PhysAbility Manual
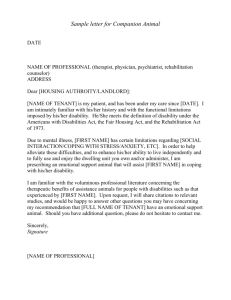
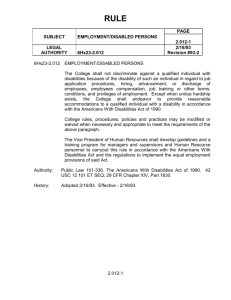
advertisement

PHYSABILITY CONTENTS Introduction…personal Introduction …program R.A.M.P Disability Specifics Intellectual Disability Autism and Autism Spectrum Disorders Cerebral Palsy Down Syndrome Hearing Impairment / Deafness Brain Injury Psychological & Mental Illness Spinal Cord Injury Blindness & Visual Impairment Assessment Tool Task Analysis Inclusive Coaching Sporting Organisations Welcome to PhysAbility and thank you for taking an interest in the wellbeing of others. With many things in life it’s often a case of not knowing what we don’t know till we find a need to know. For some that will start a journey of research to find out, others a three pointer in the big too hard basket and the rest will turn to professionals for information. PhysAbility is a link between people wanting to know and professionals who have the training around the concept of physical activity for bodies of all abilities. Finding myself in the realm of ‘wouldn’t have a clue’ when my youngest son Dane was diagnosed with Autism Spectrum Disorder at the early age of 20 months, it opened up a whole different world of parenting and, with my very narrow knowledge base limited to a Rainman (Dunstan Hoffman) reference, I pursued the internet, books, professionals to increase my knowledge and join the dots so to speak. Being a fairly active person (ok the 4 years in the UK doesn’t count) I encouraged both my children to do the same. Yes Dane took a bit more figuring and as an absconder, activities were inside under lock and key, trampolining at home, local gymnastics and encouraging his love of water, lessons at the local swimming pool. Meeting instructors with the patience of saints enabled us as a family the opportunity of doing things together such as Sawtell Swim Club on a Friday night, a great way for our local community to meet Dane and vice versa. All families are different and circumstances vary for those with disabilities as it does with those of more able bodies but in the following years it became more and more apparent to me a variety of barriers were in place that were preventing a majority with disabilities from engaging in any form of physical activity. Children I had the pleasure of teaching swimming during their school years, were ballooning to near obesity levels in supported living situations, aged parents not having the physical capacity to assist their grown children participate in social sport, recreational activities and those whose lifestyle were sedentary and opportunities not passed on to those in their care. So, the seed of breaking down some barriers through increased awareness was sown and in time a plan unfolded. I learnt a while ago that if I want others to step out of their comfort zones then I need to lead by example. So under the banner of Konnecting Kommunities thru Km’s I decided to run from Tweed Heads to Coffs Harbour via Lismore to raise funds. Why; 1. to put together a living manual that would assist health, fitness professionals have a broadened understanding of the barriers preventing people with disabilities from accessing opportunities under the banner of personal fitness. 2. Information for clubs and supporting groups regarding inclusive practices for all abilities; 3. Forum for individuals to share their experiences, and 4.Event accreditation by assistance with course layout for adaptive athletes. As a triathlete you would think that running wouldn’t be a challenge? As one who firmly believes that triathlons should be a swim, bike, bike and being a middle aged woman who is a bit round, running does not come the easiest for me. So with beautiful support from our local community, fellow runners Jenny and Peter, support crew of Anthony (who ran a big bit more than he anticipated). We headed up the highway. Unfortunately due to injury Peter didn’t get to start but the team “soldiered on” and 304km later ran onto Coffs Harbour with one goal satisfied and another beginning. PhysAbility is not an exhaustive document but one that hopes to bring professional, sporting clubs, groups and people with all types of disabilities to a starting point where a common language can be used to form partnerships that may last a lifetime… a healthy lifetime. All bodies are designed to move..in their own way. With thanks, Jo Magill PhysAbility is based upon the belief that everybody, no matter what our internal and external wiring may be, enjoys and benefits from voluntary movement. Are you aware that 4.2 million Australians are estimated to have a disability? That now equates to 1 in 5 people currently living in Australia. The overall population of people with disabilities is increasing. There are multiple reasons for this, including better identification, increasing levels of obesity, improved technology that saves and sustains lives and the aging demographics. Many people with intellectual/developmental disabilities are living much longer and are experiencing the long term effects of a disability combined with the effects of aging. Many health disparities observed with people with disabilities aren’t necessarily a direct result of having a disability and may occur directly or indirectly from a lack of good health promotion practices. People of all ages with disabilities face substantial health risks associated with a physically inactive lifestyle. Unfortunately even when individuals with disabilities want to increase their physical activity levels, they are often confronted with many more barriers than the general population. This can create a ‘chicken and the egg’ scenario. People with disabilities overall are often the least active members of the community but need activity most, because of secondary complications arising from sedentary behaviour. Poor aerobic capacity, poor muscular fitness and flexibility can often lead to restricted functional independence and increase risk of chronic disease complications such as coronary artery disease, hypertension and depression. While regular physical activity has the potential to offset some of the decline in health and function observed in people with disabilities, barriers to promoting increased physical activities must first be addressed. Barriers identified include poor accessibility, lack of awareness of fitness facilities, transport, lack of knowledge of how and where to exercise, perceived discrimination, expense of training, foreign unfamiliar environmental thought. Young adults with moderate to severe disability often have great difficulty transitioning from adolescence to adulthood where programs such as recreation and physical activity were primarily school based which is no longer part of the individual’s life. Children with disabilities also have significant lower levels of physical activity compared to their nondisabled peers and by adolescence inactivity has been reported as 4.5 times higher in comparison. As in the whole population, higher levels of inactivity during childhood and adolescence are likely to contribute to increased risk of adverse health conditions alongside rising health costs. Health and fitness professionals have a unique opportunity to impact a large and substantial segment of the population (ie people with disabilities) who are underutilising indoor and outdoor fitness and recreation facilities and programs in their community. This is where “PhysAbility” can help. As health and fitness professionals, we do not want to tell you how and why to work with your clients but wish to offer knowledge as to specifics of some disabilities that may pertain to your potential clients. While preaching to the converted; did you know: Resistance training 2-3 times a week for 6-10 weeks will lead to significant improvement in the strength of persons with Cerebral Palsy plus the added bonus of increased self-perception. Exercise training generally can produce significant gains in strength in paretic muscles through increased motor unit recruitment for someone with an incomplete spinal cord injury. With a complete spinal cord injury, intact muscle groups can be strengthened to be similar to the respective muscles in the general population. Randomized studies regarding the effect of exercise and Multiple Sclerosis found significant improvements in fatigue with exercise. Significant increases in VO2 peak and in duration, workload, and/of distance were shown in studies of the effects of exercise in persons with an intellectual disability. One study showed increased walking speed among older people with an intellectual disability. Apart from the physical benefits demonstrated, studies also revealed decreased perceived barriers to participation in exercise, and increased outcome expectations in self-efficacy and life satisfaction. Endurance and physical work capacity were improvements noted by persons with Down Syndrome who participated in cardiovascular exercise programs. And the list could go on…… PhysAbility aims to assist in the following ways: 1. Provision of a manual that can be used on a day to day bases when working with clients with a disability 2. 6hr workshop that brings PhysAbility to life including a. Theoretical education regarding disabilities & implications within the fitness and sporting industry b. practical application of adaptive practices in a gym setting c. Case study discussions covering: i. ii. iii. iv. Initial thoughts of specific fitness program for an individual client Challenges that are likely to arise initially and ways to overcome What would your assessment look like? Fitness program over 12 weeks including training sessions, goals, number of sessions, other challenges and v. Demonstrate to you client that gains in fitness are being made. 3. Adaptive Day for Sporting Clubs a. A half day workshop to help members of local sporting clubs and organisations identify ways for inclusive practice for all interested members 4. Event accreditation a. Assistance with course layout for adaptive athletes and participants b. Signage signalling PhysAbility friendly c. Events advertised on PhysAbility web site and FaceBook page R.A.M.P Value the no Value the why When thinking why you can’t, it becomes clearer as to why you can While recognising that many physical activities and sports have an element of inaccessibility for many with disabilities, a critical feature is to understand the type and nature of the barrier that many prevent individuals from engaging in physical activities. Using the acronym of RAMP – Restoring Activity Mobility and Participation, Rimmer and Schiller developed a model which systematically addresses barriers in the built environment experienced by people with disabilities. The idea of ramping up to successive levels offers a logical progression through the domains or rather four components – Access, Participation, Adherence and Function (Health). Each building on the previous, they reflect the interconnectedness between the components (levels) in achieving optimal health and well-being. Access is necessary for participation, and regular participation and adherence are necessary to obtain benefits in health and function. RAMP Framework Access refers to offering an opportunity to experience typical use of the environment or exercise equipment. The most commonly known access issues for people with disabilities is the physical access, into a building, full use of the available facilities, access on and off equipment. The more subtle aspect of access is information on the availability of services, facilities, programs and equipment. Without at least awareness of the options available, the options are functionally unavailable. One way to identify people with disabilities is to connect with local organisations who serve the disabled community. These include special education programs, independent living centres, developmental disability service providers, rehabilitation facilities, hospitals and long term care facilities. Meet with professionals in these settings, make them aware of the accessible physical activities that are available in their community, partner with them on transitioning people with disabilities into all areas of indoor and outdoor activities. Even commencing activities in a residential setting is a great way to build rapport and confidence remembering that where you start isn’t necessarily the final destination. As health and fitness professionals, sporting group co-ordinators can consider the following when establishing and upgrading premises and equipment: 1. Consider purchasing equipment using universal design features such as swivel-away seats; 2. Easy reach weights and easy to change weight on resistance machines; 3. Wide enough spaces between machines for transfer ease 4. Travel paths free of temporary or permanent obstacles 5. Good colour contrasts are good adjustments for users with visual impairments 6. Firm surfaces especially where transfers may occur 7. Adjusted height of benches, lockers etc any items that all members use 8. Sloped entries, slings, hoist etc especially around swimming pools or multi level sites where stair access is the norm Participation goes beyond physical access and refers to developing modalities of physical