Confidentiality of Testing and
Treatment of Adolescents with HIV:
A Legal Guide for Clinicians
AETC Adolescent HIV/AIDS Workgroup
This presentation was developed by the Adolescent
HIV/AIDS Workgroup, and its Legal Rights and
Entitlements Subgroup, in collaboration with the AIDS
Education and Training Centers National Resource
Center (AETC NRC).
It was updated in October 2010 by David Korman, JD
from Pennsylvania/MidAtlantic AETC.
Subgroup Members
David Korman, JD — Subgroup Leader
(Pennsylvania/MidAtlantic AETC)
Vera Holmes, LCSW (FXB Center)
Cathy Samples, MD, MPH (New England
AETC)
Subgroup Members from AETC NRC
Megan Vanneman, MPH – Subgroup
Coordinator
Supriya Modey, MPH, MBBS
General consensus
Many adolescents will not seek medical care
unless they are assured of confidential
services.
Support for minors’ rights
Legislation promoted in all states providing
confidential medical care for minors with respect to
reproductive, sexually transmitted infections (STIs)
and HIV/AIDS-related issues by:
-American Academy of Family Physicians
-American Academy of Pediatrics
-Society of Adolescent Medicine
-American College of Obstetricians and Gynecologists
Laws vary from state to state
Laws pertaining to
confidential medical
treatment of minors vary
tremendously state to
state.
HIV testing and treatment
often not specifically
addressed.
General medical rule:
minors are without legal capacity
In general, minors* lack legal capacity to make
medical decisions.
Involvement of parent/guardian often required.
* (generally persons under the age of 18 years)
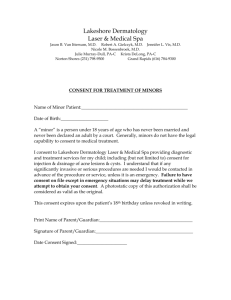
Typical statute
Any person who is eighteen years of age or
older, or has graduated from high school, or
has married, or has been pregnant, may
give effective consent to medical, dental and
health services for himself or herself, and
the consent of no other person shall be
necessary.
(Pennsylvania, 35 P.S. Sec. 10101)
Law provides for exceptions
“Non-confidentiality disincentive”= minors may not
want to ask for treatment for sensitive matters if
believe service not confidential.
Due to “non-confidentiality disincentive,” some
exceptions to general rule of non-capacity of
minors.
Situations where minors might have
capacity:
Sexually transmitted
infections
Substance abuse
Reproductive or
contraceptive services
Mental health
interventions
Married
HIV may be specifically addressed
Some states— minors’
rights to confidential HIV
testing and/or treatment
specifically provided
statutorily.
Others— unclear.
Different requirements in different
states
Some states (with specific HIV-related
statutes) designate age at which
parental/guardian consent not needed (as
low as 12 years; as high as 16).
Some states— depends upon clinical
judgment of provider (assess minor’s
maturity and ability to make rational
choices).
Caveat
Especially in those states that follow “The
Mature Minor Rule,” it is important for the
clinician to document carefully:
Minor’s maturity
Reasons for non-disclosure to parent
Minor’s understanding of situation
Minor’s consent
Caution: some states provide for
mandatory disclosure of positive test
Some states— minor may have right to HIV
testing without parent/guardian consent, but
positive test result must be disclosed to
minor’s parent/guardian.
Dilemma
Informing minor of obligation to disclose
positive test result to minor’s
parents/guardians might dissuade testing.
Failure to inform minor of limit to
confidentiality of test results is
unlawful/unethical.
Testing vs. treatment
Most states that provide
confidential testing of
minors do not address
issue of confidential
treatment of minor who
does not want his/her HIV
status or treatment
disclosed to
parent/guardian.
Interpretation of other laws dealing
with minors’ capacity to make medical
decisions
Interpretation of other statutes pertaining to minors’
care (usually pertaining to STIs or substance
abuse) crucial in states without specific HIV statute
that addresses minors.
* Note: some states do not treat HIV as an STI.
Minor’s consent to treatment statutes
Many states— subscribe to “Minor’s
Consent to Medical Treatment Acts.”
Acts typically provide circumstances under
which minor may be tested or treated
without parent/guardian consent.
Typical statute with expressed exceptions
Pennsylvania’s statute (fairly representative)
Any minor may give effective consent for
medical and health services to determine the
presence of or to treat pregnancy, and venereal
disease and other diseases reportable under the
act of April 23, 1956 (P.L. 1510), known as the
"Disease Prevention and Control Law of 1955," and
the consent of no other person shall be
necessary.
How to proceed?
Law of your forum
Is there a statute that
deals specifically with
minors and HIV?
Yes…
No…
You are
lucky, but
read
carefully …
Does this
situation fall
within one of
the
commonly
related
issues (like
STIs)?
Are the “exceptional” conditions met?
Is the patient old enough?
Is this a covered situation?
STI
Substance abuse
Reportable communicable disease
Emancipation
Regardless of age or “exception” …
determine if minor has capacity
Generally, minor has capacity if can:
1. Understand the situation.
2. Explain reasons for decisions or actions.
3. Describe risks and benefits of decision or
action.
If legal capacity is absent …
Determine who has authority for minor.
Usual default is parents (or custodial parent if only one
parent available).
Is there a reason for parent(s) not to be involved (e.g.,
abuse, incest, neglect, absence)?
Is a non-parental guardian already established?
Listen to the adolescent
Usually helpful for young person to talk with
parent or supportive adult regarding health
care decisions.
