Aspect of Anaerobic Infection
advertisement

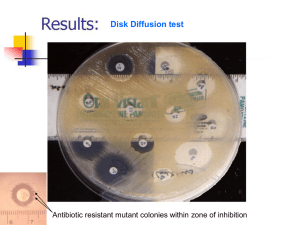
Clinical and lab aspect of anaerobic infection Ali Somily MD, FRCPC,ABMM Classification 1. Anaerobic spore forming bacilli 2. 3. 4. 5. 6. (Clostridia) Gram negative bacilli non-sporing (Bacteroides) Anaerobic streptococci (Peptostreptococcus) Anaerobic staphylococcus (Peptococcus) Gram negative diplococci (Veillonella) Gram positive bacilli (Actinomyces) Propionibacterium Bacteroides fragilis Fusobacterium nucleatum Antimicrobiolial Sensitivity • All of them resistant to aminoglycosides – Gentamicine – Tobramycin – Amikacin • Almost all are sensitive to metranidazole (flagyl) Anaerobiosis • Lack cytochrome-cannot use oxygen as hydrogen • acceptor Most Lack – Catalase – Peroxidase • Contain flavoprotein so in the presence of oxygen • produce H2O2 which is toxic Some lack enzyme superoxide dismutase so many killed , peroxide and toxic radicales enzyme like fumarate reductase must be reduced form to work Anaerobic chamber NONSPORING ANAEROBES HABITAT I : • These organism are normal flora in: • A. Oropharynx • eg. 1. Bacteroides melaninogenicus Now called provetella melaninogenicus – 2. Fusobacteria – 3. Veillonella HABITAT II: • B. Gastrointestinal tract – Found mainly in the large colon in large numbers – Total number of anaerobes = 10 11 – While all aerobes (including E. coli) = 10 4 – examples are (1) B acteroides fragilis (2) Bifidobacterium species • C. Female genital tract (mainly in the vagina) CLINICAL ASPECTS • ANAEROBES ARE INDIGENOUS FLORA OF SKIN & MUCOUS MEMBRANES • NORMALLY CONTAINED AWAY FROM INTERNAL STERILE BODY SITES • HIGH MORBIDITY & MORTALITY INFECTIONS CAUSED BY ,NONSPORING ANAEROBES • A. The head, neck and respiratory tract • B. The lower abdomen and the pelvis FEATURES OF ANAEROBIC INFECTIONS • Characterized by foul smell • Gas formation • Infections are always near to the site of the body which are • • • • • • habitat. Deep abscesses The infections are also polymicrobial Failure to grow organism from pus if not culture anaerobically. Failure to respond to usual antibiotics. Infection from animal bites. Detection of "Sulphur granules"' due to actinomycosis INFECTIONS BEGIN • DISRUPTION OF BARRIERS – TRAUMA – OPERATIONS – CANCEROUS INVASION OF TISSUES • DISRUPTION OF BLOOD SUPPLY – DROPS OXYGEN CONTENT OF TISSUE – DECREASE IN Eh POTENTIAL – TISSUE NECROSIS WHAT ARE THE INFECTION CAUSED BY THESE ANAEROBIC ORGANISMS I 1. 2. 3. 4. 5. 6. Post operative wound infection Brain abscess Dental abscesses Lung abscess Intra abdominal abscess, appendicitis, diverculitis All these infection can cause bacteriaemia WHAT ARE THE INFECTION CAUSED BY THESE ANAEROBIC ORGANISMS II 1. 2. 3. 4. 5. 