Teens and Contraception: New Approaches
advertisement

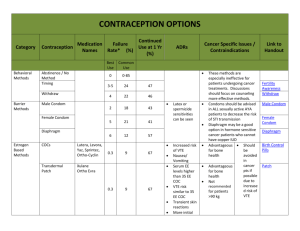
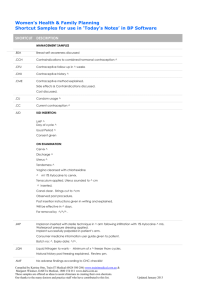
Teens and Contraception: New Approaches for Improved Compliance and Decreasing Teen Pregnancy Jennie Yoost MD, MSc Assistant Professor Pediatric and Adolescent Gynecology Marshall University Department of OBGYN LEARNING OBJECTIVES Understand the mechanism of action and safety profile of different long acting reversible contraceptives including the subdermal implant and levonorgestrel intrauterine devices. Understand the spectrum of contraceptives available and continuation rates of different methods among teenage users. Understand the noncontraceptive benefits to using different methods of contraception. Understand use, access, and mechanism of action of Emergency Contraception. Case #1 14 year old female presents with her mom. She started menses age 11. Mom is interested in discussing birth control. The girl is not sexually active. Mom feels she “has a good head on her shoulders” and makes good decisions. She worries about some of her friends, and wants her started on birth control “just in case”. Case #2 15 year old female presents for vaginal discharge. She has been sexually active since age 12, and has had a total of 6 partners since that time. She took birth control pills for a few months, but not using anything at this time. Pregnancy test is negative in the office. You ask if she is interested in birth control. She reports that she is, but “just has a hard time remembering it.” What do you offer her? WHAT ARE OPTIONS FOR TEENS? SAME OPTIONS AS ADULTS! Pills Patch Ring Injection Intrauterine Device Subdermal Implant Abstinence: It is important. It is encouraged. It can be secondary. It only works if you are abstinent Are teens really “doin’ it”? Youth Risk Behavioral Survey 2011 45.6% sexually active 4% report sexual debut before age of 13. (7% among AA) 13% > 4 sexual partners 53% report condom use 22.6% OCP use 7.5% other methods The problem of unintended pregnancy 6.7 million pregnancies per year in the US 50% are unintended Among 15-19 year olds: 82% unintended 2010 US adolescent birth rate 34.2/1000 2007 US adolescent birth rate 42.5/1000 How do we compare to the rest of the world? Variations within the US: among states (2010) GOOD: New Hamp 15.7 Massachusetts 17.2 Vermont 17.9 BAD: Texas 52.2 Arkansas 52.5 New Mexico 53 Mississippi 55 WV (44.8) #43 Teens and birth control compliance: METHOD USE FAILURE: Perfect Use FAILURE: Typical Use Continuation at 12 months Pills Take one pill daily 0.3% 9% 33-52% Patch Place one patch weekly 0.3% 9% 25-50% Ring Place one ring 0.3% monthly 9% 31%* Injection by 0.2% health provider Pills are overall the every 3 teens.months 6% 27-55% Injection • most common choice for • 50% of adolescents report missed pills during a given cycle What is a LARC? Long Acting Reversible Contraception Intrauterine Device Progesterone containing (Mirena®, Skyla®) Copper T (Paragard®) Subdermal Implant Nexplanon® LARCs- a good option for teens! Copper IUD Paragard® No hormones Effective for up to 10 years Placed by a simple procedure Can be done under sedation Mechanism of Action Copper ions inhibit sperm motility Inhibition of sperm capacitation (ability of sperm to fertilize an ovum) Sterile inflammatory reaction of endometrium (phagocytosis of sperm) May cause increased menstrual bleeding LARCs- a good option for teens! Levonorgestrel IUDs Mirena® 20mcg/day levonorgestrel Lasts 5 years Skyla® 14mcg/day levonorgestrel Lasts 3 years Smaller dimensions Placed by a simple procedure Can be done under sedation Mechanism of Action Increased cervical mucous Decreased tubal motility/ change in tubal fluid Alteration of endometrium Ovulatory inhibition Levonorgestrel IUDs Noncontraceptive Benefits Contraindications Decreased menstrual bleeding Active PID or puerperal or postabortion sepsis Amenorrhea Current STDs Improved dysmenorrhea Undiagnosed vaginal bleeding Malignancy of genital tract Known uterine anomaly or distortion of uterine cavity Local action No medication interaction Use in girls with medical comorbidities Pregnant (too late!) LARCS- a good option for teens! Subdermal Implant Nexplanon™ 68mg etonogestrel Single rod Effective for at least 3 years Procedure Inserted subdermally in groove just below biceps Can be placed at initial visit Mechanism of Action Ovulation inhibition Increased cervical mucous Endometrial atrophy Nexplanon® LARCs- a good option for teens! METHOD Levonorgestrel IUD Subdermal Implant FAILURE: Perfect Use 0.2% FAILURE: Typical Use 0.2% 0.05% 0.05% Don’t Believe Me? ACOG: “top tier methods of contraception including IUDs and implants should be considered as first line choices for adolescents” CDC/WHO: • Subdermal implants= Category I “no restriction” • IUD=Category II “advantages outweigh theoretically or proven risk” “But my friend’s sister’s friend told me that…….” Lets Look at the Data: Pregnancy Compliance/ Continuation Satisfaction Bleeding patterns Risks CHOICE study- prospective cohort (St. Louis, Aug 2007-Sept 2011) 9256 patients Risk of pregnancy: Pill/patch/ring= 4.55/100 pt years LARC= 0.27/ 100 pt years Efficacy not altered when stratified for age <21 CHOICE Study Results: LARCs had 81% continuation at 1 year--Better than any other non-LARC method!! LARC- Satisfaction CHOICE study: 75% of patients chose a LARC method 69% of adolescents chose a LARC method Women using LARC methods had highest satisfaction at 1 year follow up Method % Satisfied at 1 year Levonorgestrel IUD 86% Copper IUD 80% Subdermal Implant 78% Injection 54% Pills 54% Ring 52% Patch 42% Subdermal Implant: What are the risks? Complications are rare (<1%) Infection Hematoma formation Local irritation Expulsion- rare case reports occurring in setting of infection Subdermal Implant: Bleeding patterns Unscheduled bleeding Can not predict bleeding pattern Abnormal bleeding can lead to discontinuation in 10-14% of patients Meta-analysis (780 women) Evaluated bleeding patterns in first 2 years of use 22% amenorrhea 34% infrequent bleeding (<3 episodes of bleeding) 7% frequent bleeding (>5 episodes of bleeding) 18% prolonged bleeding (≥1 episode lasting >14 consecutive days) IUD Risks: “This ain’t your Mama’s IUD” Infection: Monofilament string- does not increase risk of pelvic infection WHO clinical trial (23,000 IUD insertions) Risk of PID was same as baseline risk in population without an IUD Increased in first 20 days after insertion (9.7/1000 women-years) From 21 days- 8 years risk 1.4/1000 women years (same as general population) IUDs and Infection Screen for Gonorrhea and Chlamydia before or at the time of insertion What if GC/CT test comes up positive? TREAT---Do NOT REMOVE IUD Absolute risk of PID is low 0-5% among women with a positive GC/CT test at time of insertion IUD Risks: Expulsion Partial or complete expulsion from the uterus Skyla: 3.2% (clinical trial- 54 out of 1665) Mirena/Paragard- between 2-10% in first year What to do: Can replace it with another IUD Can change methods IUD Risks: Perforation Skyla clinical trial: incidence of <0.1% Mirena/Paragard: WHO: <1 per 1000 Dependent on experience of practitioner Insufficient data to demonstate a difference in perforation risk between parous and nulliparous women Only case series exist of difficult removals and laparoscopic removals IUD: Bleeding patterns Mirena® Most common change is decreased bleeding Average monthly blood loss drops by 90% At 1 year 20-40% amenorrhea Best bleeding profile among all options FDA approved for treatment of heavy menstrual bleeding IUD Bleeding patterns: Skyla™ First 90 days Second 90 days 1 year 3 years Amenorrhea <1% 3% 6% 12% Infrequent bleeding 8% 19% 20% 22% Frequent bleeding 31% 12% 8% 4% Prolonged bleeding 59% 17% 9% 3% Treatment days 1-28 Treatment days 337-365 Mean # bleeding days 7.3 (±5.6) 2.1 (±2.7) Mean # spotting days 9.2 (±6.1) 3.3 (±3.1) IUD: Other Myths and Misconceptions MYTH: IUD causes infertility Fertility returns immediately with removal Prior studies among infertile women showed no correlation with previous IUD use MYTH: IUD causes ectopic pregnancy Misconception: IUD insertion is painful/difficult in nulliparous Insertion not technically difficult Risk of discomfort (86% report discomfort with insertion) Pre-procedure misoprostol gives no improvement Overall well tolerated Lowers risk just as overall risk of pregnancy decreased Misconception: IUDs must be inserted 0-0.5per 1000 womenyears (compared to 3.25-5 in women without) If pregnancy occurs, proportion is higher during menses Can be inserted at any time Menses may make insertion easier Must exclude pregnancy Levonorgestrel IUD: Don’t Forget the Benefits!! Treatment of heavy menstrual bleeding Treatment of dysmenorrhea (“bad cramps”) Treatment of pelvic pain and endometriosis Use in those with medical contraindications to estrogen Menstrual suppression for physical and developmental disabilities Contraception in Teens: Some final thoughts A pelvic exam is not required for giving an adolescent birth control (IUD is exception) Quick Start is preferred for all methods Discuss concerns/misperceptions at the onset Case #3 16 year old female presents for routine gyn exam on Monday morning. Sexual history reveals that she is currently not using any hormonal contraceptive method. Had unprotected sex on Saturday night and concerned about her chance of pregnancy. Wants to know what she should do. Emergency Contraception Plan B One-Step™ - Levonorgestrel 1.5mg FDA approved in 1999 Available over the counter for age ≥17 2011- Dept HHS overturned FDA decision to make OTC without age restriction 4/5/13: Federal court rules emergency contraceptives needs to be sold over the counter 4/30/13: FDA approves morning-after pill without prescription for girls 15 and older Response to court ruling: American Academy of Pediatrics: “While pediatricians recommend that teens delay sexual activity until they fully understand its consequences, we strongly encourage the use of Society contraception, of Adolescent including Health emergency andcontraception Medicine: “Today’s to protect ruling theacknowledges health of our adolescent clear evidence patients that EC is a safe and whoeffective are sexually method active.” of backup birth control for all women of reproductive age” American College of Obstetricians and Gynecologists: “EC is a safe, effective way to help prevent unintended pregnancy after a contraceptive failure, unprotected sex, or sexual assault. We believe all EC products should be available over the counter.” Emergency Contraception: What is it? Levonorgestrel 1.5mg • Progesterone only medication taken in one dose • Decreases risk of pregnancy from 8% to 1-2% after single episode of unprotected sex • Can be taken up to 5 days after unprotected intercourse Emergency Contraception: How does it work? Progesterone Inhibits or delays ovulation May interfere with sperm transport or tubal motility Does not disrupt a pregnancy!!!! X X Let me repeat….. If you’re already pregnant, it won’t do anything to the existing pregnancy Will not cause an abortion Will not harm a developing embryo. Emergency Contraception: Who can take it? World Health Organization: Category 1 No restrictions to use Okay for females with contraindications to birth control pills Cardiovascular disease, liver disease, migraines, etc… Emergency Contraception: When do you take it? No clinical exam or pregnancy test necessary before use Any time unprotected or inadequately protected intercourse occurs Take as soon as possible after event Efficacy decreases with time Still moderately effective when taken up to 5 days after intercourse Emergency Contraception: What are the side effects? Nausea (18%) Vomiting (4%) Repeat dose if vomiting occurs <2 hours from initial dose Irregular bleeding Menses occurs usually within 1 week before or after expected Emergency Contraception: Costs approximately $50 Does not protect against subsequent intercourse Does not protect against STDs Need to discuss more effective forms of contraception References: ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol 2011;118:184-96. Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol 2012;120:983-8. FINER LB, ZOLNA MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011;84:478-85. KEARNEY MS, LEVINE PB. Why is the teen birth rate in the United States so high and why does it matter? The journal of economic perspectives : a journal of the American Economic Association 2012;26:141-66. YANG Z, GAYDOS LM. Reasons for and challenges of recent increases in teen birth rates: a study of family planning service policies and demographic changes at the state level. J Adolesc Health 2010;46:51724. MARTIN JA, HAMILTON BE, VENTURA SJ, et al. Births: final data for 2010. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2012;60:1-70. EDWARDS SM, ZIEMAN M, JONES K, DIAZ A, ROBILOTTO C, WESTHOFF C. Initiation of oral contraceptives--start now! J Adolesc Health 2008;43:432-6. EATON DK, KANN L, KINCHEN S, et al. Youth risk behavior surveillance United States, 2011. MMWR Surveill Summ 2012;61:1-162. References: THURMAN AR, HAMMOND N, BROWN HE, RODDY ME. Preventing repeat teen pregnancy: postpartum depot medroxyprogesterone acetate, oral contraceptive pills, or the patch? J Pediatr Adolesc Gynecol 2007;20:615. SUCATO GS, LAND SR, MURRAY PJ, CECCHINI R, GOLD MA. Adolescents' experiences using the contraceptive patch versus pills. J Pediatr Adolesc Gynecol 2011;24:197-203. ZIBNERS A, CROMER BA, HAYES J. Comparison of continuation rates for hormonal contraception among adolescents. J Pediatr Adolesc Gynecol 1999;12:90-4. RUSSO JA, MILLER E, GOLD MA. Myths and misconceptions about longacting reversible contraception (LARC). J Adolesc Health 2013;52:S1421. CARR S, ESPEY E. Intrauterine devices and pelvic inflammatory disease among adolescents. J Adolesc Health 2013;52:S22-8. ROSENSTOCK JR, PEIPERT JF, MADDEN T, ZHAO Q, SECURA GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol 2012;120:1298-305. WINNER B, PEIPERT JF, ZHAO Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med 2012;366:1998-2007. ACOG Practice Bulletin No. 112: Emergency contraception. Obstet Gynecol 2010;115:1100-9. Thank You!