activity that are both beneficial and satisfactory for people with disabilities. Access is primarily concerned with availability and opportunities while participation is primarily concerned with usability or stage of readiness to use available opportunities. The emphasis on the participation component in the RAMP model is to ensure that the experiences of people with disabilities are not diminished relative to the experience of other participants. So whilst physical adaptation is required it is also essential that within the participation component, education and training of professionals who have little or no background in working with people with disabilities. Many people with disabilities find that the lack of knowledge about specific disability, poor professional behaviour and negative attitudes limits their opportunity to participate in a much wider variety of physical activity programs. People engage in physical activities for a variety of reasons but above all it’s the enriching experience that will have people of all abilities returning again and again. Please don’t limit your search of knowledge to within your own industry but include those who work alongside people with disabilities in their day to day lives, carers, family members, Occupational therapists, speech therapist etc.. Adherence presents possible the greatest challenge in securing the health benefits of physical activities. Full benefits can be and are achieved when individuals participate in moderate physical activities most days throughout their lifespan. So like most people variety is a spice of life… Possible strategies for increasing adherence to beneficial recreation and exercise programs involve varying the types of activities or activity locations and developing social networks that connect people and make the physical activity part of a socially engaging experience, part of the local community. Keep sight of a determined goal eg.. If wanting to go sailing but upper body strength and weight are current barriers; a. Weight program for strength b. Nutrition program to assist with weight loss c. Encourage visiting Sailing program, familiarising with equipment, d. socialising with others who share same interest of sailing Health and function sits at the top of the RAMP model and equates to achievements in beneficial health outcomes eg musculoskeletal, cardio respiratory, functional, metabolic and mental health. The ultimate goal of any health/fitness professional is to improve quality of life and help lower the risk of various health conditions. Therefore it is important to identify effective methods for measuring and monitoring physical activities For example, movement of upper extremities may account for only a small portion of total energy expenditure in the ambulatory population whereas wheelchair users use their upper body for all activities of daily living and for exercise such as arm cranking and wheelchair propulsion. Consequently, quantifying upperextremity movement is necessary for an adequate measure of physical activity among wheelchair users. It is also imperative to avoid an overuse injury resulting from repetitive motions associated with certain exercises. For someone whose daily activities are confined to self-propulsion in a wheelchair, continually working the upper body to exhaustion can impede even the most simple of their daily tasks. Overall, the establishment of good monitoring strategies to ensure the modalities chosen are safe and effective for the participants. Disability Specifics INTELLECTUAL DISABILITY Individuals with an intellectual / developmental disability have considerable limitations in intellectual function. They may have difficulty learning & managing daily living skills. This is because their cognitive (thought-related) processing is impaired. People with an intellectual disability often learn slowly, but given time, can adapt to new situations & enjoy many regular life experiences. Intellectual disability affects around 2-3% of the population in Australia. Intellectual Disability Characteristics: In clinical terms intellectual disability is often defined in terms of the severity of the condition: o Mild intellectual disability, IQ = 55 – 70 o Moderate intellectual disability, IQ = 30 – 35 o Severe intellectual disability, IQ = <30 The level of intellectual disability may be stable or can progressively become more severe. Intellectual Disability may co-exist with other physical disabilities. Generally speaking a person with an intellectual disability: o Learns & processes information more slowly than someone without an intellectual disability o Has difficulty with abstract concepts such as money & time o Has difficulty understanding the subtleties of interpersonal interactions Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. An intellectual disability cannot be treated with medication. Medication may be used for the control of other symptoms or illnesses which are affecting an individual, not the intellectual disability itself. Exercise Considerations: Fitness levels of persons with developmental disabilities are generally much lower than those of the general population. Most individuals with developmental disabilities get very little physical activity & carry high amounts of body fat, particularly women. These traits do not develop from their condition, but rather from their lifestyle. As they grow older, it is likely that a greater number of them will suffer from secondary disease & disability at an earlier rate than the general population Fitness levels of children with developmental disabilities are also often very poor, predisposing them to greater health risks in adulthood. Issues most related to exercise are: Issues most related to exercise are: Previous exposure to activity & exercise may be very limited There is often low motivation for exercise & lack of comprehension about the benefits of exercise Exercise will need to focus on activities which the client finds enjoyable & meaningful & in which they can achieve some success, which will assist with engagement & long term program adherence & success Factors such as limited cognitive understanding as well as limited physical capacity need to be considered Implications for Trainers: There are many ways to make positive lifestyle changes in persons with developmental disabilities using behavioral strategies that in many respects are no different from the general population. These may include: Develop a reward system that reinforces small accomplishments in the exercise program. Repeat this regularly Offer a ‘buddy’ system that will allow the person to exercise with a friend or someone they enjoy being around Keep visual wall charts to record progress. Many adults with developmental disabilities will enjoy seeing their names on the board & following their progress as they increase their physical activity levels Work with carers to incorporate activity into daily scheduling, such as shooting hoops, walking to shops, running around park for fun General Exercise Guidelines for Individuals with intellectual Disability: People with developmental disabilities have the same essential needs as the general population in terms of improving their health & fitness. An exercise program should include the three common elements: cardiovascular endurance, strength & flexibility. If there is not enough time, energy or concentration to complete everything in one session, break it up into two or three shorter sessions. Be conservative. Start the program at very low levels (e.g., 10-minute walk, 5 minutes on a stationary bike) & work toward higher levels once adherence is established. The highest dropout rate will usually occur in the first six months of the program. One very important strategy for increasing exercise compliance among persons with developmental disabilities is to motivate staff & caregivers. It will be extremely difficult to change the lifestyle patterns of persons with developmental disabilities if staff or family members are not proactive in encouraging physical activity participation. A fitness program should include as much variety as possible. Cardiovascular Exercise: One of the most challenging aspects of a physical fitness program for persons with developmental disabilities is improving cardiovascular fitness. Aerobic condition may initially be quite poor but progression is only limited by other coexisting conditions. Getting some adults with developmental disabilities to exercise at a sufficient intensity level for 20 to 30 minutes to attain these physiological changes may be difficult. It is best to start off slowly & gradually increase the workload. Start off at a lower intensity (45% to 55% MHR) & gradually increase the intensity as the person's fitness & motivation levels improve. Effective activities include those that are rhythmical, repetitive & simple in nature. Walking is a very simple & effective activity. Dancing is also a great cardiovascular activity that many adults with developmental disabilities enjoy. There are many other activities that can be used to improve cardiovascular fitness, including jogging, swimming, hiking, bicycling, arm cycling, stair-climbing, rowing & skating. Strength Training: The strength levels of adults with developmental disabilities are generally inferior to adults without developmental disabilities, but gains are only limited by lack of other coexisting conditions. Muscular strength & endurance is related to improved performance in daily activities including lifting & carrying things, walking up a flight of stairs, maintaining good posture & performing workrelated tasks (e.g., pushing carts, stocking shelves). Some recommendations for a strength-training program include: Do activities that the person enjoys The program should be progressive in nature & highly individualized The first few weight training sessions will require a great deal of supervision. Practice using the equipment for several sessions to ensure that the person understands how to properly lift the weight Emphasize the development of the arms, legs, stomach & back Provide adequate rest between exercises Teach persons to track & record their own progress. Simplified forms can be developed to teach persons with developmental disabilities how to record their results Provide clear feedback reinforce form & safety instructions frequently. Flexibility: Flexibility levels are only limited by other coexisting conditions & it should be given as much emphasis as it would in a program with any other population. Communication & Teaching Style: Effective communication is a cornerstone to success when working with clients with developmental disabilities. You may need to liaise with another professional such a speech therapist to develop effective communication strategies, or to understand what strategies work best for your client. Some points to consider: Clients may have difficulty communicating with you or understanding exercises & instructions, particularly verbal instructions. You may need to repeat instructions, in a variety of different ways to ensure full understanding. Sometimes demonstrations, pictures or diagrams can be useful. Allow additional time for an individual to mentally process an instruction or desired movement Sometimes memory may be problematic & instructions & demonstrations previously given to an individual may need to be repeated at each session. It may take a very large number of repetitions before a client becomes proficient or comfortable with an exercise or activity It is important that there is an element of success. Provide a lot of encouragement & motivation. Progress pictures, charts or goals may also provide motivation. Monitor the program on a regular basis The client may not be able to generalise a particular movement or activity to another piece of equipment, another place or another time. You may need to go over an activity each time a variable is changed Tips that may help you when communicating with someone who has a developmental disability include: Make sure you have the person’s full attention. User their name, gain eye contact or touch their arm to get their attention Speak clearly. Don’t rush. Allow the person time to listen, process your words & respond Use simple language, but start by assuming the individual can understand you, then adjust your level of communication as needed according to their response Ask the person how they prefer to communicate if they do not use speech. This can include gestures, communication aids or devices, sign language, facial gestures, head or hand movements. If you are not able to understand the person, you may need to ask their carer to assist Use appropriate language for the person & the situation – for example, simple, clear words & short, uncomplicated sentences. If the person is an adult, do not speak as though they are a child. Use visual aids such as pictures, diagrams signs, objects, gestures or miming to improve understanding Use respectful tone & volume. Try a different method rather than raising your voice Check their level of understanding by asking them to rephrase what you have said in their own words If you don’t think you have been understood, try repeating your message more