3._Menopause_&_HRT
advertisement

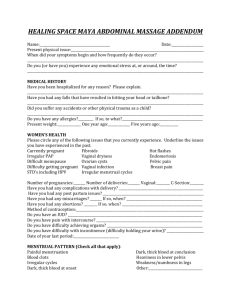
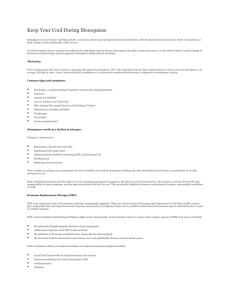
Menopause and HRT Dr. Huda Muhaddien Muhammad MBCHB ,FICOG, CABOG Menopause refers to final menstrual period (from the Greek meno –month- ,– pausos- ending ) . Represents a watershed reproductive life of a women . in the The average age of the menopause in the western women is approximately 52 years. Climacteric (from the Greek klimakter –rung of ladder-) : Signifies a major movement on life’s ladder. Is often used synonymously with (perimenopause or the changes). Is transition from the reproductive to non reproductive state. Occurs as a result of loss of ovarian follicular activity leading to a fall in E2level below the level needed for endometrial stimulation. It can only be said to have 12 consecutive months of amenorrhea . Can occurs suddenly . For most of the women there is gradual changes in the menstrual pattern in the years preceding the menopause as the ovarian activity fluctuates , which may be accompanied by troublesome symptoms; this is often called the perimenopause Surgical menopause: occurs when functioning ovaries are removed as in TAH &BSO for malignancy or severe endometriosis. Iatrogenic menopause induced by treatment as radio-chemotherapy or using GnRh analogues for a variety of conditions . Premature menopause : occurs if the menopause happens before the age of 45 . 1% of women under 40 years , 0.1 % under 30 years . It is one of the more common causes of the primary and secondary amenorrhea . the cause is usually unknown . Well established causes of POF should be excluded:- Primary causes: 1) Chromosomal disorders as Turner’s fragile X. 2) Auto -immune disease as hypothyroidism, Addison’s, myasthenia gravis. 3) Enzyme deficiencies as galactosaemia ,17 α- hydroxylase definiecy. Secondary causes: 1) Surgical menopause oophorectomy . after bilateral 2) Chemotherapy or radiotherapy. 3) Infections varicella. like TB , mumps, malaria, Pathophysiology: As the ovary ages the remaining follicles ( least sensitive to gonadotrophins) are increasingly less likely to mature. Ovulation declines and ovarian function gradually declines. The 1st endocrine change is a fall in Inhibin production by the ovary ( a glycoprotein that inhibits production of FSH ). Eventually the level of estradiol production is no longer sufficient to stimulate endometrial proliferation and menopause ensues. Further decline in estradiol levels over subsequent years has effects on all estrogen – responsive tissues. Menopause may only be a single event .but is represents a significant change in hormonal milieu and affects her future health and quality of life. Investigations : In most cases the diagnosis is pretty straightforward and doesn’t require any further investigation It is mandatory to investigate women suspected of undergoing premature menopause. What investigations: FSH ( a level > 30 IU/L is considered diagnostic of menopause). There is no value of measurement of E2, progesterone ,testostosterone in the diagnosis of the menopause. T4 & TSH should be checked if there clinical suspention Further assessment for screening for significant diseases in late years and introduce appropriate preventive measures: 1) Breast screening and mammography. 2) Endometrial assessment for abnormal bleeding. 3) CV disease risk assessment. 4) Skeletal assessment including bone density estimation and fracture risk assessment Effects of the menopause : women’s experiences will vary enormously , some women have no symptoms at all; while others can have a dreadful time with debilitating symptoms that stop them functioning properly. The effects vary chronologically and are categorized as following a/ Short term (0-5 years): •Vasomotor symptoms e.g. hot flushes ,night sweats. •Psychological symptoms e.g. labile mood ,anxiety and tearfulness . •Loss of concentration ,poor memory. •Joint aches and pains. •Dry & itchy skin. •Hair changes. •Decreased sexual desire. b/ intermediate (3-10 years): •Vaginal dryness, soreness. •Dyspareunia. •Sensory urgency. •Recurrent UTIs. •Urogenital prolapse. c/ long term ( >10 years ): •Osteaporosis. •Cardiovascular disease . •Dementia. Genitourinary problems : Urogeniotal atrophy is common observational in postmenopausal women which increases with age. Vaginal atrophy results in loss of the normal architecture within the vaginal epithelium, reducing its secretions and elasticity and making it more prone to trauma, dryness, spontaneous bleeding and infection. Clinically this manifests as vaginal dryness, Itching, dyspareunia , vaginal pains, bleedings, discharges , and infections . Distal urethra and trigone of the bladdor are also prone to atrophy as a result of estrogens deficiency . This can lead to urethral syndromes ( urinary frequency and dysuria in the absence of infection) , this is respond well to local vaginal estrogen. Thinning of the trigon and urethral mucosa lead to a more sensitive and trauma prone bladder which in turn leads to sensory urgency and recurrent UTI . Also this will respond to local estrogen. Loss of estrogen plays a role in more widespread pelvic floor dysfunction leading to weakening of the supporting tissues and ligaments ( already had been damaged by childbirth) thus increase the incidence of prolapse and stress urinary incontinence . Long term effects: These conditions often develop without obvious clinical manifestation in the early post menopause , but pose a significant economic burden for future particularly with an increasingly ageing population. Those women underwent premature menopause will spent a prolonged period without estregens so they are at high risk . Osteoporpsis : Is defined as a skeletal disorders characterized by compromised bone strength predisposing to an increased risk of fracture . 