6. Infection of the female genital tract Septic abortion Puerperal infection or sepsis Endometritis Pelvic abscess 12. Other infections – – – a) Breast abscess in puerperal sepsis b) Infection of diabetic patients (diabetic foot infections). c) Infection of pilonidal sinus LABORATORY DIAGNOSIS: • When anaerobic infection is suspected; – a) Specimens have to be collected from the site containing necrotic tissue. – b) Pus is better than swabs. – c) Specimens has to be send to the laboratory within 1/2 hour why? – d) Fluid media like cooked meat broth are the best culture media. – e) Specimens have to incubated anaerobically for 48 hours. TREATMENT: • Bacteroides fragilis is always resistant to penicillin. • But penicillin can he used for other anaerobes • Flagyl (metronidazole) is the drug of choice. • Clindamycin can also be used. ORAL & DENTAL • > 400 SPECIES OF ANO2 IN MOUTH • MOST INFECTIONS = POLYMICROBIC – MIXED ORGANISMS – ENTER AS A GROUP • ANO2 NOT INITIAL INVADER – USUALLY SECONDARY – 1ST ORGANISM DECREASES [O2] & Eh ORAL & DENTAL • COMMONLY ASSOCIATED WITH 1. 2. 3. 4. 5. DENTAL ABSCESSES ROOT CANALS JUVENILE PERIODONTITIS ADULT PERIODONTITIS CLENCHED FIST INJURIES ENT – HEAD & NECK 1. CHRONIC OTITIS MEDIA 2. CO-PATHOGENS WITH CHRONIC STREP TONSILLITIS 3. ACUTE SINUSITIS – POST-DENTAL EXTRACTIONS OR TRAUMA – 2o INVADER ENT – HEAD & NECK • VINCENT’S ANGINA – COMBINATION OF FUSOBACTERIUM & SPIROCHETE SPECIES OVERGROWTH – ANAEROBIC PHARYNGITIS – GRAY MEMBRANE – FOUL ODOR Vincent’s disease • Trench mouth • Sudden onset of pain in the gingiva (mastication) • Necrosis of the gingiva – interdental papilla – a marginated, punched-out, and eroded appearance • A superficial grayish pseudomembrane • altered taste sensation is present • Fever, malaise, and regional lymphadenopathy Ludwig’s Angina Lemierre Syndrome Expansion of the retropharyngeal soft tissues PLELRO PULMONARY I FECTION • • • • • ASPIRATION LUNG ABSCESS ASPIRATION PNEUMONIA M ETASTATIC LUNG ABSCESS BRONCHIACTSIS ALL OF ABOVE CAN CAUSE EMPYEMA LUNG & PLEURAL 1. 2. 3. 4. 5. ASPIRATION PNEUMONIA EMPHYSEMA LUNG ABSCESSES MALIGNANCIES LEUKOPENIA THORACIC ACTINOMYCOSIS THORACIC ACTINOMYCOSIS ACTINOMYCOSIS Molar tooth appearance of Actinomyces israeIii Macroscopic colony (left) Gram stain (right) of Actinomyces SKIN & SOFT TISSUE • TRAUMATIZED & DEVITALIZED TISSUE 1. TRAUMATIC WOUNDS 2. HUMAN/ANIMAL BITES 3. ISCHEMIA OF EXTREMITIES • DIABETES • ATHEROSCLEROSIS CLENCHED FIST INJURIES DIABETIC FOOT HUMAN BITE NECROTIZING CELLULITIS FEMALE UROGENITAL • • • • CHORIOAMNIOTIC INFECTIONS ENDOMETRITIS PID – ABDOMINAL INFECTIONS BACTERIAL VAGINOSIS WITH GARDNERELLA & BACTEROIDES SP. PUERPERAL INFECTION SEPTIC ABORTION • PUERPERAL ABSCESS • SEPTIC ABORTION • BACTERAEMIA • PELVIC ABSCESS • ADENXAL ABSCESS • PERITONITIS • ENDOMETRITIS ABDOMINAL INFECTIONS • MANIPULATION, INVASION OR TRAUMA TO GI TRACT 1. 2. 3. 4. TRAUMA SURGERY APPENDICITIS MALIGNANCIES • COLON CANCER CNS 1. HEAD TRAUMA 2. HEMATOGENOUS SPREAD – FROM ANY INFECTED BODY SITE 3. GEOGRAPHIC SPREAD – SINUS INFECTIONS – DENTAL ABSCESSES BONE & JOINT • • • • HEMATOGENOUS SPREAD TRAUMA PERIVASCULAR DISEASE JUVENILE PERIODONTITIS OTHER INFECTIONS • • • • GRAM NEGATIVE BACTREMIA BREAST ABSCESS AXILLARY ABSCESS INFECTION OF DIABETIS EG.DIABETIC ULCERS • INFECTION OF PILONIDAL SINUS • PARONYCHIA CLASSIFICATION 1. Anaerobic spore forming bacilli 2. 