slowly or using different words or methods If you don’t understand the person do not pretend that you have understood. Be honest & ask them to tell you again. Safety: There will need to be a lot of supervision, especially at the initial stages & when using machines or equipment for the first time. Also be aware that even if you are using the same machine, but in a different manner this will often seem like a totally new experience for the client so spend the time & explain, show & ensure that they can do the activity & use the equipment safely Resources & Further information: NSW Council for Intellectual Disability Australasian Society for Intellectual Disability http://www.nswcid.org.au/ https://www.asid.asn.au/ AUTISM & AUTISM SPECTRUM DISORDERS Autism Spectrum Disorder (ASD) is a developmental disability that affects affect a person’s communication, social skills & behaviour. It is typically diagnosed in childhood & often lasts throughout a person's lifetime. The most well-known types of Autism Spectrum Disorders are Autism & Aspergers syndrome. The word 'spectrum' describes the range of difficulties that people with ASD may experience & the degree to which they may be affected. The severity of its effects on each person can vary greatly. No one person is affected the same as another, & even one individual may not have the same consistent effects day to day. Some people may be able to live relatively normal lives, while others may have an accompanying learning disability & require continued specialist support. ASD Characteristics: The word autism means ‘absorbed in self’. Individuals with ASD might show a range of characteristics, & these characteristics vary between individuals. They can also change depending on the person’s age & stage of development. Many of the characteristics displayed by people with autism include: Impaired ability to communicate & relate to others socially Obsessive or repetitive behaviour – pre-occupation with certain objects or topics or wanting to do something over & over again. Displaying repetitive patterns of behaviour, such as body rocking, spinning, head-nodding, hand flapping, objecttapping, & light gazing Resistance to change, both in daily schedule as well as environment Unusual sensory interests such as sniffing objects or staring intently at moving objects Sensory sensitivities including avoiding everyday sounds & textures such as hair dryers, vacuum cleaners & sand Intellectual impairment or learning difficulties Co-ordination difficulties, often appearing awkward or clumsy. Tripping over or bumping into objects Hyperactive behaviour – hard to sit still & are always on the go Tics –uncontrolled jerky movements, such as blinking, twitching their faces, or jerky movements of the arm or shoulder Aggressive & highly emotional behaviour Difficulty understanding what you say & tendency to take things literally Secondary challenges including: o Anxiety & depression o Sleeping & eating disturbances o Attention issues o Temper tantrums, aggression or self-injury o Seizures Exercise is an effective therapy for children, adolescents, & adults with autism. It can reduce the severity of negative behaviours as well as improve social skills. Medication It's important to understand the effects that medication can have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. There is no medication that has been proven to address the core characteristics children with ASD show in the areas of communication & social relations. But medication can help ease challenging behaviours associated with ASD. Some of the most common medications prescribed may include Ritalin, Selective serotonin re-uptake inhibitors (SSRIs), Antipsychotics & Anti-epileptic medication. Side effects of each drug can vary greatly but may include: lower appetite tics & more repetitive behaviours Increased anxiety& hyperactive behaviour. irritable or nervous feelings gaining weight feeling tired or sleepy drop in blood pressure or heart rate Exercise Considerations: Exercise provides so many positive outcomes for children with autism, but the most important part is that the child is comfortable & is having fun. If the child can pick the activity / exercise themselves they can retain a sense of control. A lot of children with ASD are either overweight or at risk. Whilst decreased physical activity may be the primary reason for the increased rate of weight gain in children with autism, unusual dietary patterns & the use of antipsychotic prescription drugs can also lead to weight gain. Participation in physical activity may be challenging for individuals with autism for various reasons such as limited motor functioning, low motivation, difficulty in planning, & difficulty in self-monitoring. Increased auditory, visual, & tactile stimuli may too prove challenging. Physical activity involving social interaction such as team sports can present a difficult situation for someone with autism. However, if implemented appropriately, the addition of physical activity to an autism intervention program can help overcome many of these challenges & improve one’s overall quality of life. Aerobic exercise can significantly decrease the frequency of negative, self-stimulating behaviours. Exercise can also discourage aggressive & self-injurious behavior while improving attention span. One theory behind these findings is that the highly structured routines or repetitive behaviors (such as those involved with running or swimming) may be similar to & or distract from those self-stimulating, repetitive behaviors associated with autism. Physical activity can promote self-esteem, increase general levels of happiness, & can lead to positive social outcomes. For those with autism who are able to participate in team sports, this presents an opportunity to develop social relationships among teammates & learn how to recognize the social cues required for successful performance on the sporting field. Implications for Trainers: It is crucial for trainers to prepare for challenging behaviour by being aware of each child’s sensory sensitivity & providing a private / quiet space for the child to calm down. Individuals with ASD prefer to follow very specific routines. It is important to make any transitions or changes to the routine gradual & consistently. Avoid activities that the individual does not like or is fearful of. For example if a child has a fear of water, exercise in a pool may not be as beneficial as another activity that they would enjoy, such as dancing, running or horse riding. The exercise program needs to be individualised for each person, their own interests, hobbies & goals. The more fun it is & the more engaged the client is the greater the adherence & success. Some of the issues for people with ASD are: coordination difficulties - difficulty linking movements into a sequence or more complicated activity or difficulty learning new physical tasks. Difficulty with gross & fine motor skills. May tire more easily. Difficulty with understanding what you are asking them to do, especially if the activity is new to them or there is more than one step to it. General Exercise Guidelines for Individuals with Autism Vigorous exercise can have a positive impact on decreasing stereotypic behaviours Exercise can be used most effectively when it mimics the feedback that the child would receive from the self-stimulatory behaviour Cardiovascular Exercise: To maintain cardiorespiratory fitness, & also reduce disruptive behaviour, is around 6090% of the heart rate maximum for a minimum 20 minutes of exercise. Any form of vigorous aerobic exercise can be utilized to control non-functional behaviours associated with autism, allowing individuals to function more easily in the workplace, social & academic settings, & beyond. Some simple activities for individuals with ASD include: Running, dancing, swimming Pool - dog paddle, kicking with kickboard (no flippers) Water based exercise can also provide added benefits for children with autism. The weightlessness of the water allows for greater range of motion & fluidity, & ease of movements. The sensory signals that the child receives from being surrounded & supported by the water also help to calm & steady the child. It also assists the child in knowing where their body, arms & legs are in space (proprioception). Many children with an Autism Spectrum Disorder enjoy the feel & the physical support that the water provides. Children with an Autism Spectrum Disorder can find learning to swim in a group environment challenging due to the noise, splashing & unpredictable movements & playing of other children. One on one sessions, in a quieter time of the day & area of the pool can be more effective. If doing pool based activities be aware that children with an Autism Spectrum Disorder, often they do not like the ‘feel’ of the flippers on their feet. Strength Training: Stabilising & core activities are often required & need to be focused on before further progression of the program can occur. Some simple activities for individuals with ASD include: push ups sit ups swimming strokes & kicking - for developing core stability Flexibility: Specific muscle stretches are generally not indicated with ASD Coordination: Some simple activities for individuals with ASD include: climbing activities pool – freestyle, backstroke walking along a balance beam Communication & Teaching Style: Individuals with ASD may demonstrate various communication difficulties including: difficulty with eye contact & other nonverbal body language such as gestures & facial expression difficulty telling you what they want or need difficulty making conversation being awkward & ill at ease in a social situation unusual or challenging behaviours in response to their confusion & stress Important strategies for creating a supportive environment for children with autism to be able to actively participate in include: Establishing a routine, with clear structure to activities & visual cues Have a clear beginning & end to the session Use positive reinforcement Communicate in a way that the individual child responds well to Teach new skills by breaking them down into smaller, organized tasks & then rewarding them for successful achievement Avoid loud noisy places with increased distractibility Use clear, simple instructions Practising movement again & again. The individual with ASD will need more time than most of their peers to learn a skill. Practise for short periods of time, frequently (rather than a large chunk for an extended period) Break down a skill or activity into much smaller parts. You may only teach part of a skill or activity in one session. Practice the parts separately, then gradually link the parts together, in sequence until the whole skill is achieved To further assist with learning & developing motor skills & movement components, it is important to use all of the senses. Simple learning methods can include: Physical demonstration of a specific movement or activity Use picture cards or DVD’s / YouTube of people doing the movement/skill you are trying to teach Use picture cards which break down the movement or activity into its component parts. Place the cards in a row in the correct order to complete the correct movement sequence Vary the volume & tone of your voice Physically guide & move the child’s arm/leg/body movements. However note that some children with an Autism Spectrum Disorder can be exaggerated in their reaction to your hands-on guidance. They may seek out your touch or they may not like the sensation & avoid your physical assistance. If their reaction to the sensory input of your guidance distracts them from their learning, focus on visual learning strategies instead Be precise - if you move the child’s body/arms/legs in an awkward movement pattern, that is the movement they will learn The key things to remember in developing any physical activity program with individuals with ASD are: make sure it is fun make sure it is achievable make sure it is not too easy, not too hard select a variety of activities do little bits & often work out the best way they learn. Tailor the way you teach to the way the individual best learns. Try visual teaching methods first. Safety: Resources & Further information: Autism Fitness www.AutismFitness.com Autism Awareness http://www.autismawareness.com.au/ Autism Spectrum Australia http://www.autismspectrum.org.au/ CEREBRAL PALSY Cerebral Palsy (CP) is a non-progressive disease that affects both fine & gross motor control. CP is a condition caused by injury to the parts of the brain that control our ability to use our muscles & bodies. Cerebral = brain. Palsy = weakness or problems with using the muscles. While there are many obstacles associated with CP, it is still possible to have an active lifestyle. There are different types of CP, but all have similar characteristics. CP can be mild, moderate, or severe, which ranges from being clumsy to being wheelchair bound. CP doesn’t get worse over time, & most people with CP have a normal life span. CP Characteristics: The signs of cerebral palsy can vary greatly from person to person & may change over time. General signs of cerebral palsy may include the following: child is slow to reach