The Period surrounding menopause
advertisement

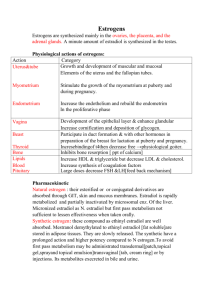
Menopause Permanent cessation of menses for at least 1 year FSH > or = 40 IU/ml Signs of hypoestrogenism Perimenopause The Period surrounding menopause: Before, during, and after Mean age of onset: 46 yrs. Mean duration: 5 yrs. (2-8 yrs.) Only one marker: Menstrual irregularity ► In only 10% of women, menstuation ceased abruptly with no period of prolonged irregularity. What Happens follicular quality and/or quality INHIBIN Level FSH Levels with normal or even increased estradiol levels until 6 mo. to 1 yr Initial Evaluations Medical History and Physical Examination Breast and Pelvic Examination Pap Smear (repeat every 1 yrs) Mammography if >40 yrs (repeat every 1 yrs) Evaluation of General Medical Conditions Detection of common medical problems as early as possible: Hypertention, Heart diseases, Diabetes Mellitus, Cancer STD screening TSH screening at 40 yrs and q 2 yrs after 60 yrs of age Occult blood after 50 yrs of age Evaluation of vision, hearing, and teeth impairments Hormonal Levels FSH (10-20) > LH (3) ► FSH (T1/2 = 3-4 hr)has longer halflife than LH (T1/2 = 20 min) ► There is no negative feedback system like Estrogen for LH Changes in circulating hormone levels at menopause Premenopause Postmenopause Estradiol 40-400 pg/ml 10-20 pg/ml Estrone 30-200 pg/ml 30-70 pg/ml Testosterone 20-80 ng/dl 15-70 ng/dl Androstenedione 60-300 ng/dl 30-150 ng/dl Age Of Menopause The most important determinant factor is genetics. ► Mothers and daughters tend to experience menopause at the same age Factors that cause slightly earlier menopause Tobacco use (about 1.5 yrs) Nulliparity Living in high altitude Heavy physical exercise Undernurishment and thinness Vegetarrian diet IUGR in late gestation Previous Hx. Of TAH or endometrial ablation Irregular menses at early 40s Age Of Menopause These factors don’t affect the age of menopause Use of OCPs Socioeconomic states Marital status Age of menarche Parity Race Height Premature ovarian failure: Spontaneous menopause before 40 yrs of age Problems Unopposed Estrogen AUB risk of endometrial cancer Hypoestrogenism Vasomotor, emotional, atrophic, cognitive, cardiovascular, and musculoskeletal impacts Estrogen-Progestin Therapy Indications of ERT Menopause Hot Flashes Vaginal Atrophy Urinary Tract Symptoms High risk for osteoporosis (Family Hx., Cigarette smoking, Low body weight) High risk for cardiovascular disease (Previous myocardial infarction, Hypertention, Family Hx., Cigarette smoking) Contraindications for ERT Absolute Pregnancy Undiagnosed uterine bleeding Active thrombophlebitis Current gallbladder diseases Liver diseases Neuro-ophthalmologic eye diseases Relative Hx. of breast cancer Hx. Of recurrent thrombophlebitis or thromboembolic disease Migraine headache ? Epilepsy ? Indications for Pretreatment Endometrial Biopsy: Characteristics associated with high risk endometrial pathology Hx. of unopposed estrogen therapy During-treatment Endometrial Biopsy Clinician’s anxiety Patient’s anxiety Treatment with unopposed estrogen AUB during treatment Endometrial thickness > 4 mm D&C Cervical stenosis Abnormal pelvic exam Suspicious endometrail biopsy results Patient’s pain intolerance Abnormal Uterine Bleeding Management of postmenopausal AUB Complex hyperplasia or malignancy Abnormal Bleeding Endometrial Biopsy Tissue insufficient for diagnosis Simple hyperplasia or normal pathology Ultrasound and/or office hysteroscopy Hysteroscopy and fractional curettage Atypical hyperplasia or malignancy Abnormal Normal or simple hyperplasia Normal Hysterectomy (or other definitive therapy) Group therapy (repeat endo. Biop. In 6 mo) Biopsy Results Endometrial biopsy results in post-menopausal period: 1-2% Cancer 50% Normal 3% Polyps The rest atrophic Plans for Treatment: Cancer and/or Atypical Hyperplasia HYSTERECTOMY Simple hyperplasia Med. Prog. Acetate 10 mg/day for 1214 days per month Nonresponders (6-7%) Re-evaluate after 3-4 months ► If persistant AUB or Hyperplasia again D&C ► If hyperplasia regressed conyinue progestrone therapy until vasomotor symptoms begin and/or no withdrawal bleeding anymore. Evaluate for ERT. Conterception Menopause The Hot Flashes Premenopausal 10-25% of women Postmenopausal No flashes Daily flashing Duration Other causes Psychosomatic Stress Thyroid Disease Pheochromocytoma Carcinoid Tumor Leukemias Cancer 15-25% 15-20% 1-2 years average 5 plus years: 25% Menopause Menopause and the Perimenopausal transition High cholestrol High LDL LDL entry into endothelium LDL oxidation Monocyte adherence, entry, and conversion to macrephages Foam cells Fatty streak Smooth muscle cell proliferation and migration Endothelial injury and dysfunction Vasoconstriction Thrombus Atherosclerotic fibrous plaque Consequences Cardiovascular The optimal cholestrol/lipoprotein profile ► Total cholestrol: Less than 200 mg/dl ► HDL cholestrol: Greater than 50 