3. 4. 5. 6. (Clostridia) Gram negative bacilli nonsporing (Bacteroides) Anaerobic streptococci (Peptostreptococcus) Anaerobic staphylococcus (Peptococcus) Gram negative diplococci (Veillonella) Gram positive bacilli (Actinomyces) ORGANISM GROUPS • GRAM NEGATIVE RODS – BACTEROIDES – PREVOTELLA – PORPHYROMONAS – FUSOBACTERIUM – BUTYRIVIBRIO – SUCCINOMONAS Bacteroides fragilis BACTEROIDES • STRICT ANAEROBE • PLEOMORPHIC • GRAM NEGATIVE BACILLI (COCCO BACILLI) • NORMAL FLORA IN – OROPHARYNX – GASTROINTESTINAL TRACT – VAGINA BACTEROIDES FRAGILIS GP • GROUP = B. FRAGILIS, B. VULGARIS, B.THETAIOTAMICRON, B. UNIFORMIS – ACCOUNT FOR 1/3 OF ALL ISOLATES – RESISTANT TO 20% BILE – RESISTANT TO MANY ANTIBIOTICS • PENICILLIN, KANAMYCIN, VANCOMYCIN, COLISTIN – AND MANY MORE BACTEROIDES FRAGILIS GP • GLC = MAJOR ACETIC & SUCCINIC, LACTIC & PROPIONIC ACIDS • NO PIGMENTATION OF COLONIES OR FLUORESCENCE BACTEROIDES OTHER SP • BACTEROIDES SPECIES OTHER, NOT B. FRAGILIS GROUP – GLC = MAJOR ACETIC & SUCCINIC ONLY – BILE SENSITIVE – RESISTANT TO KANAMYCIN ONLY – SOME PIGMENTED BACTEROIDES • B. FRAGILIS IN THE GUT AND VAGINA • B.MELANINOGESUS AND B.ORALIS IN THE MOUTH AND OROPHARYNX • B. FRAGILIS PENICILLIN RESISTANT, • OTHER ARE SENSITIVE, • IT IS THE COMMONEST ORGANISM IN THE GUT 10 12 ORGANISM /GRAM OF FAECES Bacteroides and other anaerobic bacilli BACTEROIDES AND FUSOBCTERIUM B.FRAG B.NECROPH ORUS B.MELANINO B.CORRODE GENICUS NS FUSOBACTE RIUM BLACK PIG. - - + - - PITTING - - - + - INDOLE+ - - + - - LYSINE+ BILE GROWTH + + Growth of Bacteroides fragilis on Bacteroides bile-esculin agar Bacteroides fragilis • Special-potency kanamycin, vancomycin, and colistin antimicrobial agent disks to first quadrant of this plate. PORPHYROMONAS • GLC = ACETIC, SUCCINIC PLUS PROPIONIC, BUTYRIC, ISOBUTYRIC,& ISOVALERIC • BILE SENSITIVE • USUALLY BLACK PIGMENTED COLONIES – P. GINGIVALIS, P. ENDODONTITIS & P.ASACCHAROLYTICA PREVOTELLA • GLC = ACETIC, SUCCINIC, ISOVALERIC, NO BUTYRIC • BILE SENSITIVE • BLACK PIGMENT & FLUORESCENCE – Pr. INTERMEDIA – LIPASE + – Pr. MELANINOGENICA – BRICK RED FLUORESCENCE FUSOBACTERIUM • GLC = ACETIC, PROPIONIC, &BUTYRIC, NO SUCCINIC • ANTIBIOTICS – SENSITIVE TO KANAMYCIN – RESISTANT TO VANCOMYCIN – COLISTIN VARIABLE Fusobacterium nucleatum FUSOBACTERIUM • F. NUCLEATUM = LIPASE Ø • F. NECROPHORUM = LIPASE + • F. NUCLEATUM >> F. NECROPHORUM ISOLATES • COMMON IN ASPIRATION PNEUMONIAS MISCELLANEOUS GNB • BUTYRIVIBRIO – CURVED GNB – GLC = MAJOR BUTYRIC • SUCCINOMONAS – CURVED GNB – GLC = ACETIC & SUCCINIC PEPTOCOCCUS NIGER • GRAM POSITIVE COCCI • GLC = ACETIC, BUTYRIC, ISOBUTYRIC, ISOVALERIC, CAPROIC • BLACK PIGMENT PEPTOSTREPTOCOCCUS • • • • GRAM POSITIVE COCCI GLC = ACETIC, SOME BUTYRIC Ps. ASACCHAROLYTICUS INDOLE + Ps. ANAEROBIUS, Ps. MAGNUS, Ps.PREVOTI, Ps. INDOLECUS STREP & STAPH • ANAEROBIC SPECIES