developmental milestones such as learning to roll over, sit up, crawl, smile, or walk weakness in one (hemiplegia) or more limbs standing & walking on tiptoe difficulty with fine motor tasks clumsiness or difficulty maintaining balance walking with an abnormal gait, with one foot or leg dragging or a scissored gait involuntary & uncontrolled body movements excessive drooling lack of muscle coordination when performing voluntary movements (ataxia) rigidity, stiff, tight or contracted muscles & exaggerated reflexes (spasticity) learning problems difficulty with speech, hearing or seeing behavioral or emotional challenges muscle tone that is either too stiff or too "floppy" Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. People with CP may be prescribed anti-seizure & antispasmodic medications & these may decrease the intensity of aerobic exercise that they can do. Exercise Considerations: There are a variety of health & social benefits associated with exercise in this population, including: increased participation in individual & community activities improved sense of well-being & a reduction in anxiety increased lung & heart efficiency increased strength, flexibility, mobility, & coordination improved bone health weight control reduction of chronic diseases & secondary conditions (eg: osteoporosis) Implications for Trainers: The benefits of exercises for people with cerebral palsy are great but each individual has their limitations. As with everything else in life, moderation is the key. Know the client’s limits & understand that they will build stamina over time. An appropriate exercise program should not aggravate conditions that accompany cerebral palsy or other neuromuscular disorders. Individuals with cerebral palsy (CP) have challenges with movement, function & mobility that last a lifetime. The disability is non-progressive, with the physical challenges faced by this population stabilising once they reach adulthood. However, while the condition is not progressive, the level of independence & mobility may actually deteriorate as the person ages. Because of the dangers of inactivity, innovative forms of physical activity & exercise for persons with mobility impairment need to be developed & implemented. Many clients with CP may be wheelchair bound & or experience frequent seizures throughout their body. Individuals with CP are also more susceptible to overuse injuries because of inactivity & other associated conditions, such as contractures & joint pain. Good positioning of the head, trunk, & proximal joints of extremities is advised. This may include strapping of the hands or feet to the pedals when using the arm or leg cycle ergometer, or strapping of the individual’s pelvis in the wheelchair for proper positioning, as well as thighs to prevent adduction of the hips, or of the feet on the footrest to prevent slipping. Other simple adaptive items to consider include: The use of gloves during wheelchair exercise Velcro gloves can be used to attach the hands to equipment (if the client has trouble with gripping). For swimming programs, the use of flotation devices should be considered. For cycling, the use of a tricycle, tandem bike or pedal straps may be helpful. General Exercise Guidelines for Individuals with Cerebral Palsy Even though the design of the exercise training program should be similar to the principles for the general population, modifications to the training protocol may have to be made based on the person's functional mobility level, number & type of associated conditions, & degree of involvement of each limb. Persons with CP fatigue easily therefore, it is important to tailor the activity, intensity, & duration to your client. The use of short intervals & relaxation & stretching sessions throughout the training sessions can help to decrease fatigue. In general, 20-30 minutes per session is the minimum goal. However, during the first few weeks, several short sessions (e.g.: 5-10 minutes) per day can be better than a longer period. It is particularly important to increase the duration, intensity, & frequency of the exercise activity gradually. Duration should be increased progressively before increasing intensity. Aerobic exercise programs should start with frequent, but short bouts of moderateintensity (40-50% HRR). Once the client is comfortable, you can progress the exercise intensity to reach 50% to 85% HRR), gradually increasing the duration of each session as endurance improves. Reducing muscle spasticity may be an important goal of treatment. This can improve comfort & function & help prevent future musculoskeletal complications such as contractures (permanent tightening of the muscle). Early prevention of contractures may reduce the need for corrective surgery. Cardiovascular Exercise: Endurance training is best done with shorter duration of efforts (ie: 5-15 minutes), 2-3 times per week (or more often) if possible. If the condition is localized in the arms or the client is wheelchair dependent, arm cycling / ergometer cab be a great option, to increase cardiovascular fitness, muscular strength & flexibility. Walking can help improve the mobility of the leg & hip muscles, & can result in increased flexibility & better balance. Ensure a thorough assessment is conducted first so that there is minimal risk of losing balance & falling. Wheeling involves propulsion of a wheelchair by the arms or legs over an extended distance. Vigorous wheeling can be done inside or outside. It can be done using a conventional wheelchair or a specialized sport wheelchair, with or without a wheelchair roller. If wheeling outside, precautions should be taken for street traffic. Hills or gradients are also great for increasing intensity of wheeling (just be mindful of the downhill descent afterwards)! Strength Training: Resistance training for persons with cerebral palsy is vitally important. These exercises should be designed to target weak muscle groups that oppose hypertonic muscle groups, improve the strength of the weak muscle group, & normalize the tone in the opposing hypertonic muscle group through reciprocal inhibition. It is also recommended to have your client perform slow, dynamic strengthening exercises over the full range of motion. Muscle strengthening exercises are most effective when they are focused primarily on the muscle group opposite the tight muscle group. For example, biceps are tight, stretch & strengthen the triceps. For people with severe contractures or weakness, extra caution is advised to minimize muscle strain. Doing any type of stomach & back strengthening exercises will help counteract a lot of the typical postural problems associated with CP. The exercise program should change consistently with changes in muscle tone. Loads should not be at a maximum. Weights should not be allowed to dangle on the limb. Free weights (e.g. bar bells) should be used with caution by persons with athetosis (involuntary body movement.) Weights are not advisable for persons who cannot control the weights. If using free weights, it is recommended to have a partner or spotter. The strong pull of the hip adductors seen in many persons with cerebral palsy will require a resistance training program that places greater emphasis on strengthening the hip abductors. This does not necessarily mean that the hip adductors do not need to be strengthened. While the adductor muscles are often very tight due to spasticity, they may also be very weak. Therefore, both sets of muscle groups must be strengthened even though the abductors might have to receive a greater amount of work. Make sure that clients have not had a hip dislocation prior to working these muscle groups. Seek medical advice if your client has had a previous dislocation. A common type of cerebral palsy that results in weakness or paralysis to the right or left side of the body is spastic hemiplegia (a similar condition occurs in persons with stroke). Developing strength on the weaker side of the body will greatly assist with this condition. Since balance is often impaired in ambulatory persons with cerebral palsy, it is important to protect clients from injury by developing safe resistance training programs that do not expose them to a high risk of injury. Some clients will be able to work on strength exercises in a standing position with physical assistance from the instructor, while others will have to perform the exercise routines from a chair. Asses the client's balance before developing a resistance program to determine if standing exercises are safe. Certain individuals with cerebral palsy have a condition known as athetosis. This condition results in involuntary movements that occur in one or more of the person's limbs. The movements are uncontrollable & are often referred to as slow & 'writhing.' Facial muscles are also involved, which make the person appear to be laughing or crying. Since the movement of muscle groups is involuntary, use of free weights may not be possible because the hand may open reflexively during the weight routine. Elastic bands may also be a problem since the resistance may be difficult to control & may result in the band snapping back too quickly. Cuff weights & machines are the most appropriate modalities. Active-assistive exercise may be needed to perform the motion smoothly. Flexibility: Flexibility training is a very important part of the exercise prescription for persons with cerebral palsy because of the high level of spasticity. Stretching will help relax & repair muscle tendons from the constant tightness & contractions seen with these types of CP. It is important to include a proper warm-up & cool-down, as well as a stretching session to help maintain muscle length & flexibility. Ballistic stretching should be avoided. Yoga can be ideal for persons with CP, especially for those suffering from Spastic or Rigidity. Swimming & water based exercises are other great options. Because of water's natural buoyancy & resistance, it makes it easier for people to perform at optimal range of motion (ROM) without feeling the effects of gravity or extra stress on joints. Aqua therapy provides deep, intense exercise within a soothing & comforting environment. If in a heated pool the warm water therapy provides a massage effect on muscles, joints & ligaments. It is important to note that cold water can increase muscle tone, but warm water often has a relaxing effect & can help reduce muscle tone. Locate a pool / ocean with the water temperature that is best suited for your client’s tone. Coordination: Yoga, Tai Chi & Balance style classes are great for improving balance, mobility & coordination. Communication & Teaching Style: Cerebral palsy can affect a person’s ability to finely coordinate the muscles around the mouth & tongue that are needed for speech. Some adults with cerebral palsy may not be able to produce any sounds, others may be able to produce sounds but have difficulty controlling their movement enough to produce speech that is clear & understood by others. Some people may not speak at all, but they may have good understanding of what is said to them. Work with the person to establish ways in which they can show you whether or not they are receiving what you say & understanding it. Really listen to the person when they speak. While many people with CP have problems with speech, you can usually learn to understand their verbal communication over time. Various tips to assist with communicating with someone with CP can include the following: Go to a quiet place & so that you are completely focused on listening Show the person you are listening to that you want to understand. Lean forward, ask questions of clarification if you need to. Be an active listener Give them time to say what they want to say (a lot of people with CP have very slow speech). Don’t interrupt, don’t finish sentences for them or cut them off with statements like ‘OK. Don’t worry. I know what you mean’ & don’t speak for them. Tune in. Remember that the speech rhythms & voice pitch of someone who has vocal impairment are often very different from those of someone who does not. Once you become familiar with these differences, comprehending the person’s speech will be much easier. Be technology knowledgeable. It is important to understand the technological aids a person with CP might use. Communicating electronically. If you are ‘talking’ with a person through an electronic communication form, learn how they use language & how to respond in the same way – it will be easier for both of you. Sometimes reading the message aloud makes it easier to follow. Safety: Even very severely involved individuals with CP can enjoy physical activity & exercise, but they may need more supervision. In certain cases, cognition may be a limiting factor, as it may affect their ability to understand the use of equipment. Weight bearing & joint flexing exercises must be done with caution, especially if the client has contractures &/or loss of bone density. Special safety considerations include strapping of the hands or feet to the pedals when using the arm ergometer or cycling & strapping of the individual’s pelvis in the wheelchair for proper positioning. The use of gloves during resistance & wheelchair exercises is also recommended. For swimming programs, the use of flotation devices should be considered. Resources & Further information: Cerebral Palsy Australia Cerebral Palsy Support Network Cerebral Palsy Alliance The Centre for Cerebral Palsy https://cpaustralia.com.au/ http://www.cpsn.org.au/ https://www.cerebralpalsy.org.au http://www.tccp.com.au/ DOWN SYNDROME Down syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of an extra chromosome (chromosome 21). It is a condition that impairs cognitive ability & physical growth. People with Down syndrome can have numerous medical conditions & like the general population, some are very fit & healthy, while others experience a range of issues. There is no cure, but exercise can enrich the lives of people with Down syndrome by improving health, longevity & productivity. Most types of exercise can be performed with minor difficulty. However, special precautions are required to ensure safety. Down Syndrome Characteristics: short stature a particular set of facial characteristics shortened limbs & fingers low muscle tone minor physical limitations often affecting gait varying degrees of intellectual disability often difficulty with speech & social interaction some health & medical challenges o bowel issues o congenital heart conditions o increased incidence of leukemia o higher incidence of Alzheimer's disease Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication isn't used to treat Down syndrome itself, however medication is often prescribed to treat other health issues associated with Down syndrome. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. Exercise Considerations: An individual with Down syndrome can participate in most forms of exercise. Overall, this is a healthy population that enjoys the social aspects of physical activity. The inclusion of physical activity daily life will improve overall health. For individuals with Down syndrome, physical activity has important implications positively impacting on health, longevity, & productivity Issues most related to exercise are: Muscle hypotonicity (muscles have the ability to be stretched far beyond normal limits), joint hypermobility & ligament laxity (increased flexibility in their joints associated with increased susceptibility to subluxation & dislocation). It is important to note that hypotonicity & hypermobility are often associated with lordosis, dislocated hips, kyphosis, flat pronated feet, forward head, & atlantoaxial instability (AAI) Atlantoaxial Instability is a severe cervical disorder that occurs in approximately 17% of the population with Down syndrome & is characterized by increased laxity between the first & second cervical vertebrae. This makes spinal cord injuries much more likely. Medical clearance is highly recommended & strict monitoring is important to avoid injury to the spinal cord & other areas of the body mild to moderate obesity in adulthood (greater amongst women than men) an underdeveloped respiratory & cardiovascular system, resulting in reduced cardiovascular capacity poor balance & perceptual difficulties some health & medical challenges o bowel issues o congenital heart conditions o increased incidence of leukemia o higher incidence of Alzheimer's disease lowered general immunity compared to the general population other medical factors to consider in relation to exercise capacity are: thyroid hormonal deficiencies, abnormal energy expenditure & substrate utilization, impaired sympathetic response to exercise, & anemia Implications for Trainers: It is extremely important to confirm if a client with Down syndrome has AAI (instability of the joints in the neck) before participation in physical activity. Contact sport & heavy resistance activities are contraindicated when AAI is present. Encouraging the client to have regular health checks, & obtain medical approval for the exercise program, particularly if it will be a physically demanding one. Ongoing education on maintaining a healthy weight & living a healthy lifestyle is important. There can be a tendency for both children & adults with Down syndrome to become overweight. The effects of aerobic training on individuals with Down syndrome can have a positive training effect but this is usually after a long training program. Down syndrome clients will have difficulty generating resistance & their hyper-flexible joints make them more susceptible to injury during movements requiring higher degrees of coordination (e.g., power exercises, plyometrics, agility). Exercise intensity for Down syndrome clients should proceed gradually. Machine based resistance training & aerobic training is encouraged at the start of an exercise program because of its low level of difficulty. Reduced cognitive ability & hormone imbalances can result in decreased memory retention, decreased motivation to exercise, & other issues. It is important to make Down syndrome clients feel comfortable with exercise. The trainer needs to focus on gradual progressions, have patience & provide adequate supervision. A combination of aerobic & resistance exercise program may have a larger impact on physical fitness than aerobic exercise alone in people with Down syndrome Training can be linked to increased performance in activities of daily living (ADL) tasks, as well as work & leisure activities. Training could include teaching skills for particular sports or activities they are having difficulties with or wish to participate in. This may include task analysis & breaking down the activity into component parts so that training can focus on increasing skills for these component tasks. By linking training goals to the client’s life goals & activities makes them more meaningful & will result in a greater adherence rate, ie: improve cardiovascular fitness so the client can actively participate in a game of tennis with their friends. For children, the training program needs to extend beyond the development of motor skills & can include specific programs, advice & education for families so they can support their children to develop active play & sporting skills. There may be a need to raise expectations of what young people with Down syndrome can achieve among parents, professionals & the wider community. All motor activity only improves with the opportunity to learn & practice. The younger a client starts with a focused training program the greater improvement they will have over time & the more profound effect this will have on their life. It is also important to remember, when programming, that it is not necessary to aim at excellence or competence in particular sports. A more important goal is to find ways to keep children & adults with Down syndrome active rather than sedentary, ideally finding ways that are fun & can be enjoyed by other members of the family so that this can be reinforced regularly, become a regular part of the family ritual. General Exercise Guidelines for Individuals with Down Syndrome obtaining medical consent, particularly if AIA or any secondary issues are present understanding the effects of any specific medications on the body in relation to exercise providing increased supervision Incorporating behavioral therapy & motivational techniques (i.e., token reward system) to improve adherence. This is a system of social reinforcement with primary & secondary reinforcement. An effective technique is recording progress on a wall chart once they reach their goal. Starting the program with light activity that is enjoyable & pain-free. Cardiovascular Exercise: The goal of an aerobic training program for individuals with Down syndrome is to increase cardiovascular fitness. Recommended modalities include: walking, jogging, stationary cycling, & aerobic dance. It is important to monitor heart rate & blood pressure whenever possible to determine the intensity level of the activity & to avoid early-onset fatigue. The general recommended protocol is training at an intensity of 60-80% of an individual's maximal heart rate (MHR), 3-5 days a week, for 20-60 minutes per session. A suggested starting protocol can be 5-10 minute continuous activity, 1-2 days a week, gradually increasing over time. It is likely to take longer than with the general population to see a training effect. Strength Training: Children with Down syndrome often have a much harder time learning to walk, primarily because of their characteristic low muscle tone. Building muscle is critical to helping children with Down syndrome combat low muscle tone & reach development milestones. One of the most effective & easiest exercises to strengthen muscles for walking is climbing stairs. The goal of resistance training is to maximize strength in the large muscle groups. Training intensity should be 70-80% 1-RM for 3 sets of 8-12 repetitions. A training effect is typically seen 10-12 weeks into the program. Circuit training is appropriate for individuals with Down syndrome. A simple circuit program can include 2-minute stations with 30-60 second rest intervals between each station. Flexibility: Due to hypermobility & joint laxity that is associated with Down syndrome, excessive flexibility training is not recommended for this population. With any stretching the focus will need to be on correct technique & joint alignment in order to reduce stress on weak & instable joints. Communication & Teaching Style: Most people with Down syndrome are great communicators. It is quite common however, for children & adults with Down syndrome to demonstrate speech difficulties. People with Down syndrome often have much better receptive language than expressive language that is, they can often understand a lot more than they can tell us. People with Down syndrome respond more to visual cues than verbal cues. Relying on nonverbal skills such as gestures & body language can also be an effective way of communicating, especially if dealing with a younger person who may have a specific difficulty with learning grammar & developing clear speech. Tips to ensure optimal communication include: Use visual supports – eg: photos or pictures on written program labeling machines with pictures of what the machine is used for & how it works Providing both verbal & non-verbal encouragement providing more visual instruction than verbal instruction Teaching clients to record their own information to improve long-term adherence & empowerment. Use technology – eg: programs online or emailed to client If client is having difficulty getting their message across then ask them to physically show you what they are talking about Use face-to-face methods to communicate, ensuring eye contact Give instructions one at a time. Allow client time to respond (& process what you have just said) Safety: Constant supervision is integral for people with Down syndrome, especially if the exercise involves complex movements, physical contact or heavy weights Resources & Further information: Down Syndrome Australia Down Syndrome NSW http://www.downsyndrome.org.au/ http://www.downsyndromensw.org.au/ HEARING IMPAIRMENT / DEAFNESS There are different terms to categorise a hearing impairment. The most common ones include Deaf, hearing impairment or hard of hearing. Because there is such a vast range of sounds to be interpreted, there will be a wide variation between individuals & what sounds they are able to hear & interpret. Deafness & hearing impairment can be hereditary or due to a range of factors such as traumatic accident, injury, disease, medication, prolonged exposure to noise or ageing process. Hearing Impairment Characteristics: People with a hearing loss can be divided into distinct groups: Deaf. People who are born deaf or became deaf at an early age (before language acquisition) use the term Deaf (with a capital “D”). Deaf people identify themselves as part of a Deaf Culture & Community & are likely to use Auslan (Australian Sign Language) as a first or preferred language. These iindividuals have complete hearing loss & are unable to use residual hearing for processing information or communicative purposes, even with the use of amplification devices. People who are Deaf often see themselves as a language & cultural minority, not as a disability group deaf. The term deaf (with lower case letter “d”) is used more generally when referring to people with a condition that has led to them acquiring a hearing loss to whatever degree regardless whether signing or oral methods of communication are used Hard of Hearing / Hearing Impairment. Generally this term is used to describe people who have experienced varying degrees of hearing loss after the acquisition of speech & still use speech as a primary means of communication Medication Most people with Deafness or a hearing impairment do not require any specific medication to manage this condition. As with all populations it is imperative to be aware of any medication they may be taking & the impact this may have on their safety & exercise performance. Exercise Considerations: Generally there are no physical limitations directly associated with hearing impairments. Most individuals can take part at a high intensity of exercise or sport without any special considerations. While people with hearing impairments do not differ radically