODI / SRS-29 / SF-12 Classification System Apical level Lumbar lordosis modifier Intervertebral subluxation modifier Global Balance modifier Background Adult Scoliosis Classification 1. Type Type I Type II Type III Type IV Type V Thoracic only Upper Thoracic major Lower Thoracic major Thoraco-lumbar major Lumbar major no other curves Apex T9-T10 Apex T9-T10 Apex T11-L1 Apex L2-L4 2. Modifiers Lumbar Lordosis A : marked >400 B : moderate 0-400 C : no lordosis, Cobb >00 Global Balance Intervertebral Subluxation 0 : none at any level + : max = 1-6mm ++ : max >7mm N Neutrally balanced <4cm P Positively balanced 4-9.5cm VP Very Positive >9.5cm Purpose Adult Scoliosis Classification Reliable classification with significant correlation to clinical symptoms Prediction of treatment patterns and surgical rates ??? Materials & Methods 1. Clinical group • • • • Spinal Deformity Study Group database Prospective, consecutive 809 patients review Ages > 18 y.o. Thoracolumbar or lumbar major scoliosis •Type IV and Type V deformities only. 2. Health questionnaires • Oswestry Disability Index (ODI) • Scoliosis Research Society instrument (SRS-22) • Short From 12 (SF-12) Materials & Methods 3. Radiographic parameters • • • • Full-length standing films Frontal Cobb angle, Apical level, Sagittal lumbar alignment (T12-S1), Sagittal Balance N Neutrally balanced <4cm P Positively balanced 4-9.5cm VP Very Positive >9.5cm Lumbar Lordosis A : marked >40° B : moderate 0-40 ° C : no lordosis, Cobb >0° Intervertebral Subluxation 0 : none at any level + : max = 1-6mm ++ : max >7mm Materials & Methods 4. Treatment approach • Surgical vs. non-surgical • If Surgical: • Anterior, Posterior, circumferential • Use of osteotomies • Extension of fusion to sacrum 5. Data Analysis • Treatment Analysis regarding • HRQOL measures • SRS-22, ODI, SF-12 • Correlation analysis • Classification types vs. treatment given Results Patients Distribution 806 thoracolumbar/lumbar major deformities – Type IV – Type V n=311 n=495 – Mean age 53.1 y.o. (+/- 15.3) – 700 Females (87%) – 106 Males (13%) Results Surgical rates Rates of operative treatment – Lordosis modifier B vs. A (51% vs. 37%, p<0.05), trend for A vs. C (46%) – Subluxation modifier ++ vs. 0 (52% vs. 36 %, p<0.05), trend vs. + (42 %) – Sagittal Balance N vs. VP: 39% vs. 59%, p<0.05 Results Treatment Analysis: Type IV, V curves 92% highest level of fixation above apex of major curve. 97% lowest level of fixation below apex of major curve. 10% to level of sublux, 87% at least one level beyond Fusion to sacrum Apical Level Trend for type V patients more likely to have fixation to sacrum (p=.074) Lordosis Modifier mod B patients more likely fusion to sacrum than mod A patients (p=.041) Sagittal Balance Modifier increasing positive balance: more likely fixation extended to the sacrum. (mod N: 59%, mod P: 80%, mod VP: 88%) (all p<0.05) Results Treatment Analysis: Type IV, V curves Surgical Approach Anterior only – mostly lordosis modifier A – Subluxation modifier 0 – Sagittal balance modifier N Circumferential: – trend most common modifier B – Most commonly subluxation modifier ++ Posterior only: – mostly lordosis modifier C – Sagittal balance modifier VP Use of osteotomies Lordosis modifier A vs. C – 25% vs. 50% p=0.01 Sagittal balance N vs. VP – 25% vs. 53% p=0.01 Results Main findings Treatment • Good lordosis (modifier A) less likely to have surgery • Most likely to require surgery: • loss of lordosis (C), • marked subluxation (++) • sagittal plane imbalance (VP) If surgery • Cross level of subluxation • Osteotomies to realign sagittal plane • lordosis modifier C gets most likely to require osteotomy • fusion to sacrum: with increasing sagittal imbalance, lost lordosis Discussion - Conclusion Adult scoliosis classification Clinical Impact established: – HRQOL – Treatment….non-op vs. surgical – Surgical strategy…we’re getting there How about results of treatment ? Work toward surgical guidelines 2 yr f/u Discussion - Conclusion Adult scoliosis classification Reliable Clinical impact • disability • surgical rate Surgical strategy ? Can we broaden to a: Comprehensive Adult Deformity Classification Classification of Adult Deformity Type I II III IV V Type K thoracic-only curve (no other curves) upper thoracic major, apex T4-8 lower thoracic major, apex T9-T10 thoracolumbar major curve, apex T11-L1 lumbar major curve, apex L2-L4 no scoli (<100), principal sagittal plane deformity Lumbar Lordosis Modifier A B C marked lordosis >400 moderate lordosis 0-400 no lordosis present Cobb >00 Subluxation Modifier 0 + ++ no intervertebral subluxation any level maximal measured subluxation 1-6mm maximal subluxation >7mm Sagittal Balance Modifier N P VP normal, <4cm positive SVA positive, 4-9.5cm very positive, >9.5cm Next Steps Adult scoliosis classification Refine Classification • Pelvic modifier • Co-morbidity index • Patient expectation scale Longitudinal follow up • who responds well to conservative care • who benefits (how much) from surgery •Complications ? Surgical analysis (2yr f/u) • what strategies are most effective