Anthrax - Columbia University
advertisement

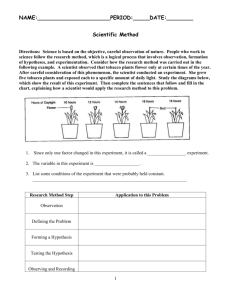
Bacillus anthracis Hirotaka Ishibashi Jennifer Jolivet Sean Patrick Kelly Bacillus anthracis Gram + rod Facultative anaerobe 1 - 1.2µm in width x 3 - 5µm in length Belongs to the B. cereus family – Thiamin growth requirement – Glutamyl-polypeptide capsule – Nonmotile Forms oval, centrally located endospores http://www.bact.wisc.edu/Bact330/lectureanthrax Endospore Oxygen required for sporulation 1 spore per cell dehydrated cells – Highly resistant to heat, cold, chemical disinfectants, dry periods Protoplast carries the material for future vegetative cell Cortex provides heat and radiation resistance Spore wall provides protection from chemicals & enzymes http://www.gsbs.utmb.edu/microbook/ch015.htm Genetics 1 chromosome – 5.2 million bp – Ames strain sequenced 2 plasmids – px01 184 kbp Pathogenicity island – pX02 95.3 kbp Capsule Anthrax receptor – Occurs > than ten thousendfold on macrophage cell – ATR/TEM8 gene Chromosome 4 gib.genes.nig.ac.jp/single/ main.php?spid=Bant_AME Where is Anthrax? http://www.vetmed.lsu.edu/whocc/mp_world.htm Anthrax From the Greek word anthrakos for coal Caused by spores Primarily a disease of domesticated & wild animals – Herbivores such as sheep, cows, horses, goats Natural reservoir is soil – Does not depend on an animal reservoir making it hard to eradicate – Cannot be regularly cultivated from soils where there is an absence of endemic anthrax – Occurs sporadically throughout US – South Dakota, Arkansas, Texas, Louisiana, Mississippi, California recognized endemic areas Anthrax zones – Soil rich in organic matter (pH < 6.0) – Dramatic changes in climate Anthrax Infection & Spread May be spread by streams, insects, wild animals, birds, contaminated wastes Animals infected by soilborne spores in food & water or bites from certain insects Humans can be infected when in contact with flesh, bones, hides, hair, & excrement – nonindustrial or industrial – cutaneous & inhalational most common Risk of natural infection 1/100,000 – Outbreaks occur in endemic areas after outbreaks in livestock Three forms of Anthrax Cutaneous anthrax – Skin – Most common – Spores enter to skin through small lesions Inhalation anthrax – Spores are inhaled Gastrointestinal (GI) anthrax – Spores are ingested – Oral-pharyngeal and abdominal Milestones in Anthrax History Early history 1800s 1900s Recent years Outbreaks in Thailand and US History of Anthrax (Early history) Although anthrax dates back more than 3,000 years, it was not recognized as a disease until the 18th century. 1500 B.C - A “plague of boils” in Egypt affected the Pharaoh’s cattle. ‘Boils’ are symptomatic of anthrax. 1600s - The “Black Bane” thought to be anthrax, in Europe kills over 60,000 cattle. 1700s - There are some accounts of human cases. History (1800s) Early 1800s - The first human cases of cutaneous anthrax in the US and UK were reported in men who contracted the disease after having been in contact with infected livestock. The disease was called Wool Sorter’s disease or Rag Picker’s disease because it affected workers in those trades. 1868 - Anthrax was observed under a microscope. 1876 - German bacteriologist Robert Koch confirmed bacterial origin of anthrax. History (Early 1900s) 1915 - German agents injected horses, mules, and cattle with anthrax during WWI. This was the first recorded use of anthrax as a biological weapon. 1937 - Japan started a biological warfare program in Manchuria, including tests involving anthrax. 1942 - UK demonstrated experiments using anthrax at Gruinard Island off the coast of Scotland. 1943 - United States began developing anthrax weapons. 1945 - In Iran an anthrax outbreak killed more than 1 million sheep. History (Late 1900s) 1950s and 60s - U.S. biological warfare program continues after WWII at Fort Detrick, Maryland 1969 - President Nixon ended United States' offensive biological weapons program, but defensive work still continues. 1970 - Anthrax vaccine for humans was approved by U.S. FDA. 1978-80 - The world's largest outbreak of human anthrax via insect vectors or contaminated meat struck Zimbabwe, Africa where more than 10,000 cases were recorded and over 180 people died. 1979 - In Soviet Union, aerosolized anthrax spores were released accidentally at a military facility, affecting 94 and killing 64 people. History (Recent years) 1991 - About 150,000 U.S. troops were vaccinated for anthrax in preparation for Gulf War. 1990-93 - The cult group, Aum Shinrikyo, released anthrax spores in Tokyo, fortunately no one was injured. On February 27, 2004, the leader of this group was given a sentence of death at a district court in Tokyo. 1995 - Iraq produced 8,500 liters of concentrated anthrax as part of the biological weapon program under Saddam Hussein’s administration. 2001 - Letters containing anthrax spores were mailed to many places in the US such as NBC, New York Times, and Media in Miami. In Florida, a man died after inhaling anthrax at the office. Outbreaks in Thailand This picture is 9 days after the onset of symptoms of oralpharyngeal anthrax. Thira Sirisanthana, Arthuer Brown, Anthrax of the Gastrointestinal Tract, Emerging Infectious Diseases, Vol. 8, 7, July 2002 1982 - In rural Northern Thailand, an outbreak of 52 cases of cutaneous anthrax and 24 cases of oralpharyngeal anthrax occurred. Oral-pharyngeal anthrax: an unusual manifestation of human infection with B. anthracis. 