from the general population with respect to exercise. However both children & adults who are hard of hearing or Deaf tend to have a higher incidence of overweight & obesity when compared to the general population. Balance & spatial awareness concerns may be evident, depending upon the specific type of hearing impairment the person has. This can have an effect on motor performance, especially in dynamic & competitive sport situations. However, deficits in balance should not prevent involvement in physical activity programs. Incorporating balance activities into the fitness program can improve performance & decrease the risk of falls, especially in older adults. Effective communication & understanding are important considerations when working with someone who has a hearing impairment. A client with profound hearing loss may not be able to hear music at an acceptable level for participation; however, they may feel the vibrations either through the floor or by holding a vibration-transmitting object while completing exercise movements. Spoken communication is also a concern for people with severe to profound hearing loss. This can lead to fewer social opportunities, lower selfconcept, decreased self-esteem, lack of self-confidence, & isolation. Implications for Trainers: There are four different types of hearing loss: conductive, sensorineural, mixed, & central hearing loss. Some of these types may affect dynamic balance & spatial orientation specifically sensorineural. This may in turn affect the clients' cardiorespiratory efficiency in exercises or activities requiring high levels of balance. General Exercise Guidelines for Individuals with Hearing Impairment If there are no other limiting factors or secondary conditions, the rules for exercise prescription intensity can be the same as the general population Balance & Flexibility: Various balance activities that can assist with improving balance for Deaf clients include: Tumbling & gymnastics Practice of basic body movements – including Tai Chi, Yoga & Body Balance classes Dance Martial arts Gym based equipment / Environmental modifications Avoid loud, constant background noise as this may cause headaches (from echoes or vibration) or reduce the effective use of hearing aids. This can be especially problematic in a gym environment Ensure adequate lighting Facilities can be equipped with strobe or visual fire alarms or other alerting devices or strategies. Alerting devices or strategies include use of the buddy or tapping system, very loud sounds, vibrations, colorful flags, or flashing lights. Communication & Teaching Style: Around 10% of Australians have a hearing loss. Generally, the more hearing a person has, the more they will speak & rely on lip reading. The less hearing they have, the more likely they will use Sign Language. Each individual has a particular communication preference which is often related to family upbringing & the schools they have attended. Hearing aids can help some people, but they only amplify whatever sounds can be heard. Unclear sounds remain unclear; they are just louder. Auslan is recognised by the Australian Government as an Australian Community Language. Auslan is a visual language that includes; sign vocabulary, complex grammatical rules, facial expression, body language & finger-spelling. It is not the same as English. Even the most experienced speech readers are able to pick up only about 30% of spoken language. Strategies that can enhance communication effectiveness include: Always face the person so that he or she can see your face, lips, eyes, & body. Stay close enough to the client so they can see your mouth & facial features Identify yourself - don't assume the person will recognise you by your voice Speak at normal speed, but avoid speaking too fast Maintain eye contact & speak directly to the person, not to the interpreter if one is present Use facial expression, body language, gestures, & common signs or cues, such as thumbs up or down to communicate emotions & meanings Avoid chewing gum or food, covering the mouth, or having an untrimmed mustache Use normal enunciation & loudness, regardless of whether the person is deaf or hard of hearing or uses a hearing aid, cochlear implant, or no assistive listening device Demonstrate exactly what is required from start to finish, as many people who are deaf or hard of hearing are very visual learners Some basic cue or feedback signs, for words such as "ready," "start," "faster," "ok," "stop," or whatever words are necessary for activity should be established & used consistently Use accurate & specific language when giving directions. For example, "the door is on your left", rather than "the door is over there". Avoid situations where there is loud or competing noise Visual & tactile cues should be used to enhance understanding, including having a notepad on hand if needing to write words down. Present instructions in writing or picture form via signing, or on a video with closed captioning Allowing the person to describe or demonstrate the test protocol before the task begins If an individual's speech is unclear or difficult to understand, the listener should not pretend that he or she understands, but rather ask for clarification In a group situation, introduce the other people present Never leave a conversation with a person without saying so Safety: The individual should be orientated to all aspects of the facility, & environment with special attention to emergency aspects, such as exits & fire evacuation procedures. Having an OHS procedure listing how to ensure all members are aware of any alarms (especially if only auditory in nature) further improves safety. Hearing aids & external cochlear implant devices should be removed before participation in activities involving contact & in water activities. Resources & Further information: Deaf Society of NSW http://deafsocietynsw.org.au/ Vision Australia http://www.visionaustralia.org Royal Institute for Deaf & Blind Children http://www.ridbc.org.au/deafness Australian Sign Language http://www.auslan.org.au/ BRAIN INJURY Acquired brain injury (ABI) refers to an injury to the brain that results in the deterioration in level of functioning. This can occur traumatically as the result of extreme force exerted on brain tissue (such as a fall, car crash, near drowning or blow to the head), or from internal causes (such as a stroke, brain aneurysm, infection or tumour) when the brain does not get enough blood or oxygen. An ABI can occur at any age, to anyone, but certain groups are more likely to experience a brain injury. Children under the age of 4 are at risk of injury from falls & child abuse. Adolescents aged 15-19 are at an increased risk due to sports & car crashes. People aged 75 years & older are at risk from falls. Many people with an ABI adopt a sedentary lifestyle. The role of increased physical activity is necessary as a preventative measure against chronic disease, cognitive challenges, & depression in people recovering from ABI. Acquired Brain Injury Characteristics: Because the brain controls our ability to move, think, sense, & socialize, the symptoms that result from ABI can vary widely. They may include: Physical symptoms. Weakness or difficulty moving the arms, legs, body, & head. The person may have difficulty sitting, standing, balancing or walking. Fatigue, decreased range of motion, & poor endurance can also be affected, as well as bladder & bowel problems. Cognitive symptoms. Difficulty remembering, paying attention, planning, goal setting or solving problems. The individual may also display learning & attention deficits. They may have a reduced awareness of these difficulties, which can cause safety concerns. Sensory symptoms. Changes in vision, hearing, or the sense of touch. Balance senses that are aided by the inner ear may also be impaired. Emotional & behavioral symptoms. Difficulty in controlling emotions, or even a change in personality. Behavioral changes may also include onset of depression & anxiety, disruptive or combative behavior, lack of inhibition, self-abuse, irritability & detachment from reality. If cognitive deficits are significant, the person's inability to understand what has happened may result in significant emotional agitation. Unlike individuals with developmental disabilities, people with brain injuries are often acutely aware of these limitations. They are still able to remember their abilities prior to the incident & can experience significant loss Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. Exercise Considerations: Most therapy interventions after ABI focus on specific impairments such as spasticity, flexibility, muscle strength, balance, gait mechanics, improving physical work capacity, endurance & functional skills. Benefits of exercise for people with ABI include: Reduced physical, emotional & cognitive complaints & symptoms, such as sleep problems, irritability, forgetting, & being disorganized. Improved cognitive & memory Reduced depression & higher levels of self esteem Improved engagement in school or work & community integration Decreased risk of developing secondary health problems Targeted exercise can also assist with improving: Alertness levels & following commands Muscle & joint flexibility General mobility, balance, coordination & postural control Strength & energy, reducing any feelings of fatigue that occur from inactivity or the injury to the brain itself A return to sports, fitness & work activities Issues most related to exercise are: People with brain injuries generally have a greater propensity towards poor health habits as well as having poor health profiles. As in other special needs populations, the benefits of a proper exercise program can be helpful in the avoidance of secondary health problems. People with ABI also have a greater risk of developing circulatory problems, including heart disease & stroke. Trainers need to be aware of the importance of the prevention strategies to reduce the cardiovascular disease & illness in a client with ABI. Implications for Trainers: Many people with TBA may have difficulties with agility, dynamic balance & coordination. These may only be subtle but could easily prevent the client from being able to safely participate in high level mobility type activities, such as sports & contact activities. Individuals with little physical impairment may have barriers to participation because of cognitive, behavioral & executive impairments. These individuals will need to receive the proper supervision & education throughout their training programs. Structured exercise programs with regular routines will help with attendance, adherence & progression with exercise program. Fatigue levels can be significantly impacted following an ABI. Trainers may need to schedule shorter sessions, or time the sessions for when the client is at their optimal energy level General Exercise Guidelines for Individuals with traumatic Brain Injury For some clients with an ABI, something as simple as walking down out the front door may be taxing. Before starting a fitness program, consult with their doctor or therapist regarding any physical challenges, balance problems or other issues that may affect the client’s safety. Participating in a regular fitness program not only improves fitness outcomes, but the skills required to execute & maintain a program may also help improve cognitive function after injury. Although the needs of an individual with a brain injury are the same as those of a non-injured person with regards to physical fitness, steps must be taken with each individual to ensure that the specific functional disabilities are addressed to ensure the success of the program. Each person has different needs & approaches to motivation, communication, & the individual's capacity to understand & follow a fitness program must be individualized. Cardiovascular Exercise: A sedentary lifestyle & lack of endurance are common characteristics of individuals with ABI. In general people with ABI will often have reduced peak aerobic capacity of 65-70% of the general population. This may mean that intensity & duration of the session needs to be lower (ie: 60-70% Max HR, with sessions between 20 – 40 minutes duration). For home based exercises sessions may be better broken down into 10 minute bouts throughout the day, or shorter if needed. Increased physical activity & exercise training improves cardiorespiratory fitness in many populations with physical & cognitive impairments. Therefore, increasing the endurance & cardiorespiratory fitness of persons with ABI would seem to have important health implications. Strength Training: Depending upon the residual physical limitations strength training may need to focus on improving range of movement, co-ordination & function rather than pure strength improvement. Range of motion exercises can help maintain strength as well as flexibility of the joint. Such exercises as simply extending & flexing the forearm or the lower leg can significantly help to maintain muscle tone & functioning ligaments & tendons that enable the client to gradually regain strength or function of the limb over time. Testing via the form of ROM & functional activities