File - PTA-2200 Fundamentals of Physical Therapy
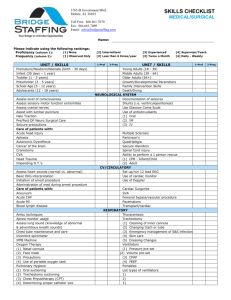
advertisement

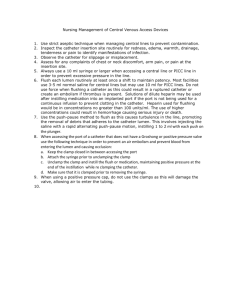
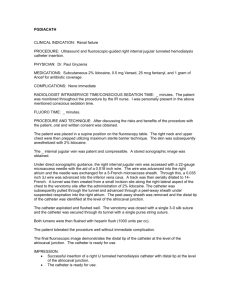
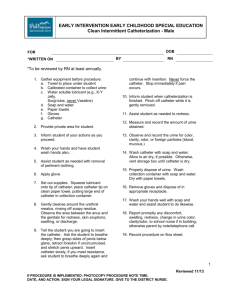
PTA 200 FUNDAMENTALS OF PHYSICAL THERAPY SPECIAL EQUIPMENT & THE ACUTE CARE SETTING Key Terms Dyspnea: Shortness of breath (SOB) Infiltrate: When fluid being administered through an IV leaks out of the vein into the subcutaneous tissues Intubate: When oxygen is being administered through an endotracheal tube the patient is “intubated” Key Terms Occlude: To close off or obstruct IV line or catheter Airway Specialized Care Units See text: Box 10-1 p 276 Orientation to Special Care Units Equipment to Monitor the patient’s physiologic state Vital signs Ventilate (ventilator or respirator) Provide intravenous (IV) therapy Deliver oxygen Remove fluids (suction, drains) Guidelines for Treating a Patient in an Intensive Care Unit Precautions to Use in the Intensive Care Unit see text Procedures 10-1 & 10-2 p 278 Precautions to Observe: Specific to PT Modify treatment to patient status Shorter treatment sessions Fewer repetitions Less active participation PT Goals & Activities in ICU Prevent contractures Passive & active ROM Positioning Body alignment Improve patient’s general condition Bed mobility training Transfer training Ambulation activities Increase functional independence Types of Beds (See Summary Handout) Standard adjustable bed Turning frame (Stryker Wedge frame) Circular turning frame Air-fluidized support bed (Clinitron) Post-trauma beds (Keane, Roto-Rest) Low air loss bed Life Support & Monitoring Equipment Mechanical Ventilators (Respirators) Use positive pressure to move or propel gas into patient’s lungs Gas is delivered through an endotracheal tube (ETT) When tube is in place, patient is intubated Patients are weaned from vents as they start to breath on their own Endotracheal Tubes Air will be induced into patient through a tube in one of several possible ways All will provide a clear airway into the lungs and allow for suction of secretions An ETT will restrict the patient from talking & once removed the patient is likely to complain of a sore throat and the voice may be distorted Life Support & Monitoring Equipment Endotracheal tube locations Oral pharyngeal Nasal pharyngeal Nasal endotracheal Oral endotracheal Tracheostomy Laryngostomy Types of Ventilators Volume-Cycled Ventilators For patients who require long-term ventilation COPD s/p thoracic surgery CNS disorders A predetermined volume of gas is delivered during inspiration dependent on patient’s need; expiration is passive Pressure-Cycled Ventilators Used for short-term ventilation Provides Intermittent Positive-Pressure Breathing (IPPB) Delivers a predetermined pressure of gas during inspiration; expiration is passive Negative Pressure Device Rarely used Includes iron lungs Create a negative pressure in the patient’s chest so air will enter the patient’s lungs Modes of Ventilation See Summary Handout & Box 10-2 p 283 Assist mode Continuous positive airway pressure (CPAP) Control mode Assisted control mode Intermittent mandatory ventilation (IMV) mode Synchronized IMV mode Positive end-expiratory pressure (PEEP) Precautions for Intubated Patients Be certain tubing is long enough for the activity Ask questions that can be answered with head nods or nonverbally Monitor patient closely Vital signs Respiratory distress Cardiopulmonary distress Patient may not tolerate exercise as well as other patients Monitors Exercise can be performed by patients on monitors provided care is taken not to disrupt the equipment See Summary handout & text p 284-286 Monitors Vital signs Arterial blood gases (ABGs) Intracranial pressure (ICP) Central venous pressure (CVP) Arterial pressure (A-line) Monitors for Vital Signs Blood pressure Respirations Temperature Blood gases Cardiac patterns EKG or ECG Telemetry Oximeter Pulmonary artery catheter (Swan-Ganz catheter) Intracranial pressure monitor (CP) Central venous pressure catheter (CVP) Arterial line (A line) Indwelling right atrial catheter (Hickman) Feeding Devices Nasogastric tube (NG tube) Gastric tube (G tube) Intravenous feeding Intravenous infusion lines (IV) Urinary Catheters External catheter (condom) Indwelling catheter inserted through urethra into bladder Foley catheter Catheter bag must remain below the level of the bladder Suprapubic catheter Oxygen Therapy Systems Nasal canula Oronasal mask Nasal catheter Tent Tracheostomy mask or catheter Chest Drainage Systems Ostomy devices Enterostomy Ileostomy Colostomy Skeletal Traction Balanced suspension traction Thomas splint Kirschner wires Skull traction: Crutchfield tongs Halo External fixation devices: Hoffman Internal fixation devices (ORIF) Patient-controlled analgesia (PAC) Dialysis Hemodialysis Peritoneal dialysis Laboratory Values O2Sat (SAO2) 95-98% Keep 90% when exercising Hemoglobin (Hgb) 14-18 g/dl (males) 13-16 g/dl (females) Hematocrit (Hct) 40-54 ml/dl (males) 37-48 ml/dl (females)