375-730-1-ED - Iranian Journal of Allergy, Asthma and

Effect of Immunotherapy with Chimeric Protein Der f 1A and Der f
1B from Dermatophagoides farinae on Asthmatic Mouse Models
ABSTRACT
To investigate the effect of immunotherapy with chimeric protein Der f 1A and Der f
1B derived from Dermatophagoides farinae ( D. farinae ) mice with asthma, fifty mice were randomized into group A (negative control), B (asthma group), C
(immunotherapy group with Der f 1), D (immunotherapy with recombinant Der f 1A) and E (immunotherapy with recombinant Der f 1B). Mice in the group B, C, D and E were sensitized by intraperitoneal injection of the D. farinae extract in the first, seventh and fourteenth day, respectively, and challenged with atomized inhalation of the extract from day 21 for consecutive 7 days. Specific immunotherapy was performed in group C, D and E with Derf 1, Der f 1A and Der f 1B, respectively, 30 min before inhalation. The negative controls were treated with intraperitoneal injection and inhalation of the phosphate buffer solution (PBS). After inhalation challenge,all mice were subjected to total counting of the leukocytes in the bronchoalveolar lavage fluid (BALF) and examination of the pathological sections of lung tissues as well as determination of the IL-5 and IFN-γ level in the BALF and spleen cell culture supernatants (SSCS) and serum specific IgE and IgG2a levels.
As compared with the asthma group, significantly alleviated inflammation of the lung, markedly reduced levels of IL-5 and IgE as well as notably increased levels of IFN-γ and IgG2a antibody were found in mice undergone immunotherapy (all P <0.01). In conclusion, the chimeric protein Der f 1A and Der f 1B derived from D. farinae could effectively relieve the symptom of asthma in the model mice, suggesting that our work may lay a foundation for specific immunotherapy of the allergic diseases with these recombinants.
Keywords: Dermatophagoides farinae ; T-cell epitope; B-cell epitope; Recombinant allergen; Immunotherapy
INTRODUCTION
Allergic asthma is defined as chronic airway condition, characterized by infiltration of the lung lymphocytes and eosinophils leading to mucus secretion and airway hyperresponsiveness
1
, and appears worldwide prevalent year by year.
2
In global scale, approximate 80% of the asthma is associated with mites, in which house dust mite is the most common inhalant allergens that causes asthma.
3, 4
Although more than 30 allergens from the house dust mites have been recognized so far, yet only the major allergens from group 1 Dermatophagoides farinae (Der f 1) are well studied.
5, 6
Previous studies found that asthma attack is commonly caused by the imbalance of the Th1∕Th2 cells 7-9
, leading to infiltration of the activated eosinophils into the
airways and airway hyperresponsiveness because of increased secretion of the IL-4,
IL-5 and IL-13 cytokines by Th2 cells differentiating from Th0, yet reduced IFN-γ and IL-2 secreted by Th1.
10, 11
Allergen-specific immunotherapy (SIT) is currently recognized as the only causal approaches to the treatment of allergy through regulation of the immune response of the body to the allergens.
12, 13
However, current use of the vaccines for
SIT purpose primarily depends on the recombining the epitopes through gene engineering, for the epitope vaccine can be safe non-toxic and stable.
14-16
In our previous work, we successfully obtained the recombinant Der f 1A and
Der f 1B by induction and purification of the two proteins via expression in plasmid pET-28a (+) - Der f 1A and pET-28a (+) - Der f 1B
17
, and tentatively applied the two chimeric proteins in murine models of asthma for specific immunotherapy.
MATERIALS AND METHODS
Experimental animals
Fifty female BALB/c mice, SPF grade, aged 6-8 weeks and weighed (20±2) g, were purchased from the Centre for Comparative Medicine, Yangzhou University
(License:SCXK SU 2007-0001).
Main reagents and experimental materials
Extracts of the house dust mite, and the purified chimeric protein Der f 1A
(synthesized by B1-T1-B2-T2-B3-T3-B4-T4-B5-T5-B6) and Der f 1B (synthesized by B1-B2-B3-B4-B5-B6-T1-T2-T3-T4-T5) were preservations of our laboratory.
