Approach to Hemostatic Disorder
advertisement

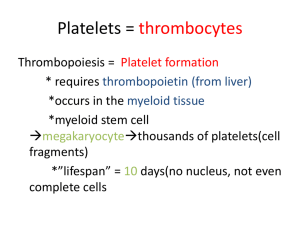
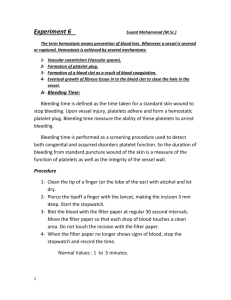
Coagulopathy Bundarika Suwanawiboon M.D. Yingyong Chinthammitr M.D. Theera Ruchutrakool M.D. Division of Hematology Department of Medicine Faculty of medicine Siriraj Hospital Bangkok Thailand 10700 Coagulopathy Bundarika Suwanawiboon M.D. Yingyong Chinthammitr M.D. Theera Ruchutrakool M.D. Coagulopathy Outline Basic of Normal Hemostasis (35 minutes) Theera Clinical and Laboratory Approach to Bundarika Bleeding Patients (35 minutes) Management of Bleeding Patients Yingyong (35 minutes) Question and answer (15minutes) All Normal Hemostasis Normal hemostasis Blood vessel Platelet Coagulation factors Fibrinolytic system Natural anticoagulants Red blood cell Platelet Red blood cell Platelet Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Red blood cell Platelet Von Willebrand factor Fibrin polymer Red blood cell Platelet Von Willebrand factor Fibrin polymer Red blood cell Platelet Von Willebrand factor Fibrin polymer Normal Hemostasis Normal hemostasis Blood vessel Platelet Coagulation factors Fibrinolytic system Natural anticoagulants Normal Hemostasis Blood vessel Endothelium Connective tissue or collagen Normal Hemostasis Blood vessel Endothelium Thrombogenesis von Willebrand factor Tissue thromboplastin Endothelin Antithrombotic Effect Thrombomodulin Platelet derived relaxing factor (PDRF) Prostacyclin (PGI2) Tissue plasminogen activator Normal Hemostasis Blood vessel Endothelium Connective tissue or collagen Normal Hemostasis Blood vessel Endothelium Connective tissue or collagen Collagen direct bind and activate platelet Release von Willebrand factor to bind platelet Normal Hemostasis Platelet Adhesion via glycoprotein (GP) Shape change from disc to ameboid form Release ADP, thromboxane A2, vWF Aggregation via glycoprotein (GP) Normal Hemostasis Platelet adhesion aggregation ligand receptor vWF GP Ib/IX/V collagen GP Ia/IIa fibrinogen GP IIb/IIIa Normal Hemostasis Platelet Platelet plug formation and vasoconstriction Primary hemostatic plug formation which is enough to stop bleeding from small and shallow wound Normal Hemostasis Factor XII HMWK/PK Factor XI Factor XIa Factor IX Factor X Coagulation pathway Factor IXa Factor VIIIa Factor VIIa Tissue factor Factor Xa Factor Va Factor X Prothrombin Thrombin Fibrinogen Fibrin Normal Hemostasis Factor XII HMWK/PK Factor XI Factor XIa Factor IX Extrinsic pathway Factor IXa Factor VIIIa Factor X Intrinsic pathway Common pathway Factor VIIa Tissue factor Factor Xa Factor Va Factor X Prothrombin Thrombin Fibrinogen Fibrin Normal Hemostasis Factor XII HMWK/PK Factor XI Factor XIa Factor IX Factor X Coagulation pathway Factor IXa Factor VIIIa Factor VIIa Tissue factor Factor Xa Factor Va Factor X Prothrombin Thrombin Fibrinogen Fibrin Normal Hemostasis Factor XII HMWK/PK Factor XI Factor XIa Factor IX Factor IXa Factor VIIIa Factor X Activated proteinC Protein S ProteinC Natural anticoagulant Factor VIIa Tissue factor Factor Xa Factor Va Factor X heparin antithrombin Prothrombin