1987 - 14 cases of both oralpharyngeal and abdominal anthrax occurred. Caused by the consumption of contaminated water and buffalo meat. Outbreaks in the US In the early 1900’s approximately 130 cases occurred annually due to the following reasons. 1) Agricultural, farm workers exposed to infected animals 2) Processors exposed to infected animal products (hair, leather, wool, bone) 3) Laboratory workers contacted with anthrax spores 4) Civilians exposed to contaminated imported animal products These four are rare today. Natural Outbreaks in the U.S. (1951–2003) 60 in 1970 human vaccination started 4745 3938 2003 23 9 7 6 3 5 5 2 3 4 2 5 2 2 2 2 2 0 0 1 0 0 0 1 0 0 0 2 0 0 0 1 0 0 0 0 0 0 0 1 0 0 0 20 03 16 12 14 19 95 22 26 19 75 70 60 50 40 30 20 10 0 19 51 19 55 Human cases in 1957 animal vaccination started • N = 409 Year • 391 cases were cutaneous anthrax. • 18 cases were inhalation anthrax • GI anthrax has not been recognized yet • Since 1990 only 2 cases of cutaneous anthrax of naturally occurring infection have been reported. Anthrax Overview PPT, CDC, 2001 (http://www.cdc.gov/) Natural Outbreaks in North Dakota The highest occurrence of Anthrax outbreaks in the US 1989-1999 - 26 cases of infected livestock were reported. 2000 - 33 cases were reported during July-September. Total of 180 animals (beef cattle, horses, and bison) died and one person was infected with cutaneous anthrax. Roughly, cases appear every 2 years in North Dakota Pathogenesis The infectious dose of B. anthracis in humans by any route is not precisely known. – Rely on primate data – Minimum infection dose of ~ 1,000-8,000 spores – LD50 of 8,000-10,000 spores for inhalation Virulence depends on 2 factors – Capsule – 3 toxins http://www.kvarkadabra.net/index.html?/biologija/teksti/biolosko_orozje.htm Capsule Glycocalyx – Sticky, gelatinous polymer external to cell wall pX02 plasmid Made up of D-glutamic acid Non-toxic on its own Only encapsulated B. anthracis virulent Most important role during establishment of disease – Protects against phagocytosis & lysis during vegetative state http://textbookofbacteriology.net/BSRP.html Toxins pX01 plasmid AB model – Binding – Activating Protective antigen (PA), edema factor (EF) & lethal factor (LF) – Make up 50% of proteins in the organism Individually non-toxic – PA+LF lethal activity – EF+PA edema – EF+LF inactive – PA+LF+EF edema & necrosis; lethal http://www.rcsb.org/pdb/molecules/pdb28_1.html Toxins (2) Protective antigen (PA, 83kDa) – Pag gene – Binds to receptor & helps internalize other 2 proteins Edema factor (EF, 89 kDa) – Cya gene – Adenylate cyclase – Affects all cells Lethal factor (LF, 87 kDa) – Lef gene – More important virulence factor – Metalloprotease – Cleaves mitogen activated protein kinase kinsase (MAPKK) – Affects only macrophages http://www.ericse.org/anthrax/anthraxmicrographs.html Mechanism of Infection Anthrax spores enter body Germinate & multiple in lymph nodes PA, EF, LF excreted from bacteria PA binds to TEM8. PA nicked by protease furin – 20-kDa segment off leaving 63-kDa peptide – Heptamer forms EF and/or LF binds Complex internalized by endocytosis Acidification of endosome LF or EF crosses into cytosol via PA mediated ionconductive channels LF cleaves MAPKK 1 & 2 EF stimulates cAMP http://kugi.kribb.re.kr/KUGI/Pathways/BioCarta/anthraxPathway/ Outcome Do not understand exactly how symptoms occur EF converts ATP to cAMP – Increases cAMP levels over 1,000 fold – Impairs neutrophil function – Alters water homeostasis – Edema LF cleaves MAPKK at its N terminus – Disrupts pathways involved in cell growth & maturation – Increased synthesis of tumor necrosis factor-α & interleukin-1β – Macrophage lysis – More cells infected with bacteria & toxin – Septic shock & death Death probably results from high levels of bacteria secreting LF toxins in blood – At death, blood contains as many as 109 bacilli/ml (depending on the species) Regulators Bicarbonate or CO2 stimulates capsule and PA formation LF requires zinc ions EF requires calmodulin, a major intracellular calcium receptor Transcriptional regulator AcpA on pX02 controls expression of capsule atxA on pX01 is a positive regulator necessary for transcription of all 3 toxin genes Clinical Information Infection Symptoms (1st and 2nd phase) Three forms of Anthrax infection and their Pathology Diagnosis Infection of Anthrax The estimated number of naturally occurring human cases of anthrax in the world is 20,000 to 100,000 per year. Humans are infected through contact with infected animals and their products because of human intervention. Anthrax spores contaminate the ground when an affected animal dies and can live in the soil for many years. Anthrax can also be spread by eating undercooked meat from infected animals. Anthrax is NOT transmitted from person to person. Humans can be exposed but not be infected. What are the symptoms for anthrax? There are two phases of symptom. 