to view the Podiatry Annual Report
advertisement
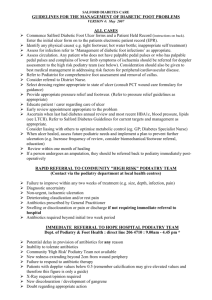
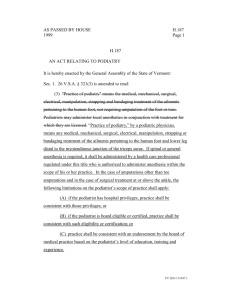
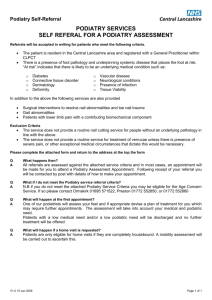
Mangere Community Health Trust PODIATRY SERVICE Annual report 2012 17 January 2012 to 31 January 2013 Compiled by Tokhy Hoang on behalf of: Mangere Community Health Trust P O Box 43-161 10 Waddon Place Mangere Auckland Phone 09 255-0602 Fax 09 255-1673 Mangere Community Health Trust Podiatry Service Annual Report 1 SERVICE DEVELOPMENT INTRODUCTION Within Counties Manukau District Health Board (CMDHB) there is an estimate of 34,000 people in the Manukau district diagnosed with diabetes and over 12,000 in the Mangere community alone. Patient education and accessible care are vital aspects to reducing preventable foot complications. The overall goal of patient education is to allow the patient to be informed and work together with the podiatrist to implement a suitable plan that meets the patient’s health needs. The Mangere Community Health Trust (MCHT) focuses strongly on improving patient access to care by being in the heart of Mangere community, completely FREE of charge and in a warm welcoming environment. The Community ‘Foot Clinic’ Podiatry Service was established in January 2012 to maintain and improve the foot health status of patients with diabetic foot-related pathologies. The service is accessible to patients within the Mangere catchment and enrolled with a local general practitioner. The aims of the service are to: Reduce the number of lower limb amputations within the Counties Manukau district. Decrease hospital admissions for foot-related complications associated with diabetes Identify and educating High Risk patients Provide a comprehensive assessment service Provide a free, appropriate and accessible service for Diabetic patients within Mangere Initiate preventive measures when necessary Provide podiatric management as appropriate Educate health professionals, patients, whanau, and members of the community in aspects of podiatry and diabetic foot pathology. The service is free to all diagnosed diabetic patients who meet the referral criteria and who are not currently in a hospital-based treatment programme. The Community Podiatry Service offers an initial assessment to all patients who meet the referral criteria. Following the initial assessment, the service may: Refer on to hospital care if required, for example Manukau SuperClinic Ulcer and Vascular teams Refer on to other health services provided within the Diabetes Hub i.e. dietitian, retinal screening or smoking cessation. Recall the patient weekly for a short course of treatment of an acute infection Recall the patient for ongoing assessments based on risk levels Diabetic Foot Category Refer the patient back to the GP/nurse along with advice on care and management. Refer on to Orthotic Centre - due to limited funding and resources, some treatments are outside the scope of our Community Podiatry Service. For example, there is no provision for orthoses or specialised footwear. We currently refer patients on to the Orthotic Centre based in Ellerslie for assistance in insoles and footwear. All patients seen within the service have a summary of their visit sent to the initial referrer and/or primary care provider to ensure continuity of care. Mangere Community Health Trust Podiatry Service Annual Report 2 Many of the PHO’s within the Mangere area have had Podiatry services offered in-house to manage their Diabetic populations in the past. However, a change to the funding structure has meant that these services are no longer available within many PHO/Primary Care settings. Additionally, where podiatry services are still offered at PHO/Primary Care level the majority of the Podiatry clinics operate once a month, this is a significant limitation for many patients in Mangere. The MCHT ‘Diabetes Foot Clinic’ has two podiatrists, Tokhy Hoang and Asia Jones. The clinic operates five days a week and provides late night and Saturday clinics. The two podiatrists have one shared day once a week where they are able to discuss various issues and provide clinical support for each other. Clinics are held at two sites in Mangere; the main clinic is situated at the Diabetes Hub, 10 Waddon Place and a satellite clinic at Te Puea Marae Medical