Conjugated estrogen
advertisement

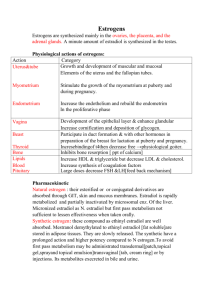
Hormone therapy in Ammenorrhea • A.Mehdizadeh .MD • Prof. of Gyn. • Iran Medical School Definition of amenorrhea • No period by age 14 in the absence of secondary sexual characteristics • No period by age 16 regardless of the presence secondary sexual characteristics • Secondary amenorrhea means lack of period at least 3 of the previous cycle interval or 6 months of amenorrhea Hormone therapy in ammenorrhea • • • • • Hypothyroidism Hyperprolactinemia Anovulation Hypothalamic ammenorrhea Premature ovarin failure • Hormon therapy in ammenorrhea • In the absence of exogenous estrogen treatment, they are at risk for developing osteopenia and osteoporosis. • Early coronary heart disease . • Developmentof symptoms of estrogen deficiency such as vasomotor flushes and genito-urinary atrophy that can be debilitating. Hormon therapy in ammenorrhea • Unless there is a specific contraindication to its use, women with POF should receive exogenous estrogen therapy. • Other strategies for protecting bone and heart health, including exercise, diet, adequate calcium and vitamin D intake, and the avoidance of smoking. Hormon therapy in ammenorrhea • • • • • 1- Absolute contraindications: Known or suspected breast cancer Known or suspected endometrial cancer Undiagnosed abnormal genital bleeding Active thromboembolic disorders Active liver & gallbladder diseases Hormon therapy in ammenorrhea 2-Relative contraindications: Heart diseases Migraine headaches History of liver disease History of gallbladder disease History of endometrial cancer History of thromboembolic events Hormone replacement therapy • • • • • Sequential estrogen- progestin therapy Continuous estrogen- progestin therapy Estrogen only therapy Seasonal regimen Progestin intrauterine device Estrogen formulation and routes of administration • Oral administration : Conjugated estrogen (0.625& 1.25 mg ) Micronized estradiol (1mg ) Ethinyl estradiol (o.o5mg & 5 mg ) • Transdermal administration • Vaginal administration- low dose method • Vaginal method- standard dose method • Estradiol implants • Percutaneous estrogen • Intranasal administration Hormon therapy in ammenorrhea • Oral contraceptives also may be used but contain greater amounts of hormones than are required and may thus be reserved for those who want to prevent even the possibility of random ovulation and pregnancy. • Androgen treatment cannot be recommended for women with POF.(acnea,hirsutism,hyperlipidemia) Progesterone regimens • • • • Medroxy progesterone acetate 5 mg Norethindrone acetate 1 mg Norethindrone 0.7 mg Micronized progesterone 200 mg • Progestin intrauterine device( Mirena- IUS) Progestin for hysterectomized women • In some special conditions should take : 1 - history of pelvic endometriosis 2- supracervical hysterectomy 3- history of endometrial carcinoma 4- history of endometrioid tumor of ovary Hormon therapy in Ammenorrhea • It is important to emphasize to young women with POF that they are distinctly different from older postmenopausal women and that the balance between the risks and benefits of hormone therapy for them also differs from that in postmenopausal women. • Because they are significantly younger, Their baseline risks for cardiovascular disease and breast cancer are much lower than those for older postmenopausal women. Hormon therapy in Ammenorrhea • Moreover, without estrogen therapy, their risk for later coronary heart disease may be increased, rather than decreased. • Hormone therapy should continue up to at least age of 50, in much the same way as endogenous hormone production does in normal women. Hormon therapy in Ammenorrhea • Although the likelihood of achieving pregnancy after diagnosis is only about 5-10%, some women with POF do conceive and approximately 80% of their pregnancies end in a healthy live birth. • However, there is no evidence that any form of treatment other than egg donation and IVF can increase the chance for pregnancy. Psychological and Emotional Support • Profound grief and a sense of loss for the children, are common in women after diagnosis of POF. • It also is important to emphasize that the diagnosis of POF does not imply or predict premature aging in any other way, something that many women understandably may fear. • . Women with POF also are at risk for developing related depression and anxiety disorders. • Consequently, refer them to a support group and to a therapist . Oral Administration The relative potencies of commercially available estrogens are of great importance when prescribing estrogen, and the clinician should be familiar with the potencies. Oral Administration Transdermal Patch Administration • The patches first used , contained an alcohol reservoir; but In the current generation of patches, the hormones are dissolved and distributed throughout the adhesive matrix. • In a study of women who had previously discontinued patches because of skin irritation (contact dermatitis), skin reactions were less common with the newer matrix patches. • The patches are designated according to the amount of estradiol delivered per day: from 14 to 100 micg. Transdermal Patch Administration • The first-pass effect may be important for lipoprotein effects. because , increase catabolism of LDL and increase production of apoprotein A-I with oral estrogen, but no effect with transdermal estrogen • Transdermal administration of 50 /mic,g estradiol twice a week is as effective as 0.625 mg oral conjugated estrogens. Clotting Factors • First-pass