Thrombin Fibrinogen Fibrin Normal Hemostasis Fibrinolytic system High Molecular Weight Kininogen (HMWK) Prekallekrein (PK) Tissue plasminogen activator (t-PA) F.XII Urokinase Fibrin polymer Plasminogen Plasmin Streptokinase Fibrin degradation products (FDP) Normal Hemostasis “New concept !” Cell-based model of coagulation Normal Hemostasis 1. Initiation IIa Hemostasis occurs on two surfaces: TF- bearing cells and platelet 2. Amplification 3. Propagation IIa X TF VIIa prothrombin thrombin VIIa TF thrombin prothrombin IXa VIIIa Xa Va TF-expressing cell IX VIII/vWF V XI Va XIa platelet X IX XIa IXa VIIIa Xa Va Activated platelet Hoffman M et al. Blood Coagul Fibrinolysis. 1998; 9(suppl 1): S61-S65. X TF VIIa prothrombin VIII/vWF Xa Va thrombin TF-expressing cell IX VIIIa VIIa TF V XI prothrombin IXa thrombin platelet X IX XIa IXa VIIIa Xa Va Activated platelet Hoffman M et al. Blood Coagul Fibrinolysis. 1998;9(suppl 1):S61-S65. Va XIa Cell-based model “Three overlapping phases” Initiation phase “TF-bearing cell to generate F.Xa, F.IXa and (little amount of) thrombin” Amplification phase “Gererate cofactor F.V and F.VIII by little amount of thrombin from initiation phase” Propagation phase “Large amount of thrombin production (burst of thrombin) on activated platelet” Approach to Hemostatic Disorders: Clinical and Laboratory Approach Bundarika Suwanawiboon, M.D. Division of Hematology Department of Medicine What is the diagnosis? Clinical Evaluation of Bleeding Patients “80% of correct diagnosis can be made by history taking and physical examination.” History Taking Identify if the bleeding problem is due to Local vs. systemic defect Location: single vs. multiple sites Severity: Spontaneous? Appropriate to trauma? Hereditary vs. acquired disorder Onset Family history Underlying disease Medication Primary vs. secondary hemostatic disoder Primary Hemostasis Secondary Hemostasis Onset Immediate Delayed Sites Skin Superficial Petechiae, superficial ecchymosis Deep Deep ecchymosis, hematoma Mucosal Common Rare Others Rare Retroperitoneal hematoma, hemarthrosis Primary Hemostatic defect Secondary Hemostatic defect Laboratory Investigation of Hemostatic Disorders Assessment of Primary Hemostasis Platelet Complete blood count (CBC) Bleeding time/ PFA-100 Platelet aggregation study Blood vessel Bleeding time von Willebrand factor (vWF) Bleeding time vWF Antigen, vWF: RCO, vWF multimer, FVIII Complete Blood Count (CBC) Platelet number Normal platelet count: 150,000 –400,000/uL > 100,000/uL Bleeding unlikely < 20,000/uL ↑ risk for spontaneous bleeding Must exclude pseudothrombocytopenia Assess for platelet morphology Thrombocytopenia Giant platelet Bernard-Soulier Syndrome Pseudothrombocytopenia Etiology of Thrombocytopenia Decreased Production • Hypoproliferation • Aplastic Anemia, Amegakaryocytic thrombocytopenia, infection, toxins, drugs Infiltrative marrow disease, TAR • Ineffective Thrombopoiesis • Megaloblastic anemia Increased Destruction • Immune • Alloimmune, Autoimmune: ITP, SLE • Non-immune • DIC, TTP, HUS Others • Splenic sequestration • Hypersplenism • Dilutional • Massive blood transfusion Bleeding Time Bleeding Time: Interpretation Normal value* : 1-9 min Prolonged bleeding time: Thrombocytopenia/ anemia (Hct < 20%) Hereditary platelet dysfunction von Willebrand disease Severe hypofibrinogenemia Blood vessels disorders Uremia Myeloproliferative disorders Medication: Aspirin, NSAIDs,other antiplatelet drugs Platelet Aggregation Study Normal Platelet Response Arterioscler Thromb Vasc Biol 2000 20:285 Epinephrine ADP Collagen Ristocetin Arachidonic acid Normal Glanzmann’s +++ +++ +++ +++ +++ - - - +++ - +++ +++ +++ + +* +* Thrombasthenia Bernard-Soulier - +++ +++ ++ ++ - Syndrome Storage Pool Disease Aspirin Effect (no secondary wave) + ++ + von Willebrand Factor Synthesized in endothelial cells and megakaryocytes Two important functions: Carrier protein for plasma FVIII Ligand binding to platelet GPIb receptor to initiate platelet adhesion Primary Hemostasis: vWF Arterioscler Thromb Vasc Biol 2000 20:285 von Willebrand Factor Panel vWF antigen vWF ristocetin cofactor activity vWF multimer analysis FVIII level vWD Laboratory Diagnosis Test/Type 1 2A 2B 2N 3 ↑↑ N ↑↑↑↑ N or ↑ ↑↑ vWF:Ag ↓ ↓ ↓ ↓ or N ↓ or N ↓↓↓↓ vWFR:Co ↓ ↓↓↓ ↓↓ ↓ ↓ or N ↓↓↓↓ LD-RIPA - - ↑ - - - N ↓↓↓ ↓↓↓ N but ↓ absent BT N or ↑ 2M FVIII N or ↓ N or ↓ N or ↓ Multimer N but ↓ abnormal abnormal N but ↓ vWF Multimer Analysis Hoffmann. 4th Ed.Hematology Basic Principles and Practice Assessment of Secondary Hemostasis Screening tests: PT aPTT Mixing study Additional Tests Fibrinogen Thrombin Time Reptilase time Coagulation factor assays D-dimer Fibrin Degradation Product Euglobulin lysis time Accurate Sample Collection is the Key Always use 3.2% sodium citrate tube and sent to the lab immediately. Fill tube to the proper level. (anticoagulant to plasma ratio = 1:9) Modification may be required based on Hct Sodium citrate (ml) = (100 – Hct pt) x 0.5 / 55* * normal plasma vol. Extrinsic Pathway Intrinsic Pathway XII TF XIIa XI HK/PK HMWK IX IX VIIa XIa XIa VII Tenase IXa/ IXa VIIIa/PL VIIIa XX VIIa/TF Xa Xa Ca Ca++++ IIII Ca Ca++++ IIa IIa Va/PL Va/PL Fibrinogen Fibrinogen Common Pathway Fibrin Fibrin XIIIa X-linkedFibrin Prothrombin Time (PT) PT : test extrinsic and common pathway Activated Partial Thromboplastin Time (aPTT) aPTT : test intrinsic and common pathway Mixing Study Deficiency Correctable Normal coagulation time 50% + Inhibitor 0% 100% Prolonged PT or aPTT occurs when coagulation factor < 35-40% <35% Uncorrectable prolonged coagulation time Interpretation of Abnormal Coagulogram Isolated prolonged PT Isolated prolonaged aPTT Prolonged PT and aPTT Isolated prolonged PT Mixing study Correctable Deficiency Hereditary: FVII Acquired: Early liver impairment Vitamin K antagonist Vitamin K deficiency Uncorrectable Inhibitor FVII (rare) Lupus anticoagulant Isolated prolonged aPTT Bleeding No bleeding Mixing study Mixing study Correctable Uncorrectable Correctable Uncorrectable Deficiency Inhibitor Deficiency Inhibitor Factor VIII /vWD Factor IX Factor XI Factor VIII Factor IX Factor XI Heparin Factor XII HMWK Prekallekrein Factor XII HMWK