OF STAPH AND STREP • STREPTOCOCCUS INTERMEDIUS • STAPHYLOCOCCUS SACCHAROLYTICUS VEILLONELLA PARVULA • • • • • GRAM NEGATIVE COCCI GLC = ACETIC & PROPIONIC NITRATE + HEAD AND NECK INFECTIONS DENTAL ABSCESSES CLOSTRIDIUM SPECIES • LARGE GRAM POSITIVE RODS • SPORE FORMATION • SPECIFIC DISEASES – PSEUDOMEMBRANOUS COLITIS – TETANUS – BOTULISM – GANGRENE - MYONECROSIS C. difficile CLOSTRIDIA CLOSTRIDIA • Causative Agents For – 1.Gas gangrene : Cl. perfringens and other e.g septicum – 2.Tetanus : Cl. tetani – 3.Botulism : Cl. botulinum – 4.Toxic enterocolitis : Cl. difficile (Pseudomembernous colitis) Clostridium perfringens (CI . welchii) • • • • Morphology large rods gram +ve With bulging endospores Not motile Capsulated Clostridium perfringens C. perfringens C. perfringens Culture: • A) Blood agar with haemolytic colonies (double zone of haemolysis • B) Cooked meat medium • Gives the NAGLAR'S Reaction & toxin neutralization on Egg yolk medium & toxin is a phospholipase C. perfringens NAGLAR'S Reaction Lipase and/or lecithinase (EYA), Diseases Caused by C. perfringens • • • • • 1) Wound Contamination 2) Wound infection 3) Gas Gangrene - most important disease 4) Gas Gangrene of the uterus in criminal abortion 5) Food Poisoning • Spores are swallowed Germinate in gut after 18 hours • Toxin • abdominal pain and diarrhoea GAS GANGRENE • Causes mainly – – – – (Cl perfringens) (Cl. welchil) CI. novyl, CI. Septicum CI oedemaritians – – – – Traumatic open wounds Compound fractures Muscle damages Contamination with dirt etc, • Pathogenesis: • Mainly in war wounds, • Old age, – Low blood supply • Amputation of thigh – Prophylaxis with penicillin NECROTIZING FASCIATITIS NECROTIZING FASCIATITIS MYOSITIS Gram Stain of vaginal aspirate 1. Clostridiae necrotizing (myonecrosis) Prevention and Treatment • • • • • Remove dead tissue Remove debris Foreign bodies Penicillin Hyperbaric oxygen TETANUS Cl.tetani • Causative organism Cl.tetani • Morphology gram +ve anaerobic with terminal spore • • • Drum Stick appearance Lives in soil and animal feaces. e,g horse Any wound can infected if contaminated by spores Face & neck wounds are more dangerous why ? C. tetani Clinical Features • Incubation period 1-2 weeks • Symptoms: Painful muscle spasm around infected wound • Contraction of muscles of face= – Trismus (Lockjaw) – Risus Sardonicus strychnine • Back – Araching of Back Opisthotonus • opistho meaning • • "behind" and tonos meaning "tension", Extrapyramidal effect and is caused by spasm of the axial along the spinal column . Caused by – Tetanus. – Cerebral palsy – Traumatic brain injury Pathogenesis • 1 ) Tetanospasmin most important powerful • • • • exotoxin 2) Totanolysin No invasion or Bacteraernia Toxin is a protein It inhibits transmission of normal inhibitory messages from central nervous system at anterior horn cells of cord Pathogenesis Diagnosis • Mainly by clinical • Laboratory not important • Lab – Organism strict anaerobe – Very motile , spread on