1) Early phase - Many symptoms can occur within 7 days of infection 2) 2nd phase - Will hit hard, and usually occurs within 2 or 3 days after the early phase. - Early Phase Symptoms Fever (temperature > 100 degrees F) Chills or night sweats Headache, cough, chest discomfort, sore throat Joint stiffness, joint pain, muscle aches Shortness of breath Enlarged lymph nodes, nausea, loss of appetite, abdominal distress, vomiting, diarrhea Meningitis - 2nd Phase Symptoms Breathing problems, pneumonia Shock Swollen lymph glands Profuse sweating Cyanosis (skin turns blue) Death Three clinical forms of Anthrax 3 types of anthrax infection occur in humans: 1) Cutaneous 2) Inhalation 3) GI Cutaneous Anthrax http://science.howstuffworks.com/anthrax1.htm 95% of anthrax infections occur when the bacterium enters a cut or scratch on the skin due to handling of contaminated animal products or infected animals. May also be spread by biting insects that have fed on infected hosts. After the spore germinates in skin tissues, toxin production initially results in itchy bump that develops into a vesicle and then painless black ulcer. Cutaneous Anthrax (2) The most common naturally occurring form of anthrax. Ulcers are usually 1-3 cm in diameter. Incubation period: – Usually an immediate response up to 1 day Case fatality after 2 days of infection: – Untreated (20%) – With antimicrobial therapy (1%) Cutaneous Anthrax (3) CDC, Cutaneous Anthrax—Vesicle Development Inhalation Anthrax The infection begins with the inhalation of the anthrax spore. Spores need to be less than 5 microns (millionths of a meter) to reach the alveolus. Macrophages lyse and destroy some of the spores. Survived spores are transported to lymph nodes. At least 2,500 spores have to be inhaled to cause an infection. Inhalation Anthrax, Introduction, DRP, Armed Forces Institute of Pathology Inhalation Anthrax (2) Disease immediately follows germination. Spores replicate in the lymph nodes. The two lungs are separated by a structure called the mediastinum, which contains the heart, trachea, esophagus, and blood vessels. Bacterial toxins released during replication result in mediastinal widening and pleural effusions (accumulation of fluid in the pleural space). Inhalation Anthrax, Introduction, DRP, Armed Forces Institute of Pathology Inhalation Anthrax (3) Death usually results 2-3 days after the onset of symptoms. Natural infection is extremely rare (in the US, 20 cases were reported in last century). Inhalation Anthrax is the most lethal type of Anthrax. Incubation period: – 1–7 days – Possibly ranging up to 42 days (depending on how many spores were inhaled). Case fatality after 2 days of infection: – Untreated (97%) – With antimicrobial therapy (75%) Gastrointestinal Anthrax http://science.howstuffworks.com/anthrax1.htm GI anthrax may follow after the consumption of contaminated, poorly cooked meat. There are 2 different forms of GI anthrax: 1) Oral-pharyngeal 2) Abdominal Abdominal anthrax is more common than the oral-pharyngeal form. GI Anthrax (2) Oral-pharyngeal form - results from the deposition and germination of spores in the upper gastrointestinal tract. Local lumphadenopathy (an infection of the lymph glands and lymph channels), edema, sepsis develop after an oral or esophageal ulcer. Abdominal form - develops from the deposition and germination of spores in the lower gastrointestinal tract, which results in a primary intestinal lesion. Symptoms such as abdominal pain and vomiting appear within a few days after ingestion. GI Infection (3) GI anthrax cases are uncommon. There have been reported outbreaks in Zimbabwe, Africa and northern Thailand in the world. GI anthrax has not been reported in the US. Incubation period: – 1-7 days Case fatality at 2 days of infection: – Untreated (25-60%) – With antimicrobial therapy (undefined) due to the rarity How is anthrax diagnosed? Gram stain Culture of B. anthracis from the blood, skin lesions, vesicular fluid, or respiratory secretions X-ray and Computed Tomography (CT) scan Rapid detection methods - PCR for detection of nucleic acid - ELISA assay for antigen detection - Other immunohistochemical and immunoflourescence examinations - These are available only at certain labs Gram Stain Analysis Bacillus anthracis in Gram stain Useful for cutaneous and inhalation anthrax. A blood sample or skin lesion is taken from the patient and cultured for 6 to 24 hours. Gram stain takes about 10 to 15 minutes. Identify whether the bacteria come from the anthrax category. Chest X-ray At day 1 Useful for inhalation and GI anthrax Chest X-rays is advised as an initial method of inhalation anthrax detection, but it is sometimes not useful for patients without symptoms. Find a widened mediastinum and pleural effusion. Picture shows widened mediastinum caused by B. anthracis infection, resulting less available space in lungs At day 3 Inhalation Anthrax, Introduction, DRP, Armed Forces Institute of Pathology CT scan Useful for inhalation and GI anthrax Even when X-rays are negative, CT scans may provide more precise information. Chest CT (Right) shows the increase in the size of the pleural effusions (accumulation of fluid in the pleural space). Inhalation Anthrax, Introduction, DRP, Armed Forces Institute of Pathology PCR Assay PCR is a target amplification method of nucleic acid based B. anthracis detection. Used for the detection of anthrax toxin genes. ex) rpoB gene - used as a specific chromosomal marker for RT-PCR detection. The rpoB gene was sequenced from 36 Bacillus strains The assay was specific for 144 Bacillus anthracis strains from different geographical locations. Provided 100% sensitivity and specificity PCR Assay (2) Detection time: - PCR only takes several hours ex) Rapid-cycle RT-PCR can be finished within 1-2 hours Can start early treatment of Anthrax There are many different types of PCR assays for the detection of Anthrax such as multiplex PCR, enterobacterial repetitive intergenic consensus-PCR (ERIC-PCR), and longrange repetitive element polymorphism-PCR. Rapid diagnostic methods provide answers in minutes or hours instead of days. Distinguishing inhalation Anthrax from cold or influenza Anthrax, cold, and influenza patients have similar symptoms at early phase such as flu-like symptoms (fever, chills, cough, and muscle aches etc.) Symptoms of Anthrax do not include a runny nose, which is common in cold and influenza . Anthrax involves severe breathing problems and more vomiting. These symptoms are not very common in cold or influenza. Anthrax have high white blood cell counts and no increase in the number of lymphocytes. Flu usually have low white blood cell counts and an increase in the number of lymphocytes. Inhalation anthrax has abnormality in X-ray or CT scan Treatment Before 2001, 1st line of treatment was penicillin G – Stopped for fear of genetically engineered resistant strains 60 day course of antibiotics Ciprofloxacin – fluoroquinolone – 500 mg tablet every 12h or 400 mg IV every 12h – Inhibits DNA synthesis Doxycycline – 6-deoxy-tetracycline – 100 mg tablet every 12h or 100 mg IV every 12h – Inhibits protein synthesis For inhalational, need another antimicrobial agent – clindamycin – rifampin – chloramphenico http://nmhm.washingtondc.museum/news/anthrax.html Vaccine BioThrax/Anthrax vaccine absorbed – Made by Bioport – Route of exposure not important Administered subcutaneously – .5mL at 0, 2, and 4 weeks, and at 6, 12, & 18 months, & booster doses at 1 yr intervals PA from attenuated, nonencapsulated Sterne strain absorbed onto aluminum hydroxide – Contains no dead or live bacteria in the preparation – Antibodies to PA prevent binding to the target cell & confer protection from anthrax. 95% of vaccinated Rhesus monkeys survived lethal doses of inhaled anthrax A December 22, 2003 ruling temporarily halted the Department of Defense’s anthrax vaccination program – Lifting of that injunction on January 7, 2004 Who gets it? People who work directly with it in the lab People who work with imported animal hides or furs in areas where standards are insufficient to prevent exposure to anthrax spores. People who handle potentially infected animal products in high-incidence areas Military personnel deployed to areas with high risk for exposure to the organism. Continuing research Anthrax Immunity Gene in Mice – Kif1C – Four varieties (two resistant & two susceptible) Hepatitis drug – Hepsera – Blocks the toxic edema factor Monoclonal antibodies – ABthrax from Human Genome Science – Phase 1 clinical trials – Neutralizes protective antigen Identify other strains for improved, faster diagnosis Weaponization & Bacillus Anthracis: Why is this Agent Considered to be the Department of Defense’s Number-One/Two Biological Threat? A sample of anthrax bacteria at the National School of Biological Sciences, Mexico City Why are Biological Agents Attractive Weapons? Generally Less Expensive than Other WMD – The “Poor Man’s Nuke” – Equivalent lethal effect from nuclear weapon would cost approximately 800 times as much ($800 invested in NW for every $1 put toward BW) Dual Use - Is the Biological Material a Vaccine or Weapon? – Same equipment often used to produce both legal vaccines/ pharmaceuticals and BW – Perpetrator can deny agents were intended for use as BW – Helps to lower cost of BW facility if also involved in legal activity – Staff of trained professionals likely always available Why are Biological Agents Attractive Weapons? (2) Silent, Unnoticeable Attacks – Bombs & bullets are loud and there effects often dramatic and widely evident - not the case with BW – BW can be tasteless, odorless, colorless and unnoticeable – Allows for more facile attacks on large populations – People could be inflicted and not immediately realize it - time lag Why are Biological Agents Attractive Weapons? (3) Plausible Deniability – – State or terrorist group can easily deny deliverance Proof difficult to come by - 2001 anthrax terrorists still not found & likely never will be (very little evidence) – DNA sequencing of biological agent and matching it with an agent in the assumed perpetrator’s possession likely the only way to locate attacker even sequencing is speculative VS. Why are Biological Agents Attractive Weapons? (4) Lengthy Incubation Period – Most weapons act immediately, not usually the case with BW – Various BW agents have incubation periods of 1-60 days on average – Can surprise