Disorders of sleep kto
advertisement

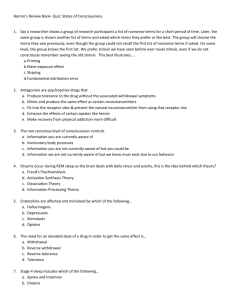
Disorders of Sleep Insomnia Narcolepsy Sleep Walking My day out with narcolepsy • Watch the clip. • What is life like from this mans perspective. • How does his sleep disorder affect his life? Disorders of Sleep - Insomnia Insomnia Narcolepsy Sleep Walking My day out with narcolepsy • Watch the clip. • What is life like from this mans perspective. • How does his sleep disorder affect his life? Disorders of Sleep - Insomnia A C E Evaluate the risk factors for Insomnia Give some explanations for primary insomnia Describe the difference between primary and secondary insomnia Check it out….. • http://www.bbc.co.uk/science/humanbody/sl eep/ Two categories of sleep disorder Type Description Daytime sleepiness? Examples Dysomnias Problems with amount or quality of sleep. Yes Insomnia Narcolepsy Parasomnias Behavioural or physiological events during sleep Not usually Sleep walking Night terrors Insomnia • What is it? • More than just “ I can’t sleep”, we all get that from time to time, maybe because we are stressed, anxious or excited. • To be diagnosed with insomnia you need proper diagnostic criteria. Diagnosing Insomnia- criteria Takes more than 30 min to fall asleep Spend less than 85 % of time in bed actually asleep Wake up frequently Suffer at least 3 times a week • Must last longer than a month to be diagnosed as clinical insomnia! Primary and secondary insomnia • Quite often insomnia can be caused by another medical or psychological condition, e.g. depression. In these cases it is known as ‘secondary insomnia’ • Primary insomnia is chronic insomnia where there is no other medical condition that might explain it. This is important for treatment! Primary Insomnia • There are a few different types of primary insomnia 1. Psychophysiological insomnia 2. Idiopathic insomnia 3. Sleep state misperception 1) Psychophysiological insomnia • Learned or Behavioural Insomnia • A vicious cycle of worry and stress! 1) Psychophysiological insomnia • Fall asleep in front of the TV but not in Bed? • It is suggested that this occurs because the learned associations are not present in the new or unfamiliar sleep environment. Primary Insomnia • Treatment for learned insomnia aims to improve sleep habits and reduce unnecessary worry. 1) Research on psychophysiological insomnia:Dauvilliers et al (2005) • Dauvilliers asked 256 consecutive primary insomniacs to complete a clinical interview, psychometric questionnaires, a questionnaire on the family history of insomnia and, when indicated, a polysomnography (a series of detailed physiological recordings of their sleep). • A control group was also used to obtained an estimated base-rate incidence of insomnia in their families. Results showed that of those patients with primary insomnia (n=77), 72.7% reported familial insomnia compared with 24.1% in the non-insomnia control group. • These findings suggest a familial link to primary insomnia. Primary Insomnia 2) Idiopathic Insomnia • This was originally called childhoodonset insomnia because it tends to occur at a very early age. • It is thought to occur due to an abnormality in the brain mechanisms that control the sleep-wake cycle. • It is suggested that a neurochemical lesion exists in the sleep system, in which patients tend to be on the extreme end of the spectrum towards arousal and thus have an inability to sleep normally. Primary Insomnia 3) Sleep state misperception • When asked about sleep, these people underestimate their total sleep time and overestimate the time it took them to fall asleep. • Dement (1999) cites a case where a patient who complained of severe insomnia was asked to sleep for 10 consecutive nights in the sleep lab. Each morning he was asked to complete a questionnaire where he had to estimate how long he took to fall asleep each night. He reported times ranging from 1 to 4 hours to fall asleep, with a mean of 90mins. According to Dement’s sleep lab recordings, he never took more than 30mins to fall asleep and the mean was 15 mins! Primary Insomnia Secondary Insomnia (More common) • There are a number of physical and psychiatric causes of secondary insomnia, including the following: – Hormonal changes in women, these include premenstrual syndrome, menstruation, pregnancy and menopause. – Decreased melatonin production: the levels of melatonin, the hormone that helps control sleep, decrease as a person ages. By age 60, the body produces very little melatonin. – Medical conditions: many medical illnesses can disrupt sleep and produce insomnia. These include allergies, arthritis, asthma, heart disease, high blood pressure and Parkinson’s disease. – Psychiatric conditions: secondary insomnia is a common symptom of depression. It is also associated with anxiety disorders, PTSD and dementia. Explanation 1- it’s Psychological • Insomnia is a learned response to night time cues, you need to unlearn your current cues and get some new