Vestibular Rehabilitation: Evaluation and Treatment Strategies for
advertisement

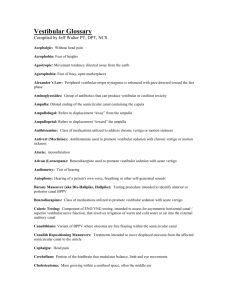
Vestibular Rehabilitation: Evaluation and Treatment Strategies for Common Vestibular Disorders Burt DeWeese, PT, MCMT Rebound Physical Therapy Vestibular Rehab Specialist burt@reboundphysicaltherapy.com Background • Graduate of Kansas State University, 1999 • Master’s in Physical Therapy from Mayo School of Health Sciences, Rochester, MN, 2002 • Completed APTA Competency Based Certification Course: Vestibular Rehabilitation-Emory University, 2004 • Working toward manual therapy certification through NAIOMT – will complete level III this year • Clinical Director at Rebound Physical Therapy, Topeka, KS Objectives • Describe the anatomy and physiology of the vestibular system. • Describe the pathophysiology of common vestibular disorders. • Complete and interview and examination of a person with vestibular dysfunction. • Identify appropriate standardized assessment tools for use in vestibular rehabilitation. • Demonstrate skill in performing the occulomotor exam. • Demonstrate skill in differentiating between types of BPPV. • Identify appropriate treatment intervention with patients with vestibular disorders. Anatomy and Physiology Anatomy of the Ear Anatomy of the Ear • The External Ear • External auditory canal • Ends at the tympanic membrane • The Middle Ear • Space between the tympanic membrane and the inner ear • Contains the malleus, incus and stapes • Transmits sound into waves inside the cochlea • Filled with air Anatomy of the Ear • The Inner Ear • Contains sensory organs for hearing and balance • Bony labyrinth within the temporal bone • Central portion is names the vestibule • Saccule and Utricle • Cochlea is anterior and vestibular portion post • Tissue layers: bony labyrinth, perilymph, membranous labyrinth, endolymph The Labyrinth • Bony Labyrinth • Perilymph • Between bony and membranous labyrinth • Membranous labyrinth • Endolymph • Inside membranous labyrinth Parnes, 2003 The Labyrinth • 3 Semicircular Canals • Anterior, Posterior Horizontal • Cochlea • Hearing component • Vestibule • Saccule and Utricle The Hair Cell • Found in cochlea, semicircular canals, saccule and utricle • Send in information to the vestibularcochlear system • “Hair” of the hair cell consists of: • Sterocilia (40-70 in one hair cell) • Kinocilium (1 per hair cell) Semicircular Canals • Hair Cells • Motion Sensors • Always sending info to the brain • Kilocilia • Deflection Towards- Excites • Deflection Away- Inhibits Semicircular Canals • Provides input about angular head velocity • Three canals on each side • Anterior (superior), Posterior (inferior) & Horizontal (lateral) • 90 degree angle from each other • Horizontal canal • 30 degree elevation Semicircular Canals • Mate on the opposite side • L ant/R post, R ant/L post • Each semicircular canal has a ampulla housing the sensor organs • Hair cells covered by the cupula • Both ends terminate in the utricle The Otoliths • Utricle (Linear) • Horizontal Movements • Head Tilt • Saccule (Linear) • Up & Down Movements • Otoconia “Ear Rocks” (Calcium Carbonate Crystals) • Hair Cells Herdman, 2000 Vestibular Occular Reflex • Allows clear vision through gaze stabilization • Coordinates eye and head movements • Sensory stimulation sends info to the brainstem region that controls eye movement • Example: Head left, eyes turn right while focusing on an object • R lat rectus/L med rectus excited and opposite inhibited Causes of Vertigo Herdman, 2000 Causes of Vertigo • BPPV • Vestibular Neuritis • Labyrinthitis • Meniere's Disease • Bilateral Vestibular Loss • Cervicogenic Dizziness Common Disorders Semi-Circular Canals Inflammation of the Vestibular Nerve • Vestibular Neuritis • Symptoms • • • • Sudden onset of vertigo Nausea/vomiting Imbalance Sensitivity to motion Inner Ear • Last hours to days • Can result in chronic dysequilibrium • Caused by viral