can be a better way to track success rather than via number of reps / weight achieved in the gym, particularly in the earlier stages post injury. It is much easier for an individual to progress with strength training (compared with cardiovascular training), which can provide powerful motivation for a participant who demands immediate gratification. Circuit training may be particularly useful because the variety of exercises performed. This can assist with alleviating the monotony for clients who are difficult to motivate & easily bored with one type of exercise. Flexibility: Many individuals with an ABI will suffer from ataxia, reduced range of motion, spasticity & reduced coordination. For some of these participants, stretching may be a tremendously grueling experience, even at its most basic approach. Stretching should be performed every day & as often as possible. Slow static stretching or PNF stretches will often be the most effective. Communication & Teaching Style: People with ABI may be lacking in motivation to exercise & various techniques may have to be utilised in order to get regular attendance & participation in the program. Ensure that the client understands exactly what you are asking of them. Get then to repeat it back to you or show you what you have requested. You may need to repeat yourself several times, or in different ways in order to correctly understood. Utilising all the senses is a good way to assist with cementing the learning Keep your voice tone low & unhurried. Give the client the opportunity to speak & allow them time to process what you have just said Speak clearly, use shorter & direct sentences Physically demonstrate as well as verbally explaining what is being requested. Because of common short-term memory problems, all aspects of the fitness program should be methodical & repetitive To assist with memory difficulties ensure appointments are written down in a calendar / phone as a reminder of when the next session is Using index cards that contain specific steps to follow for each set of exercises. These cards reduce the number of times the client may need to ask for help & ensures that they are doing the exercise correctly, especially if requiring to do this independently Provide regular & frequent breaks to accommodate fatigue Use wall charts & photographs to track progress & provide motivation Neurobics are mental exercises that can enhance the brain's performance. These can be incorporated into the training sessions, which help create & develop neural cells & pathways in the brain. Instead of lifting a weight from the rack with the dominant hand, ask the client to switch to using their non-dominant hand. Other examples include using a different route to get to a destination, reversing the order that you do the training session, learning a new dance / aerobics routine, closing eyes whilst performing simple exercises Safety: Specific issues with regards to safety include: Difficulties with balance & coordination. Consideration with regards to the type of exercise & amount of supervision – ie: highly choreographed aerobics classes or bike riding may not be appropriate, but tandem cycling, Pump or spin classes could be a better option Cognitive, behavioral & executive impairments. These individuals will need to receive the proper supervision & education throughout their training programs Resources & Further information: Brain Injury Association of NSW http://biansw.org.au Mid North Coast Brain Injury Rehabilitation Service Ph: 6652 2856 PSYCHOLOGICAL & MENTAL ILLNESS A mental illness is a health problem that significantly affects how a person feels, thinks, behaves, & interacts with other people. It results from complex interactions between the mind, body & environment. Factors which can contribute to mental illness are: long-term & acute stress biological factors such as genetics, chemistry & hormones use of alcohol, drugs & other substances cognitive patterns such as constant negative thoughts & low self esteem social factors such as isolation, financial problems, family breakdown or violence Approximately 1 in 5 Australians will suffer from a mental illness at some point in their lives, with anxiety & depression being the most commonly diagnosed mental illness. Mental illness may fall into two distinct categories – psychotic & non-psychotic. Diagnoses vary significantly with symptoms & degrees of severity. Some of the major types are: anxiety depression schizophrenia (psychotic) bipolar (psychotic) mood disorder personality disorders eating disorders Mental Illness Characteristics: While most people may experience strong feelings of tension, fear, or sadness at times, a mental illness is present when these feelings become so disturbing & overwhelming that people have great difficulty coping with day-to-day activities, such as work, enjoying leisure time, & maintaining relationships. At their most extreme, people with a depressive disorder may not be able to get out of bed or care for themselves physically. People with certain types of anxiety disorder may not be able to leave the house, or may have compulsive rituals to help them alleviate their fears. People with Mental Illness often have high rates of physical illness, much of which goes undetected. Some common symptoms of mental illness include: Fatigue Lack of energy Hopelessness Reduced Psychomotor skills Lack of interest or motivation Fear & low self-worth Lost touch with reality (psychotic illness) Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. Individuals with depression are typically prescribed antidepressant medication. Side effects can vary from medication to medication. They include: Headache Nausea Dry mouth Constipation Sexual problems Drowsiness Blurred vision Additional common side effects of anti-psychotic medication can include: Blurred vision Dry mouth Drowsiness Weight gain Muscle spasm or tremors Loss of menstrual periods in women Low blood pressure & dizziness Sexual difficulties Nausea or constipation These side effects are particularly prevalent when individuals are first taking the medications, & may subside after a period of time. Exercise Considerations: On average, depressed people only exercise about half as much as people who aren’t depressed. This lack of cardiovascular fitness puts a depressed person at an increased risk of heart disease. It also believed that depression & exercise influence each other – a sedentary lifestyle increases the risk of depression & depression increases the likelihood of a sedentary lifestyle. Exercise improves mental health by reducing anxiety, depression & negative mood & by improving self-esteem, cognitive function & feelings of wellbeing Exercise is especially important in patients with schizophrenia since these patients are already vulnerable to obesity, associated with antipsychotic treatment. Regular exercise can be an effective way to prevent or manage mild anxiety & depression & it has been shown that physical activity can be as effective as antidepressants or psychological treatments like cognitive behavioural therapy (CBT). Monitoring fitness gains & exercise performance throughout an exercise programme may provide positive feedback & encourage further participation for your client. It is also important to monitor their depression levels throughout exercise programmes to make sure the workload is manageable & helpful in managing the client’s mental illness. Simple strategies to assist & effectively manage some of the barriers that arise with clients with mental illness can include: Schedule exercise sessions for earlier in the day as opposed to evening after a full day of work has occurred Find a form of physical activity that is enjoyable to the individual Find a picture or word that is motivational to the client & hang it in a visible place Encourage the individual to share their physical activity plans with a friend or family member who can help with motivation, or train in a small group whereby motivation & accountability can be pursued with others in the group Vary physical activity & keep it fun to prevent boredom Create a training log & get the individual to complete this each week & return to you Work together to create realistic goals & write them down, along with a rewards system for achievement Implications for Trainers: A single session of exercise can result in reasonably large mood benefits, including: Increases in positive mood states Decreases in negative mood states Positive well-being Vigor, more refreshed, elation, feeling upbeat, happy or enthusiastic Peaceful, calm or relaxed To reap the psychological benefits of exercise, there are some key points to remember: To feel better after exercise a 10-15 minute walk is sufficient To feel better during activity, exercise for longer periods. It is better to walk for 45minutes (even at a lower intensity) than for 20 minutes The largest improvements are often made on the days that the individual feels least positive prior to exercising General Exercise Guidelines for Individuals with Mental Illness Many different forms of physical activity have proven effective with reducing the symptoms of mental illness. The physical activity programme undertaken by a client suffering from mental illness, should be tailored to their individual preferences. It is recommended that the person undertake a full pre-exercise questionnaire & testing before commencing any training, particularly if there is a possibility of other co-morbidities. One of the most important considerations when building the exercise program for this population is to make it fun & interesting for the client whilst keeping all activities & goals achievable. It may also be beneficial to introduce new exercise settings to encourage & motivate the client as well. Successful exercise programmes give the client a sense of achievement, mastery & build confidence. The program needs to be flexible in order to encourage & challenge the participant through normal exercise adaptions. Cardiovascular Exercise: With regards to reduction in symptoms, evidence is strongest for aerobic activities such as walking, running, cycling, swimming, & exercise classes – rather than anaerobic activities (such as weight training). Although a 10-15 minute walk can result in mood improvements, most mood improvements aren’t detectable until 25-40 minutes of physical exertion, where people will feel less tense, more clearheaded, more elated – less depressed, & more energetic. Strength Training & Flexibility: Whilst evidence is strongest for cardiovascular exercise with regards to reduction of symptoms associated with mental illness it is important to develop a well-rounded exercise program for your client, including strength & resistance training & flexibility if appropriate. Communication & Teaching Style: Be respectful to the person. When someone feels respected & heard, they are more likely to return respect & consider what you have to say. If they are experiencing events like hallucinations, be aware that the hallucinations or the delusions they experience are their reality. You will not be able to talk them out of their reality. They experience the hallucinations or delusional thoughts as real & are motivated by them. Communicate that you understand that they experience those events. Do not pretend that you experience them. Some people with paranoia may be frightened, so be aware that they may need more body space than you. Do not assume that they are not smart & will believe anything you tell them. Mental illness has nothing to do with the person's intelligence level. Do not lie to them, as it will usually break any rapport you might want to establish. If needed, set limits with the person as you would others. For example, "I only have five minutes to talk to you" or "If you scream, I will not be able to talk to you." Call for help (police, security, or colleagues) if you feel physically threatened or need help deescalating the person. Safety: Tailor exercises to account for possible drug side effects (eg: if experiencing blurred vision, do activity indoors or exercise outside with supervision or in low traffic areas). If you think the client is in crisis & you have concerns about their safety, call emergency services (triple zero – 000), contact their doctor or local mental health service. Do not leave the person alone, unless you are concerned for your own safety. Resources & Further information: Beyond Blue Lifeline Kids Helpline Headspace http://www.beyondblue.org.au/ https://www.lifeline.org.au/ Ph: 13 11 14 http://www.kidshelp.com.au/ http://www.headspace.org.au/ Ph: 1800 55 1800 SPINAL CORD INJURY Spinal cord injury (SCI) is damage to the spinal cord that results in a loss of function such as mobility or feeling. It’s a permanent and irreversible injury. The extent of dysfunction depends on the location of the injury. Quadriplegia (also referred to as tetraplagia) is loss of function below the neck (paralysis of the four limbs & trunk musculature) Paraplegia is loss of function below the chest (usually resulting paralysis of the legs & hips & in some cases the trunk) Spinal cord injuries may be caused by trauma (eg: motor vehicle accidents, falls, highimpact sports injuries & diving