cues- a new bed time routine! • The fact that this works is evidence that this is the problem! – – – – Only go to bed when sleepy Only use your bedroom to sleep in, not work or watch TV Get up at the same time every day Do not take naps Explanation 2- its down to high levels of arousal • High levels of arousal, whether it is down to anxiety, depression or anxiety about sleep itself are likely to interfere with the brains sleep mechanisms. • How do we solve it? CBT or relaxation techniques Explanation 2- Solution: CBT • “ I won’t sleep” “I need sleep” “if I don’t sleep, I won’t cope tomorrow!” The more someone with insomnia tries to sleep, the more anxious they get! • CBT challenges some of these assumptions and reduces anxiety. • Again, the fact that it works is evidence for this explanation (ditto relaxation techniques). Explanations for Insomnia • Whilst you don’t strictly speaking need to know about treatments for insomnia- if a treatment works well, it is likely to be because it has something to do with the cause of it, so it isn’t a waste of time! 1. It’s psychological 2. Its down to high levels of arousal 3. Its faulty brain mechanisms Explanation 3- Faulty brain mechanisms • The most prescribed psychological drug over the last 40 years has been nitrazepam (aka Mogadon), which was a sleeping pill. • Whilst it does increase the time spent asleep, it interferes with the normal ultradian patterns. They lead to morning sleepiness and make the insomnia worse when you stop taking them! Explanation 3 contd • Obviously, if the insomnia is secondary to another complaint- then drugs to treat the original problem will also reduce the insomnia Personality Factors and Genetics • How much sleep do you need a night? Einstein needed 10 hours, Margaret Thatcher only needed 4! • It seems to vary, the average people GET is about 7.5 hours a night, 16% get less than 6.5, 16% more than 8.5 hours. (not much variation there!) Personality • So what is it that means some people need more, or less? • Neuroticism seems to be associated with insomnia (Heath et al 1998, did a twin study that showed higher neuroticism more insomnia). Personality- Chronotype • Are you a ‘morning person’ or an ‘evening person’? A ‘lark’ or an ‘owl’? Larks and Owls (chronotypes) • The circadian rhythms of larks is roughly 2 hours ahead of owls and this difference is genetic. • Chronotypes are stable over seasons and lifetimes, controlled by endogenous pacemakers, controlled by ‘clock’ genes. • A distinct personality trait that is genetically determined! Chronotypes- so what • Well, not much- but maybe owls should not try to go to bed too early! And Larks just shouldn’t try to stay up too late! Plenary • • • • You are suffering from a sleep disorder – describe your symptoms (write them down) 2mins Pass your symptoms along 4 people Now diagnose the patient who has been passed to you– how will you treat this client? Why? Investigating Insomnia worksheet Essay Questions Outline and evaluate explanations of two or more sleep disorders (24 Marks) PPP Factors Predisposing Genetics Precipitating Environmental Stressors Perpetuating Stress due to sleep problems! Narcolepsy • Describe the symptoms of Narcolepsy • Outline and evaluate explanations for Narcolepsy. REM hypothesis Mutation in HLA Hypocretin Narcolepsy First identified as a medical condition in early 20th century. Onset is early adulthood or adolescence but can occur early or later in life Affects about 0.5-1 in 1000 people worldwide so very rare. http://www.youtube.com/watch?v=3MBCeK n0Oeo Narcolepsy Symptoms 4 general symptoms associated with Narcolepsy: 1) Excessive daytime sleepiness and sudden sleep attacks: These can occur at anytime (even while eating or driving). An episode lasts about 10-20 mins. 2) Sleep paralysis: A consciously experienced inability to move just prior to falling asleep or waking up. 3) Dreamlike experiences: whilst still awake and just before falling asleep or just before being fully awake 4) Cataplexy: Skeletal muscles weaken or are paralysed and the person collapses and enters REM sleep. It is often triggered by an emotional event (Laughter or anger) Explanations for Narcolepsy The REM hypothesis The narcolepsy-HLA link Hypocretin Explanations for Narcolepsy The REM hypothesis-A kind of REM sleep at an inappropriate time (Popular explanation in 1950s) Malfunction in the system that regulates REM sleep In cataplexy neurons in the medulla, which are active during REM and suppress skeletal muscles are activated when they shouldn’t be. It explains some of the symptoms of narcolepsy, such as lack of muscle tone (Cataplexy) which match REM sleep Explanations for Narcolepsy Evidence for The REM hypothesis Vogel (1960) observed sleep patterns during narcoleptic episodes in one patient and found (as predicted) that REM patterns were present at the beginning of each episode. Siegel (1999) recorded activity in brainstem of narcoleptic dogs and found the same activity