Centre. PATIENTS, FAMILIES AND WHANAU Patient education is essential and is being provided on a one-to-one basis at each assessment. With Maori and Pacific patients we encourage family/whanau members to come along as well, provide them with information and to help reinforce the importance of foot care and management of diabetes within the home environment. RELATIONSHIPS AND CLINICAL NETWORKS Diabetes is a complex condition which requires an approach that integrates efficient collaboration and communication within the wider inter-disciplinary team. To provide equitable, seamless effective diabetes podiatry care, we require that these various components work together with patients and their family to ensure the care provided is appropriate for an individual's needs based on the stage, type and status of their diabetes. Ensuring strong linkages with other services are crucial to the quality of service delivery provided by the service. Integration requires a team of dedicated professionals to enable the service to work well for both patients and clinicians. There is strong day-to-day communication between the Podiatrists and members of local diabetes care. There is evidence that effective collaboration between the three tiers of care can reduce hospitalisation and essentially provide better care to patients and carers alike (Diabetes UK, 2009). Primary tier Retinal screeners Dieticians Health promoters General practitioners Pharmacists Diabetes nurse specialists Other primary podiatry services within the community Physiotherapists Smoking cessation team Mental health advisor Mangere Community Health Trust Podiatry Service Annual Report 3 Secondary tier Secondary podiatry services - Manukau Superclinic, Greenlane Hospital, Middlemore Hospital (accordingly to patient’s residence) Orthotists Prosthetists Tertiary tier Orthopaedics Vascular specialists Rheumatologists Neurologists EXTENSION OF PODIATRY SCREENING SERVICE: Nail Surgeries Ingrown nail infections (onychocryptosis) occur when the edge of the nail grows into the skin and pierces the flesh as it grows out. Ingrown nails can lead to serious diabetic foot complications because it can quickly progress to a secondary infection such as osteomyelitis (infection tracking into the bone joint causing bone destruction) which could result in an amputation. An amputation would result in loss of mobility, placing severe restrictions on daily living activities and quality of life. MCHT podiatry has performed two partial nail avulsion surgeries on patients suffering chronic ingrown nails. During each procedure we used phenolisation to prevent re-growth of the nail edges to provide long-term results (Appendix 4). Potential costs saved so far (average per patient): Podiatry visits $55 each consult x5 =$275 Chemical matrixectomy= $500 Total podiatry intervention $775 VS amputation and secondary care-$11,000 minimum Other factors associated with loss of limb: - Loss in quality of life - Loss in income - Shorter life expectancy - Depression and other psychological issues (Data is based on the guidelines from Diabetes NZ, 2005) MANAGEMENT OF REFERRALS AND SERVICES DELIVERED Referral Criteria Service users may be referred by: General practice; A midwife; Or other providers of a diabetic service (e.g CMDHB diabetes clinic; podiatrist; nurse specialist) Entry Criteria Services users will be Mangere Community Health Trust Podiatry Service Annual Report 4 Patients with diabetes; and Be registered with a GP within Mangere Reside in the Mangere Referral Data A total of 1961 patients were referred to the service from commencement for the 12 months from January 2012 to January 2013. For the six months from July to December 2012, 1090 patients had been referred into the service compared to 743 for the previous 6 months. From the large number of referrals 1382 patients attended appointments. Referral sources either come from the following. Referrer GP Midwife Internal (Eye screening/ Dietician) CMDHB Diabetic Nurses Manukau SuperClinic Total 311 1 1111 52 30 The number of referrals from GPs, nurses, and the Manukau Super clinic was relatively low within the first half of the year; however there has been a steady increase as the service became established. Attendance rates With the high number of referrals, attendance is an issue. This needs