mg/dl ► LDL cholestrol: Less than 130 mg/dl ► Triglycerides: Less than 250 mg/dl Risk of MI ► Total cholestrol > 256 mg/dl ► Triglycerides > 400 mg/dl ► HDL cholestrol < 50 mg/dl Risk of Heart diseases based on Chol/HDL ratio ► < 2.5 Lowest risk ► 2.5-3.7 Below average risk ► 3.8-5.6 Average risk ► 5.7-8.3 High risk ► > 8.3 Dangerrous Consequences Osteoporosis Excess alcohol Diet Excess caffeine & low calcium Low Vit D Low calcium Age Heparin Race Anticonvulsants Environmental factors Drugs OSTEOPOROSIS Lack of estrogen Corticosteroids Body weight Thyroxine Diseases Lifestyle Sedentary Smoking Pathophysiologic factors Consequences Osteoporosis Commonly associated injuries: ► Femoral Head Fx. ► Hip Fx. ► Vertebral Fx. ► Colles’ Fx ► Teeth Loss Specific causes Drugs Heparin, anticonvulsants, high intake of alcohol Chronic Disease Renal and hepatic Endocrine diseases Excess glucocorticoids Hyperthyroidism Estrogen deficiency Hyperparathyroidism Nutritional Calcium, phosphorus, vitamin D deficiencies Consequences Osteoporosis Laboratory Exams ► Ca, Phos, ALP, PTH ► RFT ► CBC, ESR, Protein Electrophoresis ► TFT Alternative Treatments: ► Calcium-Vit D Supplements ► Bisphosphonate: ETIDRONATE 400 mg for 2 weeks then ► ► ► 12 weeks drug free OR ALENDRONATE (FOSAMAX Tabs) 5-10 mg/day Calcitonin: 100 IU/day SQ OR 200 IU/day Intranasal Raloxifen (EVISTA 60 mg Tabs): Hot flashes, risk of breast cancer Tibolon: 2.5 mg/day Hormone Replacement Therapy The Sequential Program for Oral Postmenopausal Hormone Therapy Daily Estrogen 0.625 mg conjugated estrogens, or 1.25 mg estropipate, or 1.0 mg micronized estradiol or equivalent doses of other estrogens Monthly progestin 0.7 mg norethindrone, or 200 mg micronized progestrone, or 5 mg medroxyprogestrone acetate, or equivalent doses of other progestins given daily for 2 weeks every month Combined with daily calcium supplementation (500mg with a meal), and vitamin D (400 IU in winter months and 800 IU for women over age 70). Hormone Replacement Therapy The Continuous Combination Program for Oral Postmenopausal Hormone Therapy Daily Estrogen 0.625 mg conjugated estrogens, or 1.25 mg estropipate, or 1.0 mg micronized estradiol or equivalent doses of other estrogens Monthly progestin 0.35 mg norethindrone, or 100 mg micronized progestrone, or 2.5 mg medroxyprogestrone acetate, or equivalent doses of other progestins Combined with daily calcium supplementation (500 mg with a meal), and vitamin D (400 IU in winter months and 800 IU for women over age 70). Hormone Replacement Therapy Relative estrogen potencies Estrogen FSH Levels Liver Pro.s Bone density Conjugated estrogen 1.0 mg 0.625 mg 0.625 mg Micronized estradiol 1.0 mg 1.0 mg 1.0 mg Estropipate (piperazine estrogen sulfate) 1.0 mg 1.25 mg 1.25 mg Ethinyl estradiol 5.0 μg 2-10 μg 5.0 μg Estradiol valerate ― ― 1.0 mg Esterified estrogen ― ― 0.625 mg Transdermal estradiol ― ― 50 μg Hormone Replacement Therapy Usual initial dosages of estrogens used for HRT Oral ► Conjugated equine estrogens Synthetic conjugated estrogens Micronized estradiol Esterified estrogens Estropipate Ethinyl estradiol Topical Patch ► 17 b-Estradiol Vaginal ► Conjugated equine estrogens 17 b-Estradiol Injectable ► Estrone Estradiol cypionate in oil Estradiol valerate in oil 0.625-1.25 mg daily 0.625-1.25 mg daily 1-2 mg daily 0.625-1.25 mg daily 0.625-1.25 mg daily 0.02 mg daily 0.025-0.1 mg patch once or twice weekly 0.2-0.625 mg, 2-7 times per week 1 mg, 1-3 times/week 0.1-1.0 mg weekly 1-5 mg IM weekly3-4 10-20 mg IM / 4 weeks Effects of HRT Cardiovascular A favorable impact on the circulating lipid and lipoprotein profile, especially a in total cholestrol and LDL-cholestrol and in HDL-cholestrol A direct antiatherosclerotic effect in arteries Augmentation of vasodilating and antiplatelet aggregation factors, specifically nitric oxide and prostacyclin (endothelium-dependent mechanisms) Vasodilation by means of endothelium-independent mechanisms Direct inotropic actions on the heart and large blood vessels Improvement of peripheral glucose metabolism with a subsequent decrease in circulating insulin levels Antioxidant activity Favorable impact on fibrinolysis, at least partially mediated by endothelial nitric oxide and prostacyclin synthesis Effects of HRT Cardiovascular Inhibition of vascular smooth muscle growth and migration – intimal thickening Protection of endothelial cells from injury Inhibition of macrophage foam cell formation Reduced levels of angiotensin-converting enzyme and renin Reduction of P-selection levels Reduction of homocystein levels Effects of HRT Cardiovascular 50% risk of coronary artery disease 45% risk of myocardial infarction risk and extension of stroke even in hypertension or smoking basal insulin levels and Insulin resistance Effect of estrogen on BP ► epinephrin associated BP ► BP with idiosyncratic effect HRT in hypertensive patient: ► Control BP q 6 mo. ► If BP variability control BP q 3 mo.