Mouse IL-5, IFN-γ, IgE and IgG2a and ELLISA were purchased from R&D (U.S.A).
Trypan blue was obtained from Sangon Biotech (Shanghai, China), and Liu's haematocyte stain was a product of Basco Diagnostics Inc. (Zhuhai, China). The microplate reader (model Elx800) was purchased from BioTek Instruments, Inc.
(U.S.A).
Animal grouping
Fifty female BALB/c mice were equally randomized into five groups, namely: group A(negative controls treated with phosphate buffered saline, PBS), group
B(asthma models), group C(treated with simple Der f 1), group D( treated with recombinant Der f 1A) and group E group(treated with recombinant Der f 1B).
Development of the asthmatic mouse models
Mice in each group were sensitized by intraperitoneal use of the mite extract at day 1, 7 and 14, respectively. Group A were treated with PBS, and group B, C, D and
E groups were sensitized with 100μl liquid extract of dust mite allergens (containing
10μg dust mite allergen, 32mg Al(OH)
3
, dissolved in 100μl PBS , pH7.2). By the day
21, all mice were caged in a box to undergo aerosol inhalation of the extract, 30 min a day, for consecutive 7 days. Group A received PBS, and group B, C, D and E were given the extract in dose of 10μg / ml.
Allergen-specific immunotherapy of the asthmatic mice
Mice in group A and B group were treated with PBS by intraperitoneal injection and aerosol inhalation, whereas those in group C, D and E were subjected to specific immunotherapy via intraperitoneal administration of the Der f 1, Der f 1A and Der f
1B in dose of 100μg / ml, 30 min before inhalation, from day 21 to 27. Twenty four hours after the final treatment, all mice were sacrificed for following tests.
Bronchoalveolar lavage fluid (BALF)
Mice in each group were intraperitoneally anesthetized with 10% chloral hydrate in dose of 0.2ml-0.3ml, 24-hour after the final challenge for endotracheal intubation.
Pre-cooled sterile PBS was used to irrigate the bronchi by repeated 3 times by respective dose of 0.4 ml, 0.3 ml and 0.3 ml, to recover the BALF, and the recovery rate was ensured to be greater than 90%. Then the BALF was centrifuged for 10 min by 2000 × g at 4 °C. The supernatant was transferred into a micro-centrifuge tube and stored at -80 °C for following detection of the IL-5 and IFN-γ levels. PBS was used to resuspend the cell sedimentation, and then, the cell suspension was taken and applied to a smear that was stained with Liu’s solution for classification and total count.
Determination of the srum specific antibodies
Serum samples were taken from the eyeball of individual mouse in each group, and then centrifuged by 380×g at 4°C for 10 min. The sera were obtained and detected for the specific IgE and IgG2a levels with ELISA kit.
In vitro culturing of the spleen cell and its cytokine detection
After the blood was obtained, mice were sacrificed by cervical displacement, and soaked in 75% ethanol for 30 min. Spleens were isolated under sterile conditions to prepare spleen cell suspension 18 . Trypan blue staining was performed, and live cell count >98% was eligible for subsequent experiment. Then the spleen cell suspension was adjusted to a cell density of 5 × 10
6
/ ml, and applied to the 96-well plate by 1 mL for each well, in which corresponding 10 µg antigen was added, and incubated in CO
2 incubator (37°C, 5% CO
2
) for 72 h. Then the supernatant was taken for measurement of the IL-5 and IFN-γ levels with commercial ELISA kit.
Microscopic observation on the lung tissues
Lung tissues were taken from each group of mice, fixed in 10% formaldehyde solution, embedded in paraffin, and sectioned in conventional technique. The tissue sections were stained with HE, and observed under on the infiltration of inflammatory cells and severity of the bronchial epithelial damage.
Statistical Analysis
One-way ANOVA was performed for the experimental results with SPSS version 16.0, and the data were expressed with x
s
. P < 0.05 was considered statistically significant.