to be addressed over the next year. Attendance 579 Screened DNA/ No contact 1382 Sites Currently, the Mangere ‘Foot clinic’ is based: Mangere Health Centre and, Te Puea Marae The location of both clinical sites are easily accessible to patients in Mangere with strong emphasises placed on providing services to both Maori and Pacific provider clients. Initial Assessment Appointments are made for all referred patients within one week of receiving the referral. A Podiatrist assesses each patient referred. Assessments generally take about 30-minutes depending Mangere Community Health Trust Podiatry Service Annual Report 5 of the health of the foot at presentation. Consultations involve a complete vascular, neurological, musculoskeletal, and dermatological examination and risk assessment of the patient. From the initial assessment a realistic and agreeable treatment plan is implemented for the patient and whanau. The outcome of the assessment will determine how often the patient will be recalled. This is based on the ‘Diabetic Foot Categorisation tool 20101’ (Appendix 1). The referrer receives a letter of podiatry assessment results which includes risk categorisation, treatment plan and recommendation date for review. Encounter by Type Ethnicity Breakdown of Patients Seen 17 Jan 2012 to 31 Jan 2013 There is a higher incidence of diabetes in the Maori and Pacific population within Counties Manukau, as is the lower of this population for free diabetes annual reviews and the relatively poorer health status of this population group. 25% of screened patients were Maori, 30% Samoan, 13% Cook Island, 17% Tongan, and 14% a mixed Pacific. Ethnicity NZ European NZ Maori Samoan Cook Island Tongan Other PI Indian Asian Other 185 334 419 174 234 198 89 23 65 23 Ethnicity Breakdown 89 65 185 NZ European 334 NZ Maori Pacific Islanders Indian 1025 Asian Other 10% of the patients with known diabetes in CMDHB are Maori and 15% are Pacific. 19% of podiatry service users are Maori and 60% are Pacific. This indicates the service is responsive to the needs of Maori and Pacific peoples. Foot Classification The “Ankle Brachial Index” (ABI) is part of the Diabetic Foot screening Tool (shown in Appendix 2) and is used to assist in the classification of the patient’s risk of peripheral vascular disease. The ABI is the ratio of the blood pressure in the lower legs to the blood pressure in the arms. Compared to Mangere Community Health Trust Podiatry Service Annual Report 6 the arm, lower blood pressure in the leg is an indication of blocked arteries (peripheral arterial disease - PAD). The ABI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressures in the arm. 800 734 700 600 500 400 300 207 200 50 100 21 13 0 Low Risk (0) Quarterly Break down ABI Low Risk (0) At Risk (1) At Risk (2) High Risk (3) Active Complication (4) At Risk (1) Jan 24 1 0 0 0 At Risk (2) Feb 68 13 7 0 1 ABI Low Risk (0) At Risk (1) At Risk (2) High Risk (3) Active Complication (4) Apr 87 17 3 1 0 May 62 19 2 0 1 ABI Low Risk (0) At Risk (1) At Risk (2) High Risk (3) Active Complication (4) July 57 17 6 2 0 August 85 19 7 4 1 High Risk (3) Mar 68 8 11 0 2 Total 160 22 18 0 3 June 67 16 5 3 2 Total 216 52 10 4 3 September 58 30 2 1 2 Mangere Community Health Trust Podiatry Service Annual Report Active complication (4) Total 200 66 15 7 6 7 ABI Low Risk (0) At Risk (1) At Risk (2) High Risk (3) Active Complication (4) Oct 64 26 3 1 6 Nov 49 24 2 0 1 Dec 45 17 2 1 2 Total 158 67 7 2 9 The above statistics have showed that majority of patients that are able to be screened using the Ankle Brachial Index are category 0 and 1, this provides an opportunity for patient education that aims to promote self-care and maintain good foot health. Patients that have been identified as category 2 and 3 have experienced changes to circulation and/or sensation. Therefore early detection and intervention at these stages can be highly effective at reducing the risk of further deterioration and complications, 13% of the patients seen in the clinic fall into this category. Service exit: Patients exit the service when the: Patient has declined the service Patient has missed two consecutive appointments. Patient has been identified as having ‘At Risk’ feet and their care is transferred on to the Manukau SuperClinic. When patients exit from the