infection • Treatment Cochlea Common Disorders • Vestibular Labyrinthitis • Viral or bacterial infection of the membranous labyrinth • Acute onset of hearing loss, vertigo, nausea/vomiting • Can last 1-4 days • Will demonstrate imbalance and sensitivity to head movements Common Disorders • Meniere’s Disease • Increased endolymph pressures • Episodic • Low frequency hearing loss • Tinnitus • Can last hours to days Common Disorders • Fear of Falling • Disuse Dysequilibrium • Orthostatic Hypotension • Cervicogenic Dizziness • Anxiety Common Disorders • Central • TBI • CVA • Multiple Sclerosis Vestibular Evaluation • Subjective component • Thorough History • Dizziness Handicap Inventory • ABC confidence scale Common Questions • • • • • • • • • • • Tell me about your symptoms. When did your symptoms begin? How long did/does your symptoms last? Are your current symptoms better, worse or the same? Can you rate the severity of your symptoms 0-10/10? Do your symptoms increase with positional changes or certain movements? Do you have difficulty with keeping objects in focus? Do you have ear fullness, pressure, ringing or hearing loss? Do you have a history of these symptoms? Have you had any falls or unsteadiness? Currently what meds are you taking? Dizziness Handicap Inventory Vestibular Evaluation • Bedside Exam • Occulomotor • • Smooth Pursuit Saccades VOR VOR cancellation Head Thrust/Head Shake Upper and lower extremity screen Cervical screen-may choose to do first Vestibular Evaluation • Other testing options • Videonystagmogtaphy (VNG) • Caloric Testing Test horizontal semicircular canals only External auditory canal is irrigated with warm and cold water with head in 30 degrees flex Significant finding 25% or more reduction indicates a unilateral weakness Observation Tools • Frenzel Goggles • Video Frenzel Lenses • Room Light Vestibular Evaluation • Functional Testing • • • • Dynamic Gait Index-videos Berg Balance Scale Timed Up and Go Static Balance Testing Eyes Open/Eyes Closed Head turns Firm and Foam Dynamic Gait Index Dynamic Gait Index • Video Berg Balance Scale Timed Up and Go • Video Timed Up and Go (secs) (7,12,14) Back against chair, arms on armrests –get up and walk at comfortable place to line 3 meters away, return to chair and sit down; repeat, take average Age (years) 60-69 70-79 80-89 Male 8 9 10 Female 8 9 10 Time < 10 seconds is normal 11-20 seconds is normal for frail elderly >14 seconds indicates risk for falls >20 seconds indicates impaired functional mobility >30 seconds indicates dependency in most ADL and mobility skills Static Balance Testing • Modified CTSIB • Ground-Eyes open and closed • Foam-Eyes open and closed • ½ Tandem and Tandem • SLS • Computerized Dynamic Posturography Computerized Posturogrphy Benign Paroxysmal Positional Vertigo BPPV Statistics • BPPV is the most common cause of vertigo in patients with vestibular disorders (Bath et al, 2000) • About 20% of all dizziness is due to BPPV (Hain, 2010) • About 50% of all dizziness in older people is due to BPPV (Hain, 2010) BPPV Defined • Benign- It does not signify anything lifethreatening. Not malignant. • Paroxysmal- Refers to the fact that the episodes are brief and self-limited – "paroxysm" means "attack." • Positional-Change in position provokes symptoms. • Vertigo-Room spinning sensation. Causes of BPPV •“Idiopathic”-50%-70% •Head injury- 7%-17% •Viruses •Vestibular neuritis- 15% •Degeneration? BPPV • Nystagmus • Non-voluntary oscillation of the eye • Defined fast and slow phases in opposite direction • Fast phase defines direction of nystagmus • Semicircular canals connected to specific eye muscles, which dictates direction of nystagmus • Video BPPV – Nystagmus • Posterior canal • Up-beating, torsional nystagmus toward involved ear • http://youtu.be/siL3MTNUIQI • Anterior canal • Down-beating, torsional nystagmus toward involved ear • Horizontal canal • Lateral, slight torsional nystagmus, greater toward involved