File
advertisement

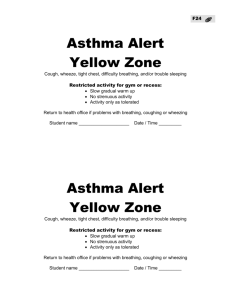
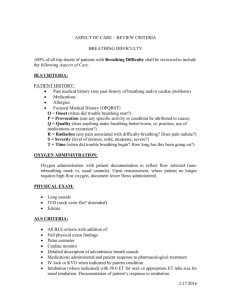
Concept Map Care Plan N360 Impaired Swallowing Pureed diet, thickened honey liquids Evaluated by speech therapist Hx CVA, Dementia Non-verbal Limited awareness Impaired Physical Mobility Contracted bilateral legs with slight movement Hx of CVA- right sided weakness Reposition q2h ROM Impaired Tissue Integrity Impaired mobility Rt heel pressure ulcer Excoriated buttocks Scratching buttocks Inzo cream to buttocks Safegel to heel Daily dressing change for heel Karissa Higa Risk for Unstable BG Level BG 200s-300s- hyperglycemia BG 31- hypoglycemia Diabetes II Regular Insulin Sliding Scale D50 1 amp prn Chief Medical Diagnosis: Asthma Priority Assessments: Breathing Pattern, Lung Sounds, O2 Sat., LOC., BG checks, VS, Wound Assessment, sign of hypo or hyperglycemia, temperature. Hypothermia Temp. 35 C Hypoglycemic Warm to touch Added blanket and towel to keep warm Ineffective Breathing Pattern Wheezing Hx COPD Advair Prednisone Ineffective Airway Clearance Wheezing Coughing Hx COPD Advair Prednisone Concept Map Care Plan N360 Desired Outcomes Ineffective Breathing Pattern The patient will maintain an effective breathing pattern, as evidenced by relaxed breathing at normal rate and depth and absence of dyspnea. Karissa Higa Interventions Ineffective Breathing Pattern Assess respiratory rate, rhythm, and depth. Monitor breathing patterns. Assess breathing position Monitor for changes in LOC and VS Assess skin color and temperature Use pulse oximetry to evaluate O2 saturation. Encourage pt to clear his own secretions with effective coughing. Administer prescribed medications. Teach caregivers appropriate breathing, coughing, and splinting techniques. Educate pt and caregivers about prescribed medications. Explain use of oxygen therapy, including type and se of equipment and why its maintenance is important. Ineffective Airway Clearance Ineffective Airway Clearance Patient will maintain clear Assess airway patency open airways as Auscultate lungs after coughing for presence of adventitious breath sounds. evidenced by normal Assess respirations, not quality, rate, rhythm, depth, flaring of nostrils, dyspnea on exertion, breath sounds, normal evidence of splinting, use of accessory muscles, and position for breathing. rate and depth of Assess changes in LOC respirations, and ability to Assess changes in HR, BP, and temperature. effectively cough up Assess cough for effectiveness and productivity. secretions after Assess secretions, noting color, viscosity, odor, and amount. treatments and deep Use pulse oximetry to monitor oxygen saturation; assess ABGs. breaths. Assist in pt. performing coughing and breathing maneuvers. Use upright position If cough ineffective, use nasotracheal suctioning as needed. Administer medications as ordered noting effectiveness and side effects. Instruct caregivers regarding need for humidification and adequate hydration Instruct caregivers on prescribed medications and coughing techniques. Concept Map Care Plan N360 Risk for Unstable BG Level Pt maintains BG within defined target ranges. Hypothermia Pt maintains body temperature above 35°C. Impaired Mobility Patient is free of complications of immobility, as evidenced by intact skin, absence of thrombophlebitis, normal bowel pattern, and clear breath sounds. Impaired Tissue Integrity Pt’s tissues return to Karissa Higa Risk for Unstable BG Level Assess for signs of hyperglycemia and hypoglycemia Monitor BG as ordered (before every meal and HS) Assess pattern of physical activity Educate pt/caregiver on medications, insulin administration, signs and symptoms of hyperglycemia and hypoglycemia Hypothermia Monitor temperature Assess heart rate, rhythm, BP, O2 sat Determine precipitating factor/event Monitor labs Apply extra blankets to keep pt warm Bear hug order Explain all procedures and treatments Impaired Mobility Assess for impediments to mobility Assess ability to perform ROM to all joints Monitor nutritional status Evaluate need for assistive devices and home assistance Assess skin integrity Assess elimination status Allow pt to perform takss at his own rate, do not rush pt Provide positive reinforcement Institute measures to prevent skin breakdown Reposition q2h Encourage CDB Instruct caregiver on hazards of immobility Educate caregivers on safe home environment, exercises (ROM), nutrition importance, and medications. Impaired Tissue Integrity Assess condition of tissue Concept Map Care Plan N360 normal structure and function. Impaired Swallowing Patient exhibits ability to safely swallow, as evidenced by absence of aspiration, no evidence of coughing or choking during eating/drinking, no stasis of food in oral cavity after eating, and ability to ingest foods/fluid. Karissa Higa Assess characteristics of wound, including color, size, drainage, and odor Assess VS for elevated fever Identify signs of itching and scratching Provide skin care as needed Administer antibiotics as ordered Encourage diet that meets nutritional needs (protein to promote wound healing) Teach pt or caregiver about proper wound care, signs and symptoms of infection, and when to notify PCP Assess for presence of gag and cough