during cataplexy as found in REM sleep. However… generally research support has not been convincing. Explanations for Narcolepsy Mutation in HLA Possibly linked to a mutation of the immune system. Honda et al (1983) found increased frequency of one type of human leukocyte antigen in narcoleptics. However..unlikely to be the sole explanation as HLA mutation was found in some but not ALL narcoleptics and also common in the general population (Mignot et al 1997) Explanations for Narcolepsy Hypocretin (neurotransmitter) 1990s American research team found that mice who could not make the neurotransmitter called hypocretin (aka orexin) displayed sleep attacks and cataplexy Lin et al (1999) found some strains of dogs (Labradors & Dobermans) also exhibited narcolepsy following excitement. The researchers identified a mutant gene on chromosome 12 in the dogs which affects neurons that secrete hypocretin. Narcolepsy Hypocretin-secreting neurons are normally active during wakefulness and keep the brain from shutting down unexpectedly. So, narcolepsy is caused by a deficiency of hypocretin. Supported by stimulant drugs used to treat narcolepsy in humans and dogs work by activating hypocretin- containing neurons. hypocretin levels in the cerebrospinal fluid of narcoleptics are v low and narcoleptics have lost 90% of hypocretin-secreting neurons from the hypothalamus (Nishino 2000) Low levels of hypocretin are not linked to inherited factors because narcolepsy doesn’t run in families (Mignot) Sleep walking • Describe the symptoms of Sleep Walking • Outline and evaluate explanations for Sleep Walking Sleep walking (Somnambulism) Is an example of a parasomnia Most common in childhood,(age 4-6) affecting 20% of children and less than 3% adults (Hublin et al 1997). More common in boys Occurs during NREM/SWS related to night terrors Walk around as if awake, involves ordinary behaviours like dressing or making food. A sleep walker is not conscious and later has no memory of events during sleep walking Sleep Walking • Sleepwalkers are difficult to wake • Each episdode can last for a few seconds or minutes • It is not dangerous to wake a sleep walker up Explanations Incomplete arousal EEG recordings of sleepwalkers show delta waves (typical of SWS) and beta waves (awake state) Seems that it occurs when a person in SWS is awakened but arousal of brain is incomplete. This abnormal arousal is likely to be genetic Explanations Other factors Increase likelihood of SW such as sleep deprivation Alcohol Fever Stress Hormonal changes in puberty A.I.Ds Nature & Nurture Can be explained by the Diathesis-Stress model Genetic basis for SW Prevalence of SW in first degree relatives is 10X greater than the general population (Broughton 1968) 50% concordance in MZ twins compared with only 15% in DZ twins Gene identified for sleep walking (DQB1*05 gene) Environmental component Maturity of brain circuits-immaturity leads to SW Amount of SWS e.g. factors such as sleep deprivation increase SWS so SW becomes more likely Being a child is related to all of above (immature and high levels A.I.Ds Real World Application Research has suggested a way to diagnose vulnerability to sleep walking. 40 patients referred to a clinic for suspected SW were observed before and after 25 hours of sleep deprivation. Before sleep deprivation 50% of the patients showed episodes of SW and after it rose to 90%. A.I.Ds Real World application Cases of murder Is a person really sleepwalking? E.g. Jules Lowe killed his father & Brian Thomas killed his wife Plenary • • • You are suffering from a sleep disorder – describe your symptoms (write them down) 2mins Pass your symptoms along 4 people Now diagnose the patient who has been passed to you– how will you treat this client? Why? Essay Questions Outline and evaluate explanations of two or more sleep disorders (24 Marks) Sleep specialist • • • • • • • • • • Review case histories of patients, make diagnoses, and recommend treatments. You have the primary information for the two case histories . Write down what you consider to be the key aspects of their patients’ sleep disorders in the appropriate box on the Sleep Specialist’s Evaluation Form Using Sleep Disorders Reference Manual. Make a preliminary diagnosis for each case history. Write your preliminary diagnoses in the appropriate boxes on their evaluation form. List the matching symptoms of the sleep disorders that match the key aspects of your case histories. Some additional information regarding each case has come to light you will be given some Secondary Information. Read the Secondary Information for each case and use this new information to re-evaluate your diagnoses. If students have changed a diagnosis, you should enter the new diagnosis, together with the reason for the change, in the appropriate boxes on the evaluation form. Recommend a treatment. You will be given the bottom portion of the appropriate case histories that contains discussion questions to complete