RESULTS
Changes of symptoms in mice
Twenty minutes after aerosol inhalation of the extract in the first day, mice in the asthma group developed symptoms of restlessness, deep and fast breath, wheezing, convulsions and scratching. The symptoms moved up with increased inhalation frequencies, yet restored within several minutes upon withdrawal of the challenge.
However, notable asthmatic symptoms were absent in the mice in control group and another two groups treated with the two recombinant proteins, except for minor irritability and other mild responses.
Content of the serum specific antibodies
After challenging for 24 h, the allergen-specific serum IgE level was (26.86 ±
4.30) IU / ml and (7.86 ± 2.66) IU / ml in the asthma group and control group( P
<0.01), whereas the IgE level was (7.31 ± 1.83) IU / ml(9.11 ± 3.78) IU / ml and (8.02
± 2.20) IU / ml in groups treated with Der f 1, Der f 1A and Der f 1B, respectively, which was lower as compared with the asthma group( P <0.01). IgG2a level (23.72 ±
13.64) μg / ml for asthma group and (9.92 ± 2.49) μg / ml for the controls, and (38.45
± 8.40) μg / ml,(37.15 ± 5.58) μg / ml and (37.64 ± 7.51) μg / ml for groups respectively managed with Der f 1, Der f 1A and Der f 1B. The level of IgG2a was significantly higher in the latter three groups than the former two groups ( P <0.01).
Changes of antigen-specific cytokine IL-5 and IFN-γ levels in spleen cells
ELISA determination of the spleen cell culture supernatants (SSCS) indicated that the IL-5 level was (208.05 ± 10.66) pg / ml in the asthma group and (93.18 ±
10.27) pg / ml in the control group. The difference was significant ( P <0.01). The level of IL-5 (98.33 ± 13.06) pg / ml, (85.73 ± 14.71) pg / ml and (87.73 ± 15.29pg / ml for groups treated with Der f 1, Der f 1A and Der f 1B, respectively, and the difference was not significant as compared with controls ( P > 0.05).
IFN-γ level in SSCS was (75.81±17.96)pg/ml in asthma group compared to
(107.39 ± 13.62) pg / ml in the control group ( P
<
0.01), (105.51 ± 11.62) pg / ml,
(117.51 ± 15.33) pg / ml and (119.13 ± 14.68) pg / ml, respectively for Der f 1, Der f
1A and Der f 1B treatment group. The difference was significant as compared with asthma group( P
<
0.01), yet was not by comparison with the control group ( P >
0.05).
The changes of IL-5 and IFN-γ specific cytokine levels in BALF
ELISA measurement of the cytokine IL-5 level in the BALF demonstrated
(182.04 ± 13.94) pg / ml for the asthma group and (92.77 ± 11.99) pg / ml for the control group( P
<
0.01), and IL-5 level was (107.80 ± 11.61) pg / ml, (97.70 ± 13.51) pg / ml and (98.17 ± 13.60) pg / ml for groups treated with Der f 1, Der f 1A and Der f 1B, which were markedly lower than that of the asthma group( P
<
0.01).
IFN-γ level was significantly lower in asthma group than the control group[(62.97±14.07)pg/ml vs.
(91.00±13.64)pg/ml,
P
<
0.01], yet was higher in Der f
1(108.18±12.30) pg/ml, Der f 1A(118.48±10.79)pg/ml and Der f 1B
(115.19±9.36)pg/ml treatment group as compared with the asthma group ( P
<
0.01).
Cell count in the BALF
The count of WBC in the BALF was (22.11±3.70)×10
8
/ml in the control group and (5.61 ± 1.84) × 10 8
/ ml in the asthma group. The difference was significant( P
<
0.01). however the WBC count decreased to a certain degree, which was
(7.02±1.37)×10 8
/ml, (6.12±1.66)×10
8
/ml and (6.58±1.81)×10
8
/ml in the groups treated with Der f 1, Der f 1A and Der f 1B, respectively, and significantly lower than that of the asthma group( P
<
0.01).