Why is this minor hesitant?
(Note: the reason given may precipitate
mandatory reporting under state law of
abuse, etc.)
Mandatory reporting
Almost every state requires reporting sexual
and physical abuse of minors.
Reporting abuse does not necessarily entail
disclosure of HIV status.
Take measures to mitigate risk of
disclosing HIV-related information.
Resources
Social Services— health care institutions
and government
Legal department (e.g., appointment of a
non-parental guardian for the child)
If adolescent appears to have capacity …
Just for HIV testing? (e.g., but not treatment)
To whom does the test result have to be reported?
Minor should be advised of reporting requirements
before testing.
Minor should be advised if legal capacity applies
only to testing and not treatment.
Reporting for epidemiology
All states require reporting newly discovered HIV
infection—confidentially or anonymously (using
unique identifiers)–whether the patient is minor or
adult.
Collection of that information is for epidemiology
only, not for law enforcement.
Important that patient understands this limited
disclosure.
Institutional caveats to inadvertent disclosure
Who pays for testing and/or treatment?
Will reimbursement through insurer lead to disclosure?
Will mailings to patient be a risk for disclosure? (e.g.,
insurance company’s Explanation of Benefits)
Will phone calls to patient’s residence be a risk for
disclosure?
Maintaining confidentiality of minor in treatment
Many times more difficult than just testing.
Almost always requires social service intervention
(e.g., housing often a problem).
Case Study 1
14-year-old female presents with history of
consensual unprotected vaginal sexual intercourse.
She wants to be tested for HIV. She indicates that
her primary sexual partner is 22-years-old.
She does not want her parents, with whom she
lives, to know about testing or her partner.
Issues
Can she be tested without parental notice or
consent?
If she tests HIV-positive, who must be
informed? What do we do next?
Whom, if anyone, must be advised of her
activity with the partner?
Reflections: can she be tested without
parental notice or consent?
Do my state’s laws:
Provide for testing without parental knowledge or
consent?
Indicate appropriate age for sexual intercourse?
Have an STI or reportable disease exception?
Reflections: If she tests HIV-positive, who
must be informed? What do we do next?
Almost certainly, HIV positive tests must be
reported by name (but held in confidence) or
unique identifier.
What does state law provide for
contact/partner notification?
How do we handle treatment for her?
Notice to minor’s parents
State law might require notification of
positive test result to parents/guardians
even without minor’s consent.
Some states mandate parent notification,
others permit parent notification, and others
forbid it without the minor’s consent.
Reflections: Whom, if anyone, must be
advised of her activity with the partner?
Is this a reportable incident?
Is this “statutory rape” or “sexual assault” even
though “consensual” because she is:
(a) Under age of consent under state law?
(b) Her partner is much older than she?
If reportable— to whom?
Law enforcement?
Child/Youth Services?
Parents?
If reportable— just the activity, or the HIV status as
well?
Caution
The requirements of health care workers for
reporting “sexual assaults,” “statutory rape,”
“aiding in the delinquency of a minor,”
“domestic violence,” “child abuse/neglect,”
and the like vary tremendously from state to
state.
Caution: states differ
In what they designate as a “reportable incident.”
In who they require to report (e.g., physician,
administrator, nurse).
In whom must be notified (e.g., law enforcement,
child protective services, parents).
In what must be reported (e.g., name of minor,
name of alleged perpetrator, alleged acts).
Variation
How would your responses differ …
If the minor were homeless?
If the minor were pregnant and in prenatal
care?
Case Study 2
14-year-old child in foster care.
Disclosed history of injection drug use.
Brought to clinic by county case worker.
Issues
Can the minor be tested?
What if the minor does not wish to tested?
Who obtains the results?
Reflections
Who has medical authority for child?
Case worker? Foster parents? Biological
parents?
Can 14-year-old minor be tested
involuntarily?
*May depend on importance of testing,
clinical picture, and/or invasiveness of test.
Reflections
Results may not automatically go to case worker,
foster parents or to child services agency.
In some states, case worker or foster parents only
obtain test results if:
(a) they generally are authorized to obtain
medical information for child;
(b) they are in charge of child’s health; and
(c) they need to know.
Bottom lines:
We must attempt to mitigate the
disincentives to minors seeking testing.
Minor’s fear of disclosure to parents or
others is significant disincentive.
“Instinctive” public policy in favor of
parental notification and involvement often
at odds with points 1 and 2.
Bottom lines (continued):
Probably disproportionate number of minors
at risk for HIV infection, are not desirous of
parental notification (compared to other
potential medical conditions).
Involvement of supportive services is often
advisable to assist in issues of abuse,
housing, guardianship, etc.
Caveat
Confidential testing of at-risk minors has typically
been practice, even in absence of explicit and
unambiguous legal authority.
Public health organizations’ support of such testing
(and treatment) may be increasingly under attack
and vulnerable to judicial limitations (e.g., the
changing judicial standards regarding
reproductive/sexual privacy in several states).
Caveat
These issues are legally and ethically complicated.
Document the patient’s understanding, consent,
and concerns.
Legal answers vary tremendously from state to
state.
Resources
Do not hesitate to utilize resources:
Lawyers
Ethicists
Social Service Workers
Adolescent Health Care Experts (Society for
Adolescent Medicine)
State HIV/AIDS/STI Bureau
Recognize there is no perfect answer,
but work for the least harmful solution
Not incumbent upon you to finish the task, but
neither are you free to absolve yourself from it.