Prekallekrein Lupus anticoagulant Acquired FVIII inhibitor Prolonged aPTT and PT Mixing study Correctable - FII,FV or FX deficiency - FV and VIII deficiency - Liver disease - Vitamin K antagonist - Vitamin K deficiency - DIC Uncorrectable - FII, V, or X inhibitor - Lupus anticoagulant - LAC + Factor inhibitor Bleeding Disorders with Normal PT and aPTT Factor XIII deficiency Dysfibrinogenemia Mild isolated factor deficiency a2 -antiplasmin deficiency Elevated fibrin degradation products Platelet disorders Vascular disorders Further Diagnostic Tests Specific coagulation factor assay Coagulation factor inhibitor assay Lupus anticoagulant panel Other Tests for Secondary Hemostasis Fibrinogen D-dimer Fibrin(ogen) degradtion product Thrombin time Reptilase time Euglobulin lysis time Fibrinogen Functional level (200-400 mg/dl) ↓ Fibrinogen (esp. < 100 ) DIC Fibrinolytic therapy Primary fibrinolytic state Congenital afibrinogenemia Acquired/congenital dysfibrinogenemia ↑ Fibrinogen Inflammatory states/acute illness May associated with shortened PT/aPTT D-Dimer Measured cross-linked fibrin degradation product by plasmin More sensitive and specific for fibrinolysis than Fibrin(ogen) Degradatioin Product (FDP) ↑ D-dimer: DIC Acute thromboembolic episodes Post-trauma or surgery Malignancy Fibrin(ogen) Degradation Product ↑ levels in Primary fibrinolytic syndromes DIC After lytic therapy Acute thromboembolic episodes After injury/surgery Thrombin Time Thrombin Time (TT) Assess the ability to convert fibrinogen fibrin by adding thrombin to plasma Prolonged TT: Inhibitor of thrombin: heparin, anti-thrombin antibody Hypofibrinogenemia or dysfibrinogenemia Inhibitor of fibrin polymerization: fibrin degradation product, paraprotein Euglobulin Lysis Time Euglobulin fraction of plasma is precipitated by acetic acid and thrombin added. Lysis of clot is observed. Normal : > 120 min Shortened ELT: DIC Liver disease Primary fibrinogenolysis: malignancy, e.g. prostate carcinoma Management of Bleeding Patients Yingyong Chinthammitr 27 June 2007 Objectives • Efficient practice of replacement therapy • Management of common bleeding problems Goal of replacement Rx • Treatment of bleeding • Prevention of bleeding before procedure • Not treat only lab. esp. in irreversible causes of coagulopathy 1 unit WB = Whole blood WB PRC PRP FFP CRP PC Cryo PRC = Pack Red Cell PRP = Platelet-rich plasma FFP = Fresh frozen plasma PC = Platelet concentrates (other: apheresis PLT = 4-6 u) CRP = Cryo-removed plasma, FFP with cryo.-removed Cryo. = Cryoprecipitate (F VIII 100 u, vWF, Fibrinogen, F XIII) Other products • • • • • • • • Factor concentrates : VIII, IX Prothrombin complex concentrates (PCC) Activated PCC (APCC) DDAVP Vitamin K injection Recombinant F VIIa (novoseven) Tranexamic acid – antifibrinolysis Fibrin glue – two bottles: Fibrinogen & Thrombin Recombinant Factor VIIa (NovosevenR) EFFECTIVE+SAFE but VERY EXPENSIVE - Hemophilia with inhibitor (alloantibody) - Factor VIII inhibitor (autoantibody) - Uncontrolled bleeding from coagulopathy (liver failure) - Uncontrolled bleeding from