ear • http://youtu.be/MtmkD5rDU0o Occurrence Rates • Percentages • Posterior canal- 92% occurrence • Horizontal canal- 6% occurrence • Anterior canal- 2% occurrence • Once patient has had BPPV, re-occurrence rate is about 25-30% BPPV • Classic Symptoms • Room spinning, nausea, imbalance • Brief episodes of vertigo with changes in head position relative to gravity • Lying down in bed Sitting up from lying down Rolling over in bed Bending over Looking up- Top Shelf Syndrome Challenges • Musculoskeletal restrictions • Pain cervical, lumbar, shoulder and hips • Fear of falling off table in sidelying when spinning • Hip replacements • Use of table/plinth Use of Plinth BPPV – Clinical Exam • Dix-Hallpike Test • 45 degree cervical rotation • Align canals with gravity • Sit to supine with 20 deg of cervical extension • Look for nystagmus and symptoms of vertigo • Practice Herdman, 2000 BPPV – Clinical Exam • Typical Nystagmus • Latency- before nystagmus starts 1-30 seconds • Direction Mixed up-beating, torsional nystagmus (post.) • Duration Less than 1 minute • Fatigues with repeated testing BPPV – Clinical Exam • All you need to know… • Direction The direction of the elicited nystagmus will tell you which canal is involved • Duration Will tell you the type of BPPV BPPV – Clinical Exam • Two types of BPPV • Canalithiasis (A) • Cupulolithiasis (B) BPPV – Canalithiasis • Otoconia are freely moving in the canals • Fall to the lowest point in canal • Induces flow of endolymph • Deflection of cupula • Fatiguing Nystagmus • Last less than 1 min BPPV – Canalithiasis • Video Animation • http://youtu.be/IHfU2cA7eRo BPPV – Cupulolithiasis • Otoconia are adherent to the cupula of the semicircular canal • Increased density of cupula • Sensitive to gravity • Persistent-last greater than 1 min Hain, 2010 Repositioning Procedures Parnes, 2003 Patient Response • Sensation of spinning • May feel like they will fall of the table • Clammy • Sweating • Nauseous • Vomitus Canal Alignment Reminder • Will treat R post. canal and L ant. canal the same way • Opposite eye movement • Post-Up beat/Rot • Ant-Down/Rot BPPV Treatment – Posterior/Anterior Canals • Canalith Repositioning Technique • Starting Position is Dix-Hallpike • Nystagmus should be same direction in all positions • Practice Liberatory or Semont Maneuver • Used for Cuplulolithiasis • Posterior and Anterior Canal • Rotate head 45 degrees away from affected side • Quick movements to jar otoconia loose Parnes, 2003 Case Study • 74 yo female with past medical history of BPPV • Slipped and fell at home • Hit her head on the floor • Admitted to hospital for 2 days • Patient self report of BPPV • Dizziness with getting in bed and rolling to the left • Patient positive for Left Posterior Canal BPPV • Treatment-Left CRT Case Study • 68 yo male with sudden onset of dizziness • Increased with rolling over in bed and looking up • Mild imbalance in Romberg eyes closed position • Positive R Dix-Hallpike with persistent upbeating and R torsional nystagmus Case Study • All other evaluation info was negative • Treatment • Semont Maneuver performed • Then performed CRT for post canal BPPV, once otoconia are dislodged from cupula • Symptoms were resolved after one visit Horizontal Canal BPPV • How do you test? Roll Test • Head in 30 degrees flexion • Rotate head either direction • Nystagmus will be lateral • Treat the side with greater symptoms Herdman, 2003 Horizontal Canal BPPV • Canalithiasis • Eyes will beat geotropic • Cupulolithiasis • Eyes will beat ageotropic Parnes, 2003 Horizontal Canal BPPV • Horizontal Canal CRT • Barbeque Roll • Head rotated to involved side first • Roll away from involved side • Keep head in 30 degrees flexion Herdman, 2000 BPPV – Flow Chart Horizontal Canal BPPV • HC- Semont maneuver • Used for Cuplulolithiasis • Horizontal Canal • Head in neutral position • Quick movements to jar otoconia loose • Then perform CRT BPPV Treatment • Post-Treatment