Pathological changes of the lung tissues
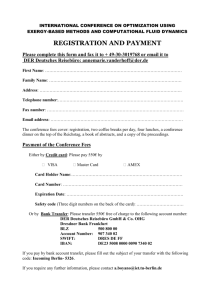
The bronchial structure and alveolar configuration remained regular and somewhat intact in lung tissues of mice undergone specific immunotherapy and controls. The mucosa at the bronchial wall also remained intact with no fracture and shedding. The small trachea and its peripheral vessels were free from infiltration of inflammatory cells and significant pathological changes (Fig. 1).
Fig. 1 Pathological section of lung tissues (HE staining ×400). Note: A: Control group;
B: Asthma group; C: Der f 1 SIT group; D: Der f 1A SIT group; E:Der f 1B SIT group.
DISCUSSION
Epitope, also known as antigenic determinant, is a special chemical group that decides the immunogenicity of antigen molecules in immune response, and a part of antigen that is recognized by immune system, once the body is stimulated to have produced antibodies or sensitized lymphocytes. The specific antibodies direct at antigen epitopes rather than the entire antigen protein. Therefore, research and development of the epitope vaccine on cellular immune mechanism can be of great importance for allergic disorders.
Epitope vaccine is commonly expressed in vitro in terms of genetic engineering technology, based on construction of the linear epitope, spatial binding of the conformatonal peptide and modification of the epitope, or is developed through artificial synthesis of the pathogenic microorganisms
19
. For one thing, epitope vaccine can counteract the disadvantages of traditional vaccine, such as virus-excretion and virulence recovery
20
, for another, this sort of vaccine has outstanding advantages of hypoallergenicity and high immunogenicity as well as immediate quantitative analysis on the antigenic epitope. Therefore, these preponderances represent promising strategies in developing the vaccines against allergic or other diseases.
In our experiment, we found that treatment of the asthmatic mice with the protein derived from the dust mite group I allergens and chimeric vaccine had led to inhibition of production of leukocytes in bronchoalveolar lavage fluid and reduction of the serum specific IgE level as well as level IL-5 secreted by Th2 cytokines in the spleen cell culture supernatant and in bronchoalveolar lavage fluid, eventually causing increase of IFN-γ secreted by Th1 cells. These findings showed that our proteins as
SIT, either prepared from simple dust mite group I allergens or developed through recombining of these allergens, can alleviate the symptoms of murine models of
asthma.
In summary, the chimeric epitope vaccine can effectively relieve the symptoms of and pulmonary inflammation for asthmatic mice to a certain extent. However, the efficacy remains to be boosted in order to develop a vaccine with higher potency by following optimization and screening of the chimeric genes.
DECLARATION
The partial content of this paper was published in Chinese under the title of
“Effect of immunotherapy of recombinant chimeric epitopes of major aller-gen group
1 from Dermatophagoides farinae on asthma of mice” in Chin J Schisto Control 2015;
27(1): 49-52.
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (No.
81270091; No. 30872367), and the Natural Science Foundation of Anhui Province
(No. 070413088).
DISCLOSURE The authors have no financial conflict of interest.
REFERENCES
1. Crameri R. High throughput screening: a rapid way to recombinant allergens .
2.
Allergy 2001; 56 Suppl 67: 30-4.
Price MM, Oskeritzian CA, Falanga YT, Harikumar KB, Allegood JC,
Alvarez SE, Conrad D, Ryan JJ, Milstien S, Spiegel S. A specific sphingosine kinase 1 inhibitor attenuates airway hyperresponsiveness and inflammation in a mast cell-dependent murine model of allergic asthma .
J Allergy Clin
Immunol 2013; 131(2): 501-11.e1.
3. Chang YS, Kim YK, Jeon SG, Kim SH, Kim SS, Park HW, Min KU, Kim YY,
Cho SH. Influence of the Adjuvants and Genetic Background on the Asthma
4.
Model Using Recombinant Der f 2 in Mice .