accidents) or disease (eg: polio, spina bifida, multiple sclerosis). Fitness plays a vital role in helping the spinal cord patient live a fairly functional existence. Spinal Cord Injury Characteristics: No two spinal cord injuries are the same & what happens with one person does not necessarily happen with another. Some general characteristics include: Movement may be lost below the level of the injury Sensation may be lost below the level of injury Blood pressure & circulation may be altered Breathing dysfunction especially in those with cervical or thoracic injuries. Temperature control may be affected, including sweating & shivering Bladder & bowel function dysfunction There may be spasms or involuntary movement below the level of injury Sexual dysfunction Fertility may be affected Other medical issues can include: Osteoporosis & Fractures may occur due to lack of use, particularly in the legs Changes in blood pressure. Hypotension (low blood pressure) usually occurs when the patient changes his body position too quickly Autonomic dysreflexia – a reflexive response to a distended bladder, fecal mass, pain or heat & resulting in pounding headaches, anxiety, sweating, chills, hypertension & the like. This is a medical emergency & life threatening. Medication It's important to understand the effects that medication have on the body in relation to exercise. Medication may affect or impair the ability to exercise. It is important to get a comprehensive list of all medications prior to starting any exercise program. Exercise Considerations: Individuals with spinal cord injuries can experience numerous benefits from regular exercise, which may include: Prevention of secondary conditions such as cardiovascular disease, diabetes, pressure sores, carpal tunnel syndrome, chronic obstructive pulmonary disease, hypertension, urinary tract infections, & respiratory disease Prevention of deconditioning & obesity Psychological &/or recreational benefits Issues most related to exercise are: Incontinence - Individuals with lesions above the sacral level experience a loss of control with their bowel or bladder o Ensure the client has an empty bowel & bladder before starting exercise. Spasticity - This condition is characterized by high muscle tone & hyperactive stretch reflexes. It typically occurs in the muscles below the site of injury & is exacerbated by exposure to cold air, urinary tract infections & physical exercise. o The spastic muscle groups will need to be stretched often Autonomic Dysreflexia - A sudden rise in blood pressure resulting from an exaggerated autonomic nervous system response to noxious stimuli below the level of injury, usually due to bladder/bowel overdistension or blocked catheter. Symptoms include profuse sweating, sudden elevation in blood pressure, flushing, shivering, headache, & nausea o Medical attention may be needed if this occurs. Orthostatic hypotension - A drop in blood pressure (greater than 20 mmHg for systolic blood pressure & greater than 10 mmHg for diastolic blood pressure). It occurs in upright postures, especially moving from supine to upright sitting/standing/head-up tilt. Symptoms include nausea, dizziness & lightheadedness o blood pressure might need to be monitored throughout exercise o avoid quick movements o maintain proper hydration o use compression stockings & an abdominal binder o If orthostatic hypotension occurs, lie in a supine position with feet elevated Thermoregulation - Irregular body temperatures are often experienced by individuals with SCI. o ensure appropriate clothing worn o drink plenty of fluids o in warm environments a fan & water spray can aid in cooling o in cold environments, ensure extra layers worn Pressure sores - Damage to the skin or underlying tissue caused by prolonged sitting, using old wheelchair cushions, sitting on hard surfaces, shear forces or as a result of a fall o perform wheelchair push-ups or pressure releases often Transfers o Be sure to follow appropriate guidelines Balance o Use straps or other physical assistance to hold the trunk in position during upright exercise. Implications for Trainers: The trainer should be aware of the level of lesion & any side effects or medical issues the client may have. Also be aware of how to transfer the client appropriately – you may need to get assistance / training from their carer initially to ensure you can do this competently & effectively. As the majority of SCI clients are wheelchair bound sessions will need to be wheelchair accessible. If training outdoors ensure the client brings the appropriate wheelchair. There are also chairs that are suitable for going on the beach or rough surfaces. General Exercise Guidelines for Individuals with a Spinal Cord Injury Some exercises provide greater benefit for persons with SCI than others. These include: Aerobic exercise to maintain cardiovascular health & prevent secondary conditions Strength training to maintain & improve the ability to perform activities of daily living & mobility, to aid in transfers, & to prevent injury through muscular balance Flexibility training to improve range of motion & reduce spasticity Cardiovascular Exercise: Quadriplegia MHR typically does not exceed 100 to 125 bpm, & training intensity should be between 50% & 70% maximal heart rate. Arm ergometry is often a preferred type of exercise training for individuals with quadriplegia. Be sure the wheelchair is locked, the hands are secured to the equipment (straps can be used for stability & balance) & the ergometer is in a fixed position. Other forms of aerobic exercise may include pushing their chair or a track chair & hand cycling. The MHR of individuals with paraplegia is also suppressed, however, for lesions below T6, the MHR is closer to the age-predicted maximum. Training intensity should not go above 70%. Types of cardiovascular training that benefit individuals with paraplegia are wheelchair ergometry, upper-body calisthenics, rowing machine, recumbent steppers, handcyling, sports such as basketball, track, swimming, quad rugby, & functional electrical stimulation-leg cycle ergometer. Strength Training: Training sessions should be held regularly. Refrain from training the same muscle groups on consecutive days. Upper-body pushing & pressing exercises (bench press, overhead press) will help transfers & wheeling, while pulling/rowing exercises will help prevent shoulder overuse injuries & improve sitting posture. Wheelchair push-ups are great to assist with transfers. Use straps or a partner for stabilization & balance. Vary exercises to reduce over-use injuries & emphasize muscle groups that are still functional. Types of strength training that benefit individuals with SCI are free weights, weight machines, medicine ball, wall pulley, cable columns, & theraband. Flexibility: Flexibility training is important to prevent contractures (permanently shortened muscles), particularly in the hip area. Paralyzed muscles should be passively stretched, specifically, the hamstrings, adductors, hip flexors, plantar flexors, & lumbar extensors. Types of flexibility training are: Passive & active resistance Theraband Standing in a standing frame (if not medically contraindicated) Standing may also help to maintain muscle bulk & may help with reducing loss in one density in your lower limbs. Equipment such as tilt tables can help standing safely with support. Communication & Teaching Style: Most individuals with SCI do not have any difficulty with communication nor do they have any intellectual or leaning difficulties. Safety: If the individual is starting physical activity, it is important to check with their GP to determine if there are any activities they should avoid. If it has been a long time since they last stood, they may require a bone density test to determine if it is safe to do so. Regularly monitor blood pressure, heart rate, RPE, & symptoms. Stop exercising if the individual feels pain or discomfort. Don't exercise if they are ill (i.e., cold, flu, bladder infection, pressure ulcer, unusual spasticity). Check medications & their effect on exercise tolerance. Often a client with SCI is self-sufficient with their wheelchair mobility, but ensure that the brakes are locked on wheelchair & ensure adequate safety measures if training outside, particularly in high traffic areas or on sloped surfaces. Resources & Further information: ParaQuad Spinal Cord Injuries Australia www.paraquad.org.au https://scia.org.au/ Spinal Cord Injury Network http://www.spinalnetwork.org.au/ Spinal Injuries Australia http://www.spinal.com.au/ BLINDNESS & VISUAL IMPAIRMENT Blindness & low vision can occur as a result of a number of different diseases, conditions or accidents. Some eye conditions are congenital, others are caused by a disease or infection & others can be caused by accidents or through over-exposure to UV light or chemicals. Many of the most common eye conditions have no known cause. Visual Impairment Characteristics: The range of vision impairment can vary greatly from loss of near / colour vision, difficulty seeing in dim lit situations to total blindness. Medication Most people with vision impairment do not require any specific medication to manage this condition. As with all populations it is imperative to be aware of any medication they may be taking & the impact this may have on their safety & exercise performance. Exercise Considerations: People with visual impairment may be prone to lower levels of fitness compared to their sighted peers. Issues most related to exercise are: Inaccessible exercise equipment & programs Decreased safety with navigating their way around a gym or using equipment safely Lighting – may need to conduct sessions in brightly lit gym or during sunny daylight hours outdoors Implications for Trainers: The first step in exercise for the blind, like exercise for the general population, is to assess the individual needs of the person. A person who is totally blind & cannot relate to visual descriptions needs to be taught exercise activities differently from someone who has some useful vision. For example, an aerobics instructor may have to use touch to demonstrate a movement. Visually impaired persons with even a little useful vision may be able to grasp at least some visual concepts, but this should not be assumed. Safety is a big issue that will need to be taken into consideration in each & every session. General Exercise Guidelines for Individuals with Vision Impairment If there are no other limiting factors or secondary diagnoses, the rules for exercise prescription intensity can be the same as the general population Cardiovascular Exercise: Walking & Running: There are several strategies commonly employed to provide guidance to people with Vision Impairment. Running outdoors: Sighted guides are commonly used. The visually impaired runner holds the elbow of the guide, who should be the faster of the two. A guide rope may be used. Ropes can be placed around a track, gym floor or even a backyard. This frees the blind person from dependence on a guide for exercise. Running on a treadmill: Any person with or without a visual impairment can run on a treadmill. It is recommended that the individual start out slowly to get a feel for the motion & use the handrails. Cycling: Stationary Cycling: A stationary bike may be used & requires no modification & little instruction. Independent Cycling: Individuals who have some usable vision may be able to ride a bicycle independently in a quiet park or around a track. It is always safer if there are peers or individuals with sight close by to ensure safety. Tandem Bicycles: Tandem bikes allow the sighted participant to ride in the front of the bike, while the participant who is visually impaired or blind rides in the back. The person in front is responsible for steering & stopping. When riding be sure to develop specific signals for turning, stopping, or emergencies. Bicycle stand / wind trainer: Bicycle stands can turn an ordinary road bike into a stationary bike. Swimming: Swimming is one of the best activities for individuals who are visually impaired or blind. There are few barriers, & the swimmer can move freely without worrying too much about obstacles. Instructors will need to demonstrate techniques via touch. For example, an instructor may use her own body to demonstrate a stroke while a blind student follows the arm motion with his fingers. Students also have to learn to use lane dividers & pool walls to stay oriented. If swimming in open water, a tether / guide rope attached to another person or a stronger swimmer staying nearby will be required General Sports: Exercise for a blind person need not be limited to basic workouts. Once a visually impaired individual has achieved a good level of physical fitness, a wide range of competitive sports is available. Aerobics: Many visually impaired people participate safely in aerobics classes. The initial routine may have to be taught or described by a helper, but after that the participant can participate independently. The participant can include an 8 count or a 4 count routine & combine different moves. Flexibility: Yoga: The life of an individual with a visual impairment can often be very stressful. