2015-3-6-TINU-Shivani-Reddy
advertisement

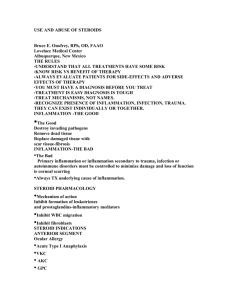
Grand Rounds Shivani V. Reddy, M.D. 3/6/2014 University of Louisville Department of Ophthalmology and Visual Sciences Patient Presentation CC: blurry vision OU HPI: 12 year old white male presents with 1 week history of blurry vision OU. He denies any pain, photophobia, flashes or scotomas. He had a similar episode 4 months prior with associated pain and photophobia. Patient denies any associated malaise, nausea or flank pain during these episodes. History POHx and PMHx 1 year ago: patient presented to KCH with fever, malaise, flank pain and 2 weeks of frothy urine renal biopsy: tubular interstitial nephritis treatment: prednisone 40 mg daily 4 months ago: patient developed blurry vision OU with pain and photophobia – diagnosed with acute anterior uveitis treatment: topical Pred Forte, Cyclogyl 12 week course of methotrexate FAM Hx none ROS cushingoid features MEDS prednisone 20 mg QOD, Cellcept 500mg PO BID ALLERGIES NKDA Exam 4 3 mm 20/20-3 ( -0.75 + 1.00 x 015) VA cc 20/20 (-1.50 + 0.25 x 165) EOM: Full OU CVF: Full OU P no RAPD 4 3 mm 16 TTP 16 Anterior Segment OD Ext L/L C/S K AC I/L OS WNL WNL WNL WNL 1+ injection 1+ injection few fine KP WNL 2+Cell, 1+ Flare 1+ Cell, 1+ Flare posterior synechiae posterior synechiae NO VITREOUS CELLS OU Fundus Exam OD 2 + disc edema, normal macula, normal vessels multiple choroidal inflammatory foci on peripheral exam Fundus Exam 1 + disc edema with mild peripapillary NFL edema, normal macula, normal vessels. Multiple choroidal inflammatory foci (arrows) OCT OD mild ILM gliosis, normal foveal contour OS normal foveal contour FA/ICG 29 seconds: few areas of choroidal leakage on ICG FA/ICG 54 seconds: foci of choroidal hypofluorescence on ICG Summary 12 y/o WM with h/o tubular interstitial nephritis diagnosed 1 year prior and an episode of bilateral anterior uveitis 4 months prior presents with blurry vision OU while taking oral prednisone and Cellcept. Exam reveals anterior uveitis , optic disc edema and multiple foci of outer retinal and choroidal inflammation OD > OS. DDx: • TINU syndrome (tubular interstitial nephritis and uveitis) • Infectious mononucleosis • Sarcoidosis • Other Infections (syphilis, herpesviridae) • Systemic lupus erythematosus Treatment Given patient’s cushingoid features and long term prednisone use, prednisone dose was decreased to 10 mg every other day and Cellcept was increased to 1.5 gm daily Follow-up pending TINU Syndrome A predominantly bilateral non-granulomatous anterior uveitis found in a subset of patients with tubular interstitial nephritis (TIN) First described in 1975 by Dobrin et.al. relatively rare with reported incidence 1-2% Uveitis occurs in approximately 65% of TIN patients TINU Syndrome Epidemiology - young females (teens – 30) - younger age groups with more male patients No racial affinity Some HLA associations with HLA-DQA1*01, HLA-DQB1*01 HLA-DQB1*05 TINU Syndrome Pathogenesis not well understood Autoantigen to both uveal and renal tubular cells (mCRP) Inflammation is T- lymphocyte driven Risk factors found in only 50% - antibiotics for URIs, NSAIDS, autoimmune diseases, Chlamydia and EBV concurrent infection Ocular Symptoms Patients present with anterior uveitis symptoms (pain, redness, photophobia, decreased vision) Other findings: optic nerve edema, retinal infiltrates, vitreous opacities ocular symptoms follow TIN in 65%, are concurrent in 15%, precede by up to 2 months in 20% TIN Findings Increased serum creatinine Abnormal urinalysis ( no definitive markers) - increased B2- microglobulin - urinary eosinophilia, pyuria, hematuria - glucosuria Renal biopsy for definitive diagnosis - Interstitial edema, mononuclear infiltrate, eosinophils and noncaseating granulomas Interstitial edema, mononuclear infiltrate, eosinophils and noncaseating granulomas Treatment renal disease very responsive to corticosteroids typically treated for 3 to 6 months with slow taper Uveitis treated with corticosteroids (topical and systemic) Even though TIN typically is self limited, uveitis can be recurrent requiring immunomodulator therapy (IMT) • mycophenolate mofetil , methotrexate, cyclosporine Prognosis Long term complication are rare Uveitis often persists longer than TIN but treatment rarely lasts over 1 year Uveitis recurs in up to 40% of patients within a few months of therapy cessation but nephritis rarely recurs retrospective case series of 4 patients with TINU Gender: 3 female, 1 male Age range: 10 -31 years All patients presented with acute anterior uveitis. 3/4 patients with vitritis 2 patients presented with TIN before uveitic symptoms: Pt 1 – 4 months prior, Pt 2 - 3 years prior. 2 patients presented with TIN concurrent with uveitic symptoms 10 year old caucasian female presenting with blurred vision, floaters. Elevated ESR, creatinine. Anterior uveitis, vitritis and lesions seen below 11 year old half- asian male with concurrent TIN and pain, redness and photophobia. Elevated creatinine. Exam with anterior uveitis, vitritis and punctate chorioretinal lesion 31 year old caucasion female with pain, redness, photophobia and floaters. Elevated creatinine. Exam with anterior uveitis, vitritis chorioretinal lesions References 1. 2. 3. 4. 5. 6. 7. 8. 9. BSCS Section 9: Intraocular Inflammation and Uveitis BSCS Section 12: Retina and Vitreous Mandeville et al. The tubulointerstitial nephritis and uveitis syndrome.Surv Ophth. 2001,46(3):195-208. Suzuki H, Yoshioka K, Miyano M, et al. Tubulointerstitial nephritis and uveitis (TINU) syndrome caused by the Chinese herb "Goreisan". Clin Exp Nephrol 2009; 13:73. Mackensen et al Br J Ophth. 2011,95:971-976. Birnbaum, et. al. Arch Ophthalmol. 2012;130(11):1389-1394. Mandeville JT, Levinson RD, Holland GN. The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol 2001; 46:195. Reddy et al. HLA-DR, DQ class II DNA typing in pediatric panuveitis and tubulointerstitial nephritis and uveitis. Am J Ophthalmol. 2014 Mar;157(3):678-86 Ali A, Rosenbaum JT. TINU (tubulointerstitial nephritis uveitis) can be associated with chorioretinal scars.Ocul Immunol Inflamm. 2014 Jun;22(3):213-7.