Immune Netw 2013; 13(6):
295-300.
Zhao JH, Wang HN, Jiang YX, Li CP. Construction of mouse model with asthma induced by recombinant Der f1 .
J Qiqihar Univ Med 2011; 32(20):
5.
6.
7.
8.
3257-9(in Chinese).
Till SJ, Francis JN, Nouri-Aria K, Durham SR. Mechanisms of immunotherapy .
J Allergy Clin Immunol 2004; 113(6): 1025-34; quiz 35.
Bousquet J, Lockey R, Malling HJ. Allergen immunotherapy: therapeutic vaccines for allergic diseases. A WHO position paper .
J Allergy Clin Immunol
1998; 102(4 Pt 1): 558-62.
Sheikh A, Smeeth L, Hubbard R. There is no evidence of an inverse relationship between TH2-mediated atopy and TH1-mediated autoimmune disorders: Lack of support for the hygiene hypothesis .
J Allergy Clin Immunol
2003; 111(1): 131-5.
Li K, Wang Z, Cao Y, Bunjhoo H, Zhu J, Chen Y, Xiong S, Xu Y, Xiong W.
The study of the ratio and distribution of Th17 cells and Tc17 cells in
9. asthmatic patients and the mouse model .
Asian Pac J Allergy Immunol 2013;
31(2): 125-31.
Prescott SL. Maternal allergen exposure as a risk factor for childhood asthma .
Curr Allergy Asthma Rep 2006; 6(1): 75-80.
10. Repa A, Wild C, Hufnagl K, Winkler B, Bohle B, Pollak A, Wiedermann U.
Influence of the route of sensitization on local and systemic immune responses in a murine model of type I allergy .
Clin Exp Immunol 2004; 137(1): 12-8.
11. Larche M, Robinson DS, Kay AB. The role of T lymphocytes in the pathogenesis of asthma .
J Allergy Clin Immunol 2003; 111(3): 450-63; quiz
64.
12. Valenta R, Campana R, Marth K, van Hage M. Allergen-specific immunotherapy: from therapeutic vaccines to prophylactic approaches .
J
Intern Med 2012; 272(2): 144-57.
13. Jutel M, Akdis CA. Immunological mechanisms of allergen-specific immunotherapy .
Allergy 2011; 66(6): 725-32.
14. Zhao D, Qiao C, Zhang Q, Guo JH, Gao FS. Progress on Epitope-Vaccine .
Prog Vet Med 2012; 33(1): 102-6(in Chinese).
15. Zhou WY, Wu C, Shi Y, Zou QM. Construction and prokaryotic expression of the double unit epitope vaccine of Helicobactor pyloriand its immunogenicity .
Chinese J Zoonoses 2008; 24(1): 33-7(in Chinese).
16. Chen JG, Su ZL, Liu YZ, Wang SJ, Peng SF, Li YZ, Shao QY, Xu HX.
Construction and biological effect ofPseudomonas aeruginosa multiepitope vaccine .
J Jiangsu Univ (Med Edit) 2008; 18(6): 484-6(in Chinese).
17. Xu HF, Xu PF, Wang KX, Li CP. Construction and expression of a chimeric gene with T-/B-cell epitopes of major allergen group 1 from
Dermatophagoides farinae.
Chinese J Schisto Control 2014; 26(4): 420-4(in
Chinese).
18. Jiang YX, Ma YC, Li CP. Effect of immunotherapy on asthma mice w ith chimeric allergens derived from the major allergen group 2 genes of dust mites .
J Shandong Univ (Health Sci) 2012; 50(10): 50-5(in Chinese).
19. Zhou WY, Shi Y, Wu C, Zhang WJ, Mao XH, Guo G, Li HX, Zou QM.
Therapeutic efficacy of a multi-epitope vaccine against Helicobacter pylori infection in BALB/c mice model .
Vaccine 2009; 27(36): 5013-9.
20. Shi XN, Dou YX, Cai XP. Advance in epitope vaccines .
Chinese Vet Sci 2011;
41(4): 422-6.