service they, and their primary care provider are informed by letter. CONCLUSION/REFLECTION The MCHT podiatry service has been running for over 12 months now and we are beginning to see some of our recall patients screened from the previous year. Most recalled patients have said they went away with the education given by the team and have started walking more, eating better and feel they have more energy now. In addition to the positive verbal feedback received from patients, we have also noticed improvements in various aspects of their diabetes management. Some patients have better feet now i.e. improved skin integrity. Many patients have improved their HbA1c levels and are getting closer to achieving the target range. MCHT podiatry and the team the Diabetes HUB will continue to re-evaluate our service to ensure we continue to provide optimal community-based podiatry care. Mangere Community Health Trust Podiatry Service Annual Report 8 Not Achieved KPI’s Partial Achieved Reduce the number of lower limb amputations within It is difficult to measure this outcome over such a short period; this will only the Counties Manukau district. become evident after a few years. Decrease hospital admissions for complications associated with diabetes foot-related Identify and educating High Risk patients It is difficult to measure this outcome over such a short period; this will only become evident after a few years. Achieved Provide a comprehensive assessment service Achieved Provide a free, appropriate and accessible service for Diabetic patients within the Mangere area Achieved Initiate preventive measures when necessary Achieved Provide podiatric management as appropriate Achieved Educate health professionals, patients, whanau, and members of the community in aspects of podiatry and diabetic foot pathology. Mangere Community Health Trust Podiatry Service Annual Report Achieved 9 APPENDIX 1: Case photos Mangere Community Health Trust Podiatry Service Annual Report 10 APPENDIX 2: CATEGORY OF REFERRALS Risk Category 0 Risk Levels Low Risk At Risk At Risk High Risk Active Foot Complication Definition No LOPS NO PAD No deformity No neuropathy ABI > 0.9 LOPS +/- deformity PAD +/ LOPS Hx of ulcer or amputation Active ulceration Charcot foot Neuropathy ABI > 0.9 Neuropathy ABI < 0.8 Neuropathy PAD Neuropathy PAD Absent Pedal pulses with possible symptoms of PAD Hx ulceration, Charcot joints, or amputation Active diabetic foot complication Same as category 1 Same as category 1 Consider vascular consultation if PAD present Multidisciplinary team management of foot complication Foot Presentation 2 3 4 (Secondary intervention) Pedal pulses palpable No deformity Treatment 1 Pedal palpable pulses Foot deformity with signs of pressure i.e callus/ corns. No Hx ulceration, Charcot joints, or amputation No Hx ulceration, Charcot joints, or amputation Patient education including advice on footwear. Consider prescription of accommodative footwear Consider prophylactic surgery if deformity is not able to be safely accommodated in shoes. Continue education Possible Hx vascular intervention of Foot deformity may be present. No Hx ulceration, Charcot joints, or amputation Consider prescriptive accommodative footwear Consider vascular consultation for combined followup Continue patient education Continue patient education patient Specialist wound care Consider vascular consultation if PAD present Consider surgery for foot deformity Suggested Follow-up Annual review with Get Checked screening Every 3 to 6 months (by specialist podiatrist) Every 2 to 3 months (by specialist podiatrist) Mangere Community Health Trust Podiatry Service Annual Report Every 1 to 2 months (by specialist podiatrist) Continue patient education As required until resolved 11 APPENDIX 3: Wagner Classification of Diabetic Foot Ulcers Grade 0: No ulcer in a high risk foot. Grade 1: Superficial ulcer involving the full skin thickness but not underlying tissues. Grade 2: Deep ulcer, penetrating down to ligaments and muscle, but no bone involvement or abscess formation. Grade 3: Deep ulcer with cellulitis or abscess formation, often with osteomyelitis. Grade 4: Localized gangrene. Grade 5: Extensive gangrene involving the whole foot APPENDIX 4: Chemical Matrixectomy Mangere Community Health Trust Podiatry Service Annual Report 12