hepatic metabolism affects the synthesis of clotting proteins, markers of coagulation that can influence the risk of thrombosis and coronary heart disease events. • Oral estrogen increases factor VII and prothrombin I and 2 fragment, whereas transdermal estrogen decreases factor VII. Clotting Factors • Estrogen users who carried a factor V Leiden mutation or a prothrombin mutation had a 25fold higher risk of VTE than did women who did not use estrogen and did not have either mutation. • The women with a prothrombotic mutation who used transdermal estrogen had a VTE risk that was similar to that of women with a prothrombotic mutation who did not use estrogen. Myocardial Infarction Risk: • Both oral and transdermal administration of hormone therapy are associated with a decrease in myocardial infarction risk in observational studies. Effects in Smokers: • POF women who smoke may have a better cardiovascular response to transdermal estrogen than to oral estrogen. • Smokers receiving transdermal estradiol have decreased plasma viscosity and thromboxane B2 levels. • These results raise the possibility, that smokers may represent a group of women for whom transdermal estrogen would be an advantage. Carbohydrate Metabolism: • There is little difference between the oral and transdermal methods of delivery on carbohydrate metabolism. • Both methods have a beneficial impact on central abdominal fat content, glucose levels and insulin resistance, associated with a reduced risk of developing adult-onset diabetes mellitus. Breast Cancer Risk • Oral estrogens/progesterone decreased (IGF-I) by 26% and increased (SHBG) by 96% ,whereas no change occurred with transdermal estradioI. • High IGF-l and low SHBG levels are associated with increased breast cancer risk. Colorectal Cancer Risk • In a case-control study, both oral and transdermal hormone therapy reduced the risk for developing colorectal cancer. • When transdermal therapy involved estrogen alone, the benefit was even greater Vaginal Administration of Estrogen-Very Low-Dose Method • Some patients do not gain full relief from the symptoms of vaginal atrophy with oral or transdermal administration of estrogen. • In addition, there are many women who desire the genitourinary effects of estrogen but either must or wish to avoid systemic therapy. • Vaginal treatment is especially helpful when a rapid response is desired. Vaginal Administration of Estrogen-Very Low-Dose Method • Many clinicians believe that estrogen administered intravaginally is not absorbed, and systemic effects can be avoided. This is not the case. • Estrogen in creams is absorbed very readily from a vagina with immature, atrophic mucosa. • Indeed, the initial absorption is rapid, and relatively high circulating levels of estrogen are easily reached. • As the vaginal mucosa matures, absorption decreases. Vaginal Administration of Estrogen-Very Low-Dose Method • This decline takes approximately 3-4 months, after which lesser but still significant absorption takes place. • Effective treatment of vaginal atrophy with minimal absorption can be achieved with the administration of 0.3 mg conjugated estrogens, 2-3 times per week. • Treatment with a vaginal cream longer than 6-12 months requires endometrial surveillance. Vaginal Administration of Estrogen-Very Low-Dose Method • Estring is a 55-mm diameter silicone ring that contains 2 mg estradiol, with a release rate of 7.5 micg/day for 90 days. • No change in endometrial thickness was observed after I year of treatment. Vaginal Administration of Estrogen-Very Low-Dose Method • Vagifem is a tablet that contains 25 micg estradiol, and the initial dose of I tablet daily produces relief from atrophic symptoms within 2 weeks. • Endometrial thickness has been reported to not change from baseline • smaller dose tablet, 10 micg, also improves vaginal atrophy, but it is not as effective as the larger dose. Vaginal Administration of Estrogen-Standard Dose Method • A vaginal ring (FemRing) that releases estradiol acetate provides 50 or 100 micg estradiol per day over a 3-month time span. • Blood estradiol level is similar to those achieved with oral and trans dermal methods. • Endometrial protection requires the addition of a progestin in the presence of a uterus. Estradiol Implants • Estradiol pellets are available in doses of 25, 50, and 75 mg for subcutaneous administration twice yearly. • Significant blood levels of estradiol wiIl persist for up to 2 years after the last insertion. • Women receiving pellets be monitored with blood estradiol levels, and levels greater than 200 pg/mL (and preferably, 100 pg/mL) should be avoided by a greater interval between insertions. Percutaneous Estrogen • Transdermal estradiol can also be administered by a gel, emulsion, or spray. • The gel, is applied once daily on an arm, anywhere from the wrist to the shoulder, or the thigh, without rubbing or massaging . • The emulsion, usuaIly two packets are applied daily. • transdermal spray, the usual dose is one spray daily to the forearm . Estrogen-Progestin Sequential and Continuous Regimens • Hormone therapy initially consisted only of sequential regimens that were logical reflections of the cyclic estrogen and progesterone patterns in a menstrual cycle manner. • Clinical trials established the doses and durations for progestin administration that would effectively protect the endometrium against unchecked proliferation. • Progestin withdrawal bleeding occurs in 80-90% of women on a sequential regimen, and for this reason the continuous combined