thrombocytopenia - Uncontrolled bleeding from platelet dysfunction (uremia , congenital defect) - Severe surgical and traumatic hemorrhage II X TFPI Xa VIIa TF TF VIIa TF TF VIII/vWF Xa IIa Va Platelet V V Tissue factor--bearing cell IX IX TF TF TF VIIa XI a X IXa VIIIa VIIIa + free vWF Va II Xa Activated Activated Platelet platelet Va Va IIa XI XIa II X TFPI Xa VIIa TF TF VIIa TF TF VIII/vWF Xa IIa Va Platelet V V Tissue factor--bearing cell Va TF TF TF VIIa X VIIIa + free vWF II Xa Activated Activated Platelet platelet Va Va IIa XI XIa Fibrin Glue - มี 2 ขวด คือ 1. Thrombin 2. Fibrinogen, F XIII (cryoprecipitate) Thrombin XIIIa Fibrinogen ------------->Fibrin ------> Cross-linked Fibrin เติม Calcium ใน Thrombin อาจเติม Tranexamic acid ใน Fibrinogen ใช้ อุปกรณ์ two syringes with one air-line Tranexamic acid - anti-fibrinolysis - adjunctive Rx in areas with high fibrinolysis (Oral cavity, GI tract, GU tract) - Contraindication : DIC, Thrombosis, Renal bleeding (obstructive uropathy) - IV : 10 mg/kg/dose q 8 h - Oral : 25 mg/kg/dose q 8 hr - Oral wash in dental bleeding Bleeding • Thrombocytopenia • Coagulopathy • Combined Platelet level & Bleeding • • • • • > 100,000/mm3 < 100,000/mm3 < 50,000/mm3 < 10,000/mm3 < 5,000/mm3 No bleeding tendency Bleeding time prolongation Bleeding after trauma , surgery Spontaneous bleeding High risk for spontaneous CNS bleeding Thrombocytopenia & Bleeding • • • • • Platelet level Platelet function Anemia Local problem Coexisting coagulopathy Platelet transfusion • Symptomatic Rx , not Rx cause • Dose: 1 unit per 10 kg BW • Indication – Bleeding associated with thrombocytopenia – Prophylaxis, before invasive procedure/surgery • Contra-indication – TTP (Thrombotic thrombocytopenic purpura) /HUS (Hemolytic uremic syndrome), HIT (Heparin-induced thrombocytopenia) Prophylaxis in thrombocytopenia Condition Threshold Chronic stable thrombocytopenia <5,000 or (underproduction e.g. aplastic anemia) No Post-chemo stable patient <10,000 Unstable (fever or infection or coagulopathy or platelet dysfunction) <20,000 Invasive procedures, surgery <50,000 Neurosurgery, ocular Sx <100,000 Plasma derivatives: FFP, Cryo. • No medications added • Return to blood bank if not use within 30 min • Most adverse transfusion reactions occur in the first 15 min. • Time of transfusion – not exceed 4 hr • Rate in adult (good cardiac condition) : 200 - 300 mL/hr • NOT for: volume expansion, protein (alb, glob) nutrient Cirrhosis • FFP 10-15 ml/kg • Vitamin K 10 mg IV • Pitfalls – Uncorrected localized bleeding problem e.g. varice, mucosal lesion – Overdependence on PT – Goal: to correct or prevent bleeding, Not to achieve a normal PT – Timing of FFP therapy before an invasive procedure Vitamin K deficiency - Vitamin K : fat-soluble vitamin - Vitamin K-dependent factors : II,VII,IX,X ; Protein C,S,Z - Vit.K : K1(green vegetables), K2(gut flora), K3(synthetic water-soluble) Vitamin K deficiency * Neonatal : hemorrhagic disease of the newborn * Children & Adult : - low intake - absorption defect - cholestasis, fat malabsorption syndrome - broad-spectrum