agar. C. tetani Prevention • • • • Toxoid vaccine: Vaccination D P T 2 , 4 , 6 , 18 months & 5 Year Booster every 10 years Treatment . • • • • Cleaning of wound Removal of Foreign body Specific by antitoxin – Horse serum can caused anaphylaxis & shock must be tested first – Human immunoglobulin – Antibiotics . Penicillin Supportive treatment – 2. Dark pace, fluids – 3. Sedative valium CLOSTRIDIUM BOTULINUIM Habitat • Soil,Ponds AND Lakes Toxin • Exotoxin • Protein • Heat labile at 100 OC – The most powerful toxin known Lethal dose 1 µg human • 3 kg kill all population of the world • Dictated for by lysogenic phage • Resist gastrointestinal enzymes Botulism • • • • From canned food., sea food e_g. salmon Not well cooked Spores resist heat at 100 oC then multiply and produce toxin ENFANTILE BOTULISM • Ingestion of Spores germination in the • • • • gutBotulism Week child Cranial nerve Constipation Other Botulism Pathogenesis • • • • • Ingested - incubation period 12-36 hour 7 Types Mainly types A, B, E, F Attacks neuromuscular junctions Prevents release of acetylcholine Symptoms • Funny eye movement as if cranial nerve affected when bulbar area of the brain affected • Respiratory and circulatory collapse SPECIMENS • Suspected food • From the patient – Faeces – Serum growth • Toxin detection by mouse – incubation paralysis and death INFANTILE BOTULISM • • • • Week lethargic child Constipation Respiratory and cardiac arrest Due to colonization of intestine by CI. botulinum • Diagnosis by -Culture of stools • Detection of toxin in feaces • Treatment • 1) Supportive • 2) Horse antitoxin • Prevention • 1) Adequate pressure • cooking autoclaving 2) Heating of food for 10 minutes at 100 OC Botox C. DIFFICILE • PSEUDOMEMBRANOUS COLITIS – 90% OF CASES CAUSED BY C. DIFF – LONG TERM TREATMENT WITH BROAD SPECTRUM ANTIBIOTICS OR CHEMO • NOSOCOMIAL DISEASE • KNOCK DOWN NORMAL FLORA • CLINDAMYCIN, AMPICILLIN, CEPHALOSPORINS • CHEMOTHERAPEUTIC AGENTS C. DIFFICILE • OVERGROWTH OF C. DIFFICILE – TOXIN THEN PRODUCED • A -FRAGMENT = ENTEROTOXIN • B -FRAGMENT = CYTOLYTIC TOXIN • PSEUDOMEMBRANE SIMILAR TO THAT OF C. DIPHTHERIAE – BACTERIA, FIBRIN, WBC, DEAD – TISSUE CELLS - TOUGH C. DIFFICILE • DIARRHEA FIRST – ELECTROLYTE & FLUID LOSS – LEADS TO DEHYDRATION • INTESTINAL BLOCKAGE – CONTENTS BLOCKED – COLON BULGES • PERFORATION, RUPTURE SEPSIS Clinical pictures C. DIFFICILE • RAPID AGGRESSIVE COURSE IN YOUNG CHILDREN • DIFFICULT TO SELECTIVELY • CULTURE – 5-10% CULTURE + EVEN WITH CONFIRMED DISEASE – TOO MANY NORMAL ANO2 PRESENT C. DIFFICILE • SPECIALIZED ISOLATION MEDIA – CCFA – CYCLOSERINE , CEFOXITIN,FRUCTOSE, EGG YOLK AGAR – CCMA – CCFA BUT MANNITOL FOR FRUCTOSE – CDMN – CYSTEINE HYDROCHLORIDE, MOXALACTAM, NORFLOXACIN AGAR C. difficile C. difficile C. DIFFICILE • C. DIFFICILE IS NORMAL FLORA – ISOLATION NOT ENOUGH • NEED TOXIN ASSAY TO CONFIRM • CELL-FREE STOOL EXTRACT – LATEX AGGLUTINATION SCREEN • SOME CROSS-REACTIVITY – EIA TO CONFIRM Major Clostridial Diseases