reflexes Assess strength of facial muscles Assess coughing or choking during eating and drinking Assess ability to swallow small amount of water Assess for residual in food in mouth after eating Assess results of swallowing studies as ordered Maintain high fowlers position with head flexed Provide small frequent meals Encourage pt to chew thoroughly, eat slowly, and swallow frequently, especially if extra slaiva is produced. Proceed slowly, giving small amounts; whenever possible, alternate servings of liquied and solids Place whole or crushed pills in custard or gelatin Demonstrate to the pt, caregiver, or family what should be done if pt aspirates Encourage family members to seek out CPR instruction Evaluation: For ineffective breathing pattern I determined if the outcome was met by evaluating the pts breathing pattern, O2 sat, respiratory status and LOC. After these assessments the pt had an O2 sat of 99% on room air, respiratory rate of 20 breaths/min, unlabored breathing and no use of accessory muscles. Pt was disoriented x3 related to his hx of dementia. Overall, pts breathing pattern was acceptable and showed no signs of respiratory distress, and outcome was met. For ineffective airway clearance I evaluated the pts respiratory status, once again, plus assessed his cough effectiveness and productivity to calculate if the outcome was met. After my assessments pt couldn't cough when told but when he did his Concept Map Care Plan N360 Karissa Higa lungs were clear after auscultation. Initially in the morning the pt had wheezing on expiratory but after medication administration his lungs were clear. Overall, pts outcome was partially met as evidenced by normal respiratory rate and depth, but unable to cough up secretions after treatments and deep breaths. Risk for unstable BG was monitored by glucose checks before every meal and at nighttime. Unfortunately, my pts glucose levels fluctuated constantly. Usually by dinnertime his glucose was in the high 300s to low 400s so according to the sliding scale more insulin was needed. However, by the time the glucose reading came in for the morning he had dropped to 31 and was now hypoglycemic. Once the nurses saw that value D50 1 amp was given and pt glucose went back up after 30min. I continued to monitor him throughout the day and pt remained asymptomatic when his glucose increased to 180 at lunch. Insulin was given at lunch and pt ate 100% of his meal. Overall, pt remained comfortable in bed by the end of my shift but the goal was not met. This week my pt also suffered from hypothermia with a temperature of 34C-35C. After assessments I reported the abnormal to my nurse and we discussed about ordering a bear hug, but it didn't not happen. Instead I put extra blankets on the pt and put a towel over his head and neck to try and warm him up. I was constantly taking temperature every 30min to make sure his temperature was going up. By the end of my shift his temperature had risen to 35.7C so the outcome was eventually met. My pt was also immobile and stayed in bed the whole time. His legs were contracted with some movement and he had right sided weakness due to a hx of CVA. He was a total assist pt so I made sure to reposition him q2h, check his briefs for incontinence, and kept his skin clean and dry. Patient’s goal was partially met due to the pressure ulcer on his heal and excoriated buttocks. For impaired skin integrity my pt had a right heel pressure ulcer and excoriated buttocks. I applied barrier cream to his buttocks and changed the heel dressing. I assessed the wound at the heel and it looked like it was healing well. However, pt goal was not met due to the healing wound and excoriation to the buttocks. For impaired swallowing my pts goal was met and he did not aspirate while I fed him. He was great at chewing his food and I made sure to feed him slowly. After I was sure he swallowed all his food I gave him another spoonful of food. I also alternated food and liquids to prevent food from being left in the mouth. Lastly, I crushed the pts medications and mixed it with thickened juice to prevent aspiration. Discharge Plan/ Patient Teaching: 1. Placement: Home 2. Support systems: family- daughter and family, wife 3. Assistance needed w/ ADLs: Feeding, oral care, bathing, PROM, turn q2h, peri care, all done by family. Concept Map Care Plan N360 Karissa Higa 4. Equipment needs: Safegel, Keflix, and Telfa for wound care on heel, nebulizer for updraft treatments as needed, thickener for feeding (nectar consistency diet for dysphagia), syringes for insulin administration, barrier cream for buttocks (Inzo), briefs and chux. 5. Patient teaching: a. How pt learns: Educate caregivers, pt disoriented x3 b. Barriers: Primary language Filipino, non verbal most of the time c. Topics to be addressed: Medications, wound care, reposition q2h, when to call PCP, how to prevent asthma attacks, insulin administration, body temperature regulation, PROM exercises, home safety (prevent falls, skin breakdown, clutter free, etc), finances if applicable, resources for emotional support, educate on caregiver strain and how to prevent it, home care agencies to help relieve family members, insurance to decrease cost of medications and supplies.