20 % of our bone is composed from trabecular bone ( shock absorbing capacity) Oestrogen acts an antiresorptive agent on the trabecular bone so E2 deficiency after menopause is characterized by unprecedented fall in bone density which ultimately may lead to increase risk of osteoporotic fractures Bone strength is a reflection of bone quality and density . Current strategies of treatment target preventive treatment at individual identified as high risk of subsequent fracture . Recent NICE guidance favours a very limited role for preventive treatment for women under 75 years unless if there was history of previous fracture . Cardiovascular disease : Is relatively uncommon before menopause . Oestrogen has against CHD. a productive influence Early menopause without estrogens is associated with 2-4 increased fold of CHD. Menopause is associated with adverse metabolic changes (raise in LDL and cholestrol and fall in HDL). Loss of oestrgen lead to vasoconstriction and atherogenesis. Dementia is much more common among women , but the evidence for a role of estrogen and menopause in the pathophysiology of cognitive decline and dementia is conflecting. Management the menopause is natural event and for many women there is no need to manage it at all. Awareness of the long term implications, such as osteoporosis and CV disease should be part of good preventative medicine. The menopause consultation : History : Concentrate on ascertaining the frequency and severity of menopausal symptoms and their impact on day to day activities. Enquiry into any sexual problems , in particular vaginal dryness soreness, and bladder symptoms should be recorded Family and personal history should focus on risk factors for CV disease , osteoporosis ,breast cancer ,thrombosis and ovarian cancer. Any previous treatment and S/E should be noted . Explanation teatments the potential s/E of all Physical examination : Abdominal examination . Breast examination . Cervical smear. Bimanual assessment of the uterine size. Assessment of the vagina for any atrophy, prolapse or incontinence. Lifestyle : The menopause could be an ideal time to look at changes in diet and exercise and build for a healthy future to maximize health potential . Smoking cessation , eating sensibly and avoid extra weight . Regular physical activity Alternative and complementary therapies: There is little evidence for the safety and efficacy of most of them. as in the following; 1-Non prescriptive treatment Lifestyle changes (diet and exercise). Complementary therapies : acupuncture, reflexology and magnetism. Herbal remedies : black cohosh (actaea racemosa), dong quai ( angelica sinensis ), evening primose oil , gingkp , ginseng, st jonn’s wort ( hypericum perforatum). Bio- identical hormones : natural progesterone gel , DHEA , phytoestrogens ( isoflavones, red clover ). Prescription: α-adrenergic agonist as clonodine. Beta blockers as propranolol Selective serotonin reuptake inhibitors: venlafaxine, fluoxetine, paroxitin ,citalopram .gabapentin HRT : estrogen alone, oestrogen and progestogen combintion , progestogen alon SSRI used for hot flushes in short trials ,only used for those who cannot take HRT. For osteoporosis , the bisphosphonates are the principle of drug used . Alternative include strontium and raloxofene ( type of SERM). Those drugs have significant S/E and should be used for women over 60 year. Para thyroid hormone is reserved for women with very high risk. Hormone replacement therapy: Is the principle treatment available for troublesome menopausal symptoms. Acts by replacing the hormones that are normally produced by the human ovary at physiological levels. Oestrogen is the main hormone and is either given alone or in combination with progestogen , which should be given for all non hysteroctemised women. Testosterone can also be given in conjuction with oestrogen. Most HRT treatment come in combination. Oestrogen : There are different types of oestrogen available. 1- oestradiol ( transdermal, gel ,implant). 2- oestradiol valerate. 3- conjucated equine oestrogens. 4- oesterone sulphate. 5-oesteriol ( vaginal only). Can be given by different doses and by different routes. The lowest dose should be used. Non –oral route ( especially transdermal ) avoid the 1st pass effect, and are considered more physiological as they release oestradiol to the circulation, rather than oesteron. Avoiding thr 1st pass effect reduces the impact on various metabolic parameters, such as haemostatic and coagulation system , so seems a better option in women with personal or family history of VTE or known liver abnormalities. Non oral routes are expensive , there can be logiical problema administerating progestogen component simultanously . Subcutaneous implants is reserved for those women who hysteroctemised with removal of both ovaries , ( repeated every six months). Implants also testosterone. allow the addition of Progesterone: In HRT , progetogens ( synthetic progeterone ) are added for at least 10 days /calender month to mimic menstrual cycle . This will reduce the risk of endometrial hyperplasia and cancer associated with prolonged use and unopposed oestrogen. It can be given either cyclically mimickining a natural 28 day cycle -28 days result in withdrawal bleeding ( used for perimenopausal women; Or it can be given continuously to prevent any bleeding –so called no bleed _ treatment ( used for post menopausal women) Types of progetogens used in HRT : C -19 nor testosterone derivatives norethisterine ( transdermal levonogesterel (transdermal, intrauterine). : ) C-21 progesterone derivatives : dydrogesterone, medroxyprogesterone acetate , cyproterone acetate . C -17 derivatives : drospirenone . Progesterone: micronized progesterone ( vaginal gel , pessary, suppository. S/E are common esp in 1st few months and can be alleviated by changing the type or the route Levonogesterole IUD can be used in women who canot tolerate systemic progestogenes . Progestogen is not used for hystorectomized women. Testosterone : 50% from the ovaries and 50% from the fat and adrenal glands . Menopause doesn’t affect testosterone level but decrease SHBG level this may lead to increase the level of free testosterone . Surgical or chemoradiation induced menopause can lead to relatively deficient testosterone. May be presented as loss of libido, fatigue. Risks and benefits of HRT: Still uncertainty and controversies present about HRT use and what exactly the risks are and how relevant they are to the majority of healthy post menopausal women. HRT Is an extremely effective treatment for menopausal symptoms and urogenital atrophy. is an effective treatment for osteoporosis, and appears to have beneficial effects on the cardiovascular system if it started around the menopause . Oestrogen is effective in relieving the hot flush symptoms within 4-6 weeks. Vaginal or topical oestrogens preperations have no significant systemic activity so can be used for those in whom HRT is contraindicated. Progestogen use with vaginal oestrogens is not necessary. For vaginal atrophy , vaginal oestrogen is applied daily for 2 week then with the improvement in the vaginal epithelium it can be reduced to once or twice weekly. This should be continued for at least 12 months at a low maintenance dose . Because of the uncertainty of its long term safety ,the regular authorities currently advice that HRT should not be used as a 1st line treatment for osteoporosis prevention as the potential risk outweigh the benefits. Protection against CVD and colon cancer is not an indication to consider HRT Risk ,benefits, uncertainty of HRT Benefits Vasomotor symptoms Urogenital symptoms Sexual function Stoke Osteoporosis Colon cancer Risks Breast cancer VTE Endometrial cancer Uncertainties CVD and stroke Alzheimer’s Ovarian cancer Risks of HRT: Breast cancer : small increase in risk within few years of starting HRT in healthy postmenopausal women . Risk is not increase with oestrogen only type The increase in the risk is associated with progetogen componant. Family history is important. Endometrial cancer : Unopposed oestrogen replacement therapy increases the risk of endometrial cancer. Any abnormal bleeding during HRT treatment should be investigated,although there is a small risk of malignancy. Ovarian cancer : Small increase in risk with long term (>10 y) treatment Venous thromboembolism : HRT increases the risk of VTE 2 fold with highest risk occurring in the 1st year. The background risk is increased with obesity , smoking and history of underlying thrombophilia such as factor V Lieden or who have previously suffered VTE. Transdermal HRT have less impact on heamostatic mechanism and lower risk of VTE. Coronary heart disease : Timing of oestrogen important. introduction is Women staring HRT shortly after menopause may have protective effect. Stroke ; Small increases in the risk with both oestrogen only and combined oestrogen and progestogen HRT, also its affected by age . Practical consideration : 1-For the majority of healthy symptomatic menopause women the potential benefits will outweigh any small risk. Contraindications to taking HRT: Absolute : suspected pregnancy, breast and endometrial cancer, uncontrolloed hypertension , known VTE, known thrombophilia and ostsclerosis. Relative :uninvestigated abnormal bleeding, large uterine fibroids, past history of benign breast disease , unconfirmed personal history or strong family history of VTE, chronic stable liver disease and migraine with aura. Selection which HRT regimen is a matter for the individual prescriber . Follow up should be arranged after about 3 months to check the treatment’s effectiveness and any persistent S/E. Treatment should be started at the lowest appropriate dose and can be increased if there is no symptomatic improvement after few months. Oestrogen related S/E: dose dependant and last for few months ( fluid retention, nausea ,headaches , breast enlargement, leg cramps and dyspepsia). Progestogen related S/E mostly like PMS (fluid retention , breast tenderness , headaches ,acne, mood swings , depression , irritability,bloating , constipation and increased appetite). If persist change the type . The average duration of treatment is 2-3 years depends on the indication and individual circumstances. it is recommended to take a minimum effective dose of HRT for the shortest duration. Premature menopause women better to take HRT until the age of 50. Once the condition is stabilized , women should be reviewed every 6 months ( individual risk of VTE, stroke and breast cancer should be balanced against the benefits that are gaining from the treatment ). Women on HRt should continue to participate in the national programmes for breast, cervical ,colorectal cancer. Stopping HRT should be gradually. Contraception should be continued until 2 years after the last period in women under 50 years; and 1 year for those above 50. Contraception could be condome ,or mirena as contraception and as part of HRT. Thank you