method of treatment evolved to improve patient continuance that was adversely affected by bleeding and other symptoms triggeredby the cyclic hormonal changes. • The addition of a daily dose of a progestin to the daily administration of estrogen allowed the progestin dose to be smaller, provided effective protection against endometrial hyperplasia, and resulted in amenorrhea within I year of treatment in 80-90% of patients. • In the sequential regimen, estrogen is administered daily and progestins for 2 weeks of every month, using the comparable doses of the following progestins. • 5 mg medroxyprogesterone acetate, or • 0.7 mg norethindrone, or • 1.0 mg norethindrone acetate, or • 200 mg micronized progesterone. • In the daily continuous, combined regimen, progestins are combined with estrogen in the • following comparable doses . • 1.5 or 2.5 mg medroxyprogesterone acetate, or • 0.35 mg norethindrone, or • 0.5 or 1.0 mg norethindrone acetate (0.1 mg dose is available), or • 100 mg micronized progesterone or • 2 mg drospirenone or • 2 mg dienogest. • These hormonal regimens are combined with daily calcium supplementation (500 mg with a meal) and vitamin D (1,000-2,000 Iu daily). • • • • • There has been a progressive decrease in dose used for hormone therapy. For many years, the standard dose of estrogen was 0.625 mg conjugated estrogens, 1-2 mg micronized estradiol, 1-2 mg estradiol valerate, or equivalent doses of other estrogens such as 5 micg ethinyl estradiol. Lower doses have been proven 0n the average to be as effective as these "standard" doses, providing clinicians and patients with more options. Conjugated estrogens in a dose of 0.3 or 0.45 mg effectively produce a gain in bone density when combined with 1.5 mg medroxyprogesterone acetate, and a dose of 0.5 mg micronized estradiol produces comparable effects. The 0.45/1.5 mg and 0.3/1.5 mg conjugated estrogens/ medroxyprogesterone acetate combinations improve vaginal atrophy, reduce hot flushing, and improve measures of sexual function in a pattern that is quantitatively and qualitatively similar to the 0.62512.5mg combinationwith less mastalgia • Two metabolites of progesterone, allopregnanolone and pregnanolone, are believed to be responsible for progesterone's unique sedative effect. • Treatment regimens with micronized progesterone should be taken at bedtime, and these estrogen-progesterone combinations are a good choice for women with sleep difficulties. Progestational Side Effects • Many women do not tolerate treatment with progestational hormones. • Typical side effects include breast tenderness, bloating, and depression. • changing to a regimen containing norethindrone or norethindrone acetate has been beneficial • Can the progestational agent be administered less frequently? • Daily combination program effectively prevents endometrial hyperplasia. • A sequential regimen that incorporates progestin exposure for less than 14 days has over time an increased risk of endometrial hyperplasia. . • Experience with extended cycle regimens is very limited. • The administration of medroxyprogesterone acetate every 3 months was associated in I study with longer, heavier menses and unscheduled bleeding and a 1.5% incidence of hyperplasia at I year, whereas in another study, overall bleeding was less, but the incidence of hyperplasia was approximately4%. • An annual endometrial biopsy is strongly recommended in estrogen users exposed only intermittently to progestin treatment • Some patients are very sensitive to medroxyprogesterone acetate. • these patients are often relieved of their symptoms by ,switching to norethindrone. • Progesterone can be administered in a vaginal gel that allows the delivery of very low doses that can effectively protect the endometrium with low systemic levels because of a first-pass effect on the uterus. • The administration of 90 mg every 2 days produces secretory changes in the endometrium. Activated Protein C (APC) Resistance and Risk of VTE. • Oral estrogen increases APC resistance, whereas transdermal estrogen has no significant effect on this marker. • Based on this difference, one would predict that transdermal delivery of estrogen would be less likely than oral delivery of estrogen to be associated with venous thromboembolism (VTE). Transdermal Patch Administration • The concentration of estrogen in the hepatic portal system after oral administration is 4-5 times higher than that in the periphery. • Because of first-pass metabolism in the liver, oral estradiol results in a circulating estrone to estradiol ratio of approximately 3; with transdermal administration the ratio is I. Metabolic Syndrome : • In a 3-month randomized trial involving 50 obese women with metabolic syndrome, oral estradiol therapy worsened markers of the metabolic syndrome, including insulin resistance, suggesting a worsening of cardiovascular risk, whereas transdermal estradiol had minimal effects. Vaginal Administration of Estrogen-Very Low-Dose Method • long-term treatment requires US monitoring of endometrial thickness with biopsy when indicated. • For women who are breast cancer survivors and are considering this treatment, clinicians and patients must accept a small but real unknown risk Lipids and Hepatic Enzymes • Both oral and transdermal estrogen reduce total cholesterol, LDL cholesterol, and lipoprotein(a). • Compared with transdermal estrogen, oral estrogen produces significantly greater elevations in HDL cholesterol and increases triglycerides, whereas transdermal estrogen decreases triglyceride levels.