opposition/victims and put them in “survival” mode rather than defense mode ==> greater vulnerability – No way of knowing where to heighten security, often impossible to trace BW origin Specific Benefits of Using Anthrax as a Biological Weapon Highly Lethal (Inhalational Anthrax) – Virtually 100% of exposed personnel will die from one breath of air with a high anthrax concentration (LD50 determined to be about 8,000-10,000 spores or .08-.5 micrograms) – Inhalation of about 1,000 spores (.01g) can cause pulmonary anthrax – 100,000 times deadlier than the deadliest chemical warfare agent – If treatment begins 48 hrs after symptoms, mortality still ~95% Specific Benefits of Using Anthrax as a Biological Weapon (2) Non-contagious – Eliminates concern of spread from one person to another (sheep different) – Allows for anthrax to be targeted at specific populations w/o worry – In contrast, Smallpox and pneumonic plague are communicable Easy to Protect with Advance Preparation – Enemy could vaccinate troops prior to an attack and/or antibiotics could be provided in order to mitigate disease’s effects – Physical and psychological advantage for attacker - no harm in entering contaminated zone Specific Benefits of Using Anthrax as a Biological Weapon (3) Long Shelf Life – Anthrax spores decay at a rate of less than one tenth of a percent per minute (very slow for an organism) – During WW II, Britain detonated experimental anthrax bombs on Gruinard Island - anthrax spores remained viable in top 15-20cm of soil for ~40 yrs until fully decontaminated in 1986 Anthrax is Stable in Many Various Types of Weapons Systems – Withstands the turbulence experienced from being sprayed/detonated – Can be loaded in munitions (freeze-dried condition) , disseminated as an aerosol with crude sprayers or even packaged in milled or un-milled powder form (ex. envelopes through mail) Specific Benefits of Using Anthrax as a Biological Weapon (4) Short Incubation Period (Relative to Most Other BW) – Lag-time between attack and the first symptoms is only 1-6 days – Prediction of intended effect is much more facile to estimate – In contrast, bacterial agent brucellosis has an incubation of 5-60 days UV Resistant – One of only two bacterial agents that is considered resistant to sunlight (the other being Coxiella) Specific Benefits of Using Anthrax as a Biological Weapon (5) Widely Available – Animal disease - soil samples from all over the world contain anthrax – Approx. 1500 microbiologic repositories across the globe sell cultures to laboratories, vaccine companies and other entities (diagnostic/treatment) Facile to Produce in Basic Form – Knowledge/technology available in open market with few controls – Cost is low (approximately $50 per kilogram in basic from) – One test tube of feed stock (samples of anthrax) in a fermenter can produce a kg of anthrax in about 96 hours – Any country with basic healthcare/pharmaceutical industry can produce Specific Benefits of Using Anthrax as a Biological Weapon (6) Spores Naturally Occurring at 1-5 m – Optimal size for BW agent b/c it is right diameter to get to the bottom of the alveoli in the lungs - if too big, spores will stick to top of lung and will likely get blown back out Anthrax Dangerous as Both a Powder and Liquid – Enhances perpetrator’s delivery options Only Need a Small Amount for a Mass Effect – 1,763 lbs of nerve gas sarin, .2 lbs of Type A botulinum toxin or only .02 lbs of anthrax spores produce the same lethal effect Locating the Threat of Anthrax: Who Has Weapons? Exact # of Countries & Terrorist Groups Unknown – Intuitively, it would seem that any country/terrorist group that has an offensive BW program also has anthrax – Any country/terrorist group with biotech/pharmaceutical corporations and/or facilities could easily make anthrax – United States and Russia are only countries confirmed to currently be in possession of weaponized anthrax – Many other nations and terrorist groups believed to have anthrax Locating the Threat of Anthrax: Who Has Weapons? (2) Determining the Most Significant Threats – US Department of Defense: “More than seven countries including Iraq, Iran, Syria & Russia have or are suspected of developing (anthrax) biological warfare capability”1 – US, Britain, Iraq, Germany, the USSR, Japan, South Africa & Aum Shinrikyo (Japanese terrorist group) have used/tested anthrax as a weapon in the past - what state/group was responsible for 2001 attacks? – US Department of State has identified seven states as sponsors of international terrorism: Iran, Iraq, Syria, Libya, Cuba, Sudan & North Korea 1 - “DoD Response to the Staff Report of the House Government Reform’s Subcommittee on National Security,” 1, 2; and “Information about the Anthrax Vaccine,” 2. Locating the Threat of Anthrax: Who Has Weapons? (3) Determining the Most Significant Threats (continued) – Secretary of the Air Force F. Whitten Peters to Senate Armed Services Committee on 07/21/99: “[Anthrax] has been weapon-ized and we know it is deployed in about 10 countries around the world.” 1 – During the 1980s, some of the Soviet Union’s intercontinental ballistic missiles (ICBM) reportedly were loaded with “cocktails” of BW agents (including anthrax) and targeted at major US cities (One ICBM could carry enough anthrax to wipe out the population of NYC). 2 1 - Peter Grier, “Up in the Air about Anthrax,” Air Force Magazine 82, no. 10 (October 1999): 68–71. 2 - Atlas, 160; and Raymond A. Zilinskas, “Verifying Compliance to the Biological and Toxin Weapons Convention,” Critical Issues in Microbiology 24, no. 3 (1998): 195–218. Locating the Threat of Anthrax: Who Has Weapons? (4) Determining the Most Significant Threats (continued) – 1991/92 UN Special Commission (UNSCOM) inspection: Iraq definitely has BW, including anthrax – In 1995, Lt General Hussein Kamal (Saddam's Son-inlaw & former head of Iraqi BW program) told UN that: Iraq indeed had large stores of weaponizable anthrax and many weapons loaded with anthrax (bombs, Scuds, Al Hussayn warheads, 122 mm rockets, artillery shells, spray tanks for fighters and remotely piloted aircraft) 1 – Iraq was able to hide much of its BW program in spite of the intense UNSCOM inspections - could other countries as well? 1 - Zilinskas, “Verifying Compliance,” 195–218; and Rolf Ekéus, “UN biological Inspections in Iraq,” in The New Terror: Facing the Threat of Biological and Chemical Weapons, 246–47. Locating the Threat of Anthrax: Who Has Weapons? (5) BW Programs by Country & Sources of Information Country ACDA DOD ( 1995-97) (1996-98) Bulgaria China Cuba Egypt India Iran Iraq Israel Laos Libya North Korea Russia/Soviet Union South Africa Syria Taiwan Vietnam X X X X X X X X X X X X X X X FIS (1993) X X X X X DOD Open Sources (1988-90) (Pre-1993) X X X X X X X X X X X X X X X X X X X X X X X X X X ACDA = Arms Control & Disarmament Agency DOD = Department of Defense = Foreign Intelligence Service of the Russian Federation W. Seth Carus, “Biological Warfare Threats in Perspective,” Critical Issues in Microbiology 24, no. 3 (1998): 154. FIS Source: Weaponizing Anthrax: How is it made? What Type of Anthrax to Use? – Inhalational (lungs) Incredibly Lethal (untreated death rate >90%) Facile attack methods (silent, flu-like, spray dispersible, etc.) – Cutaneous (skin) Not near as lethal (untreated death rate ~20%) More difficult to administer (need cut or abrasion) – Gastrointestinal (intestines) Somewhat lethal (untreated death rate ~25-60%) More difficult to administer (one has to consume anthrax) Best Type of Anthrax for Use as Weapon: INHALATIONAL Weaponizing Anthrax: How is it made? (2) Simplistic Approach: – Grow bacteria culture (germination => vegetation, in vitro @37º C) – Allow bacteria to sporulate, separate by filtration or centrifugation – Weaponize - what type of dispersal? Wet dispersal – Spray liquid solution (droplets) over enemy Dry dispersal – Dry with drying agent (ex. Magnesium Sulfate) = powder – Aerosolize and spray over targeted population – Disperse in mail or by some other means But is it this easy? Answer: NO Weaponizing Anthrax: How is it made? (3) Wet Dispersal – Very difficult to formulate for effective use When solution is sprayed, droplets tend to be large (ex. Windex forms droplets ~100m in size) Droplets do not stay in air for long Would need jet aircraft flying at 600mph or special high pressure sprayers that cost ~$100,000 and would have to be mounted on a truck Not practical Solution: Use Dry Powder Weaponizing Anthrax: How is it made? (4) Dry Dispersal – More facile, but not necessarily a walk in the park… After spore formation & filtration/centrifugation, spores & remaining cells will form sticky paste (consistency of peanut butter) Paste dried down ==> forms brick (or freeze dried) Brick needs to be ground into fine (1 m) powder ==> spores will have surface charge ==> clumping Need to neutralize “static cling” (similar to putting a sheet of Bounce in dryer) Weaponizing Anthrax: How is it made? (5) Neutralizing “Static Cling” of Spores – Exact formulations and recipes are classified Basic approach is to coat spores with a fine silica or alumina clay (Iraqi’s use the chemical Bentonite) Spores no longer clump, actually want to stay apart, repel each other ==> do not stick to surfaces Without surface charges, spores can easily reaerosolize after coming in contact with objects/ground Treated area can be infectious for a long time after dispersal (Increases danger and lethality of BW) Weaponizing Anthrax: How is it made? (6) How to Aerosolize? – Once anthrax is weapons-grade (appropriate size and w/o surface charges), can simply be dispersed by basic spray methods (such as a crop-duster plane) The True Danger: Possible Effects Anthrax Attack World Health Organization (WHO) – Estimates that 250,000 people would develop disease and 100,000 would die if 50kg of aerosolized anthrax was released from an aircraft over a developed urban population of five million (w/o treatment).1 US Congressional Office of Technology Assessment – Estimates that between 130,000 and 3 million deaths could follow the aerosolized release of 100 kg of anthrax spores upwind of the Washington, DC, area—lethality matching or exceeding that of a hydrogen bomb.2 1 - World Health Organization. Health Aspects of Chemical and Biological Weapons. Geneva, Switzerland: World Health Organization; 1970:98-99. 