Instructions- typically 24 hours • • • • Avoid lying down until you go to bed. Avoid up and down head movements. Prop head up at night with pillows. Avoid sleeping on affected side. • Debate Other Treatment Options • Brandt-Daroff • Home CRT • Balance retraining • Surgery-canal plugging Brandt-Daroff Exercises • 3-5 cycles • 3 times per day • Hold position for 30 seconds after vertigo stops Parnes, 2003 Home CRT • Same as CRT • Place pillow under shoulders • Tip head over pillow and rest on mattress Balance Re-training • Progress toward balance activities if the patient continues to have imbalance. • Will discuss balance activities in the Vestibular Rehabilitation section. Vestibular Rehabilitation Output of CNS • Vestibulo-Ocular Reflex (VOR) • Allows clear vision while the head is in motion. • Vestibulo-Spinal Reflex (VSR) • Generates compensatory body movement in order to maintain head and postural stability. • Prevents Falls Vestibular Function Testing • Video Infrared Recording • Eye Movements and Head Shake • BPPV • Caloric Testing • Head and Eye Movements • Saccades, Smooth, Pursuit, Head Thrust, Slow VOR Vestibular Testing • Computerized Dynamic Posturography • Dynamic Visual Acuity • Dynamic Gait Index • Static Balance Testing • Romberg, Sharpened Romberg, SLS • Timed Up and Go Treatment Theory Treatment Theory for Dysfunctions • Compensation • Response to permanent vestibular lesion. • Goals- approximate normal gaze stability and postural control. • CNS changes to optimize function. • Visual input important. • Mechanism for Compensation- Habituation Treatment Theory • Habituation • Long-term reduction of a response to a noxious stimulus. • Repeated movements of provocative stimulus. • Patients who move more, improve more. • Need to provoke symptoms to reduce symptoms. • Examples (MSQ) Treatment Theory • Adaptation • Long term changes in neuronal responses. • Goals Decrease retinal slip- gaze stabilization. Improve postural stability. Decrease symptoms. Decrease sensitivity. Increase balance and function. Treatment Exercises • Based on Models of VOR • Retinal Slip and Head Movements • Main Exercises • x1 and x2 Viewing Exercises Viewing Exercises Treatment Exercises • Guidelines • • • • • Target Seen Clearly Head Movement +/- 30 degrees Smooth Continuous Pushes Upper Limit Treatment Exercises • Progression • • • • • • • Duration: 1-2 minutes Frequency: 3-5x/day Target Size: Small Position of Head: Level, Slightly Down Position of Patient: Sit, Stand Target Distance: Near, Far Compliant vs. Non-Compliant Surface Treatment Exercises • Active Head Movements b/t 2 Targets • Remembered Target • Walking Fwd/Bwd with Head Turns • Bean Bag Toss (1 & 2) • 180 & 360 Degree Turns • Ball Against Wall • Walk in Circle with Ball Toss Treatment Exercises • Sit to Stand with head turns • Wobble board with head turns • Hurdles with ball toss • Obstacle course • Stairs Balance Re-training • Romberg • ½ Romberg • Full Romberg • On ground and on foam • Add head turns Home Exercise Program • All the previous discussed exercises • Can modify as needed • Can create any exercise incorporating head and eye movements • Include balance activities. Billing • PT evaluation- 97001 • Neuromuscular Re-ed-97112 • Canalith Repositioning-95992 • One unit per day • Therapeutic Activity-97530 Treatment Frequency • 1-3 times per week • Can take up to 8-12 weeks • Most often 4 weeks length of treatment • BPPV only: 1-3 visits • If BPPV and neuritis • Treat BPPV first, once resolved, treat neuritis and balance disorders Any Questions? Bibliography • Herdman, Susan. Vestibular Rehabilitation. Philadelphia: F.A. Davis Company, 2000. • Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ 2003; 169:7 681-693. • http://www.dizziness-andbalance.com/disorders/bppv/bppv.html. Timothy Hain, MD. Benign Paroxysmal Positional Vertigo. July 19, 2010. • Vestibular Rehabilitation: A Competency Based Course. Emory University. Atlanta, Georgia. Thank You!