antibiotics (+low intake) Vitamin K deficiency • Vit. K 10 mg IV slowly, sc • FFP • Prothrombin complex concentrate (PCC) HEMARTHROSIS AND HEMOPHILIC ARTHROPATHY Hemophilia A • Cryoprecipitate • Factor VIII concentrates • FFP • DDAVP vWD • DDAVP • Cryoprecipitate • F VIII concentrates • FFP Hemophilia B • FFP • Cryo. Removed Plasma • F IX concentrates Rx of Bleeding episodes in Hemophilia Site Level (%) Rx Length Joint 30-40 1 dose Muscle 30-40 1-3 doses Hematuria 30-40 1 dose Retroperitoneal 50 5-7 d GI 50 5-7 d Neck 100 7-10 d Intracranial 100 10-14 d Hemophilia A with hemarthrosis • • • • 60 kg. Raise F VIII to 30 % 1 u/kg raise 2% F VIII half life = 12 hr – Raise 30% -> 15 u/kg = 15x60 = 900 u – Cryo. 9 bags ( cont. ~5 bags q 12 hr) Hemophilia B with hemarthrosis • • • • 60 kg. Raise F IX to 30 % 1 u/kg raise 1% F IX half life = 24 hr – Raise 30% -> 30 u/kg = 30x60 = 1800 u – FFP 1800 ml. ( cont. 900 ml. q 24 hr) Warfarin-associated coagulopathy & bleeding • Life-threatening Bleeding – withhold warfarin, FFP/PCCs, vit. K 5-10 mg. i.v., provide medical support (e.g. PRC) • Major, non-life-threatening Bleeding – withhold warfarin, FFP/PCCs, vit. K 1-10 mg. i.v., provide medical support (e.g. PRC) J Thromb Haemost 2006;4:1853-63 Warfarin-associated coagulopathy & No bleeding INR 4.5-10 – Withhold warfarin – Withhold warfarin – Vit. K 1 mg. – Reintroduce at a – Recheck INR in 24-48 hr lower dose on the following day – Recheck INR in < 72 hr INR >10 – Withhold warfarin – Vit. K 1 mg. i.v. – Recheck INR in 24 hr Identify and correct the cause of elevated INR Beware of re-thrombosis from overcorrection J Thromb Haemost 2006;4:1853-63 Heparin • Unfractionated heparin (prolonged APTT) – Bleeding: hold heparin, protamine (1 mg/100 u heparin) – No bleeding: hold heparin (Hf. life 1 hr) • LMWH (normal APTT) – Bleeding: protamine (neutralize all anti-IIa but 75% of anti-Xa) DIC • Rx cause • Bleeding – FFP , PLT concentrate – Cryoprecipitate raise fibrinogen > 100 mg/dL :1 bag/5 kg BW raise fibrinogen 100 mg/dL Treatment of DIC * Treat associated disease * Bleeding - Replacement therapy * Thrombosis - heparin : purpura fulminans, acral/dermal ischemia, retained dead fetus syndrome, giant hemangioma, aortic aneurysm without rupture, solid tumor * AT concentrate, APC Massive blood transfusion • > Total blood volume in 24 hour • Dilution and/or consumption of PLT, Coag. Factors • LAB: platelet, coagulogram, fibrinogen • PLT > 50,000, PT <1.5 times the midpoint of normal range, Fibrinogen >100 mg/dL : generally adequate for hemostasis Platelet dysfunction • Stop Antiplatelet agents before surgery – Aspirin : 7 days (irreversible inhibition) – NSAID : 1-4 days (reversible inhibition) – Clopidogrel : 10 days Uremic bleeding Treatment Regimen Onset *PRC /LPB Hct ~30% 1h *EPO 50-100 U/kg Hct 30% (~6 wk) *Cryoppt. 10 units 1h *DDAVP 0.3-0.4 mcg/kg 1 h IV or SC 2-3 mcg/kg intranasal Duration While Hct at this level Same *Conjugated 0.6 mkd IV estrogen 50 mkd po x 5 days *Dialysis 14 d (IV) 5 d (PO) 6h 2d 24–36 h[Effective ~ 50%] 4–8h Thank you for your attention Question…