2 - Office of Technology Assessment, US Congress. Proliferation of Weapons of Mass Destruction. Washington, DC: US Government Printing Office; 1993:53-55. Publication OTA-ISC-559. The True Danger: Possible Effects Anthrax Attack (2) Centers for Disease Control and Prevention (CDC) – Produced an economic model that suggested a cost of $26.2 billion per 100,000 persons exposed to inhalational anthrax 1 Decontamination of Gruinard Island in the UK – Decontamination took place from 1979 to 1987 – Total cost is unpublished (assumed to be ~500,000 British pounds), but materials required included 280 tons of formaldehyde & 2000 tons of seawater 2 – Decontamination of buildings/other areas equally as costly/difficult 1 - Kaufmann AF, Meltzer MI, Schmid GP. The economic impact of a bioterrorist attack. Emerg Infect Dis. 1997;3:83-94. 2 - Titball RW, Turnbull PC, Hutson RA. The monitoring and detection of Bacillus anthracis in the environment. J Appl Bacteriol. 1991;70(suppl):9S-18S. The True Danger: Possible Effects Anthrax Attack (3) Sverdlovsk Accident (Russia BW Plant) - New cases of inhalational anthrax developed as late as 43 days after the presumed date of release (lengthy period of lethality) Guillermin J. Anthrax: The Investigation of a Lethal Outbreak. Berkeley: University of California Press. In press. The True Danger: Possible Effects Anthrax Attack (4) Peters, C.J., D.M. Hartley. Anthrax Inhalation and Lethal Human Infection. Lancet. 359 (9307): 710-711. Analysis of the 2001 US Anthrax Attacks Period From 10/02/01 - 11/20/01 – 22 cases of anthrax infection, 11 inhalational (all confirmed) and 11 cutaneous (4 suspected & 7 confirmed) – 7 states : CT(1), FL(2), MD(3), NJ(5), NYC(8), PA(1) & VA(2) – 5 of 11 inhalational infections resulted in death (~45% mortality rate) – All persons received immediate treatment upon onset of symptoms – Mean duration between exposure and onset of symptoms: 4.5 days (estimate) Analysis of the 2001 US Anthrax Attacks (2) Above anthrax-containing envelopes postmarked September 18th, 2001 Above anthrax-containing envelopes postmarked October 9, 2001 *Also believed to be three or more other envelopes that were never found Analysis of the 2001 US Anthrax Attacks (3) http://www.anthraxinvestigation.com/ Analysis of the 2001 US Anthrax Attacks (4) Anthrax in Envelopes – Concentration of about 1 trillion spores per gram – 2 grams anthrax per envelope – Each letter contained ~200 million times average LD50 – All anthrax was unmilled, contained a certain type of silica to reduce electrostatic charges and was of the Ames strain – all characteristic of US weapons-grade anthrax Analysis of the 2001 US Anthrax Attacks (5) Anthrax Found at American Media Inc. Building (Florida) – No letters found, but anthrax isolated in 90 different locations in the building – Estimated cost of cleanup: $7 million Anthrax Found at Hart Senate Office (Washington D.C.) – 628 persons tested for bacillus anthracis, 28 found positive – Cleanup took three months and cost an estimated $23 million (with chlorine dioxide liquid) 4 Envelopes Processed at Two Facilities - NYC & Trenton – Both facilities tested positive for bacillus anthracis as well as at least 5 other facilities associated with Trenton facility Analysis of the 2001 US Anthrax Attacks (6) What Did These Attacks Exemplify? – Lethality of anthrax: 5 of 11 inhalatory victims died (though provided with best possible treatment), less than 2 grams of anthrax per envelope – Facile spread of weaponized anthrax: 7 states affected and only 4 letters found, rapid spread in buildings – Long shelf-life of anthrax: some people in NYC were affected weeks after others (varying incubation periods?) – Incredibly high cost of clean-up/decontamination: millions of $ – Difficulty of finding perpetrator: still not found, likely never will be Analysis of the 2001 US Anthrax Attacks (7) Concerns Resulting from 2001 Attacks – What would have happened if more people were affected? Would the mortality rate have been higher? – Who created this weapons-grade anthrax? Terrorist group thought to be unlikely, but then what state sponsor? Did US lab employee(s) or government official(s) lend a hand to perpetrators? – How can the US prevent other similar attacks? – What would have happened if anthrax would have been aerosolized? Defense: Protection Against Anthrax Vaccination – Very Effective: 2 dose efficacy against up to 1,000 LD50 in monkeys (human response believed to be very similar) Early Detection – Extremely important: How can the US learn about an anthrax attack before the appearance of symptoms? (would eliminate much of danger) – Time lag between exposure and symptoms is primary reason for the high mortality rate experienced with anthrax infections – A device similar to a smoke alarm or carbon monoxide detector? – Currently nothing on the market that could serve such a purpose, little research in this particular area Defense: Protection Against Anthrax (2) Air Cleansers/Filters – Simply a reduction of risk, by no means an elimination – Appropriate for mailrooms, wool-sorting facilities, etc. Irradiation of Susceptible Materials – Virtually eliminates threat of anthrax in mail – But is it worth it? Do the disadvantages outweigh the benefits? – Important Question: To what point are we willing to protect ourselves from anthrax threat? What are we willing to sacrifice? Defense: Protection Against Anthrax (3) Pre/Post Exposure Antibiotic Treatment – Isolates from the 2001 US attacks were sensitive to fluoroquinolones – Quite effective in mitigating effects of anthrax if caught at early stage Decontamination of Exposed Areas – Often costly & timely, but can be done rather successfully (using liquid chlorine dioxide or some other disinfectant) Use of Protective Clothing & Equipment – US military M17 & M40 gas masks provide good protection against 1-5 m particles (cost ~$325) – Protective suits can be worn to easily eliminate cutaneous threat Defense: Protection Against Anthrax (4) Only Reactionary, Post-Exposure Protection Methods Exist! – Besides vaccination/antibiotic treatment, there is no other preventative methods of protecting against anthrax – Most methods of protection are reactionary, this doesn’t help to solve the main problem: anthrax infections need to be determined earlier, before onset of symptoms – How can we currently protect ourselves from a massive bioterrorist attack? How can we make it more facile to distinguish btw. common maladies and anthrax? PRIMARY OBJECTIVE: NEED DEVICE/METHOD THAT WILL HELP TO PROTECT LARGE POPULATION FROM LARGE-SCALE ANTHRAX ATTACK Anthrax: Why it May Not be as Big of a Threat as People Think LD50 for Anthrax is Quite High – Smallpox: 10-100 organisms, Q Fever: 1-10organisms, etc. Very Difficult to Weaponize (Need State/Gov’t Support) – Aum Shinrikyo has failed to aerosolize anthrax on several occasions – Need sufficient nanotechnology engineering to be able to keep spores from clumping and sticking to surfaces (Army scientists could not weaponize anthrax when given the equipment a BW terrorist would likely have in his/her home) Even if have Technology, Weapons-Grade Anthrax Very Costly – Only US & Russia known to definitely have weaponized anthrax, large-scale production requires multi-million dollar investment Anthrax: Why it May Not be as Big of a Threat as People Think (2) Anthrax Strains are Highly Specific – Only certain strains are effective against humans, some are harmless Lengthy Incubation – While this is also an advantage, it can serve as a disadvantage – Don’t immediately know if weapon has “struck target” Difficult to Use Anthrax Against Precise Targets – 2001 US attacks: directed against high-status people, never reached targets – Aerosolization is most deadly, but also the most difficult to direct as a result of environmental conditions Anthrax vs. Other BW Agents: Brief Overview Disease Inhalation anthrax Brucellosis Trans mit Man to Man No No Infective Dose (Aerosol) 8,000-50,000 spores 10 -100 organisms Incubation Period 1-6 days Duration of Illness Per sistence of Organism Vaccine Efficacy (ae rosol e xpos ure) 2 dose ef ficacy against up to 1,000 LD50 in monkeys No vaccine <5% untreated Very stable - spores remain viable for > 40 years in soil Very stable > 1 week Low with treatment, high without Unstable in aerosols & f resh water; stable in salt water No data on aerosol Death in 7-10 days in septicemic f orm 1-6 days (usually f atal) > 50% Very stable No vaccine High unless treated within 12-24 hours For up to 1 year in soil; 270 days in live tissue 2-10 days (average 3-5) 10-40 days > 2 weeks 2-14 days Moderate if untreated Very low For months in moist soil or other media For months on wood and sand 3 doses not protective against 118 LD50 in monkeys 80% protection against 1-10 LD50 94% protection against 3,500 LD50 in guinea pigs Vaccine protects against large doses in primates 5-60 days (usually 1-2 months) 4 hours 5 days (usually 2-3 days) 10-14 days via aerosol 2-3 days 3-5 days (usually fatal if untreated) Weeks to months Le thality (approx. cas e fatality rates) High Chole ra Rare 10-500 organisms Glanders Low Assumed low Pneumonic Plague High 100-500 organisms Tulare mia No 10-50 organisms Q Fe ver Rare 1-10 organisms Smallpox High 7-17 days (average 12) 4 weeks High to moderate Very stable Vene zue lan Equine Ence phalitis Viral Hemorrhagic Fevers Botulism Low Assumed low (10-100 organisms) 10-100 organisms 2-6 days Days to weeks Low Relatively unstable TC 83 protects against 30500 LD50 in hamsters Moderate 1-10 organisms 4-21 days Death between 7-16 days Relatively unstable - depends on agent No vaccine No 0.001 g/kg is LD50 for type A 1-5 days For weeks in nonmoving water and food Staph Enterotoxin B Ricin No 0.03 g/person incapacitation 3-5 g/kg is L D50 in mice 3-12 hours after inhalation 18-24 hours Death in 24-72 hours; lasts months if not lethal Hours High for Zaire strain, moderate with Sudan High without respiratory support < 1% Resistant to f reezing 3 dose ef ficacy 100% against 25-250 LD50 in primates No vaccine High Stable No vaccine T-2 Mycotoxins No Moderate 2-4 hours Moderate For years at room temperature No vaccine No Days - death within 10-12 days for ingestion Days to months www.nbc-med.org/SiteContent/HomePage/ WhatsNew/MedManual/Feb01/AppxC.doc - http://www.sumanasinc.com/webcontent/ anisamples/ani_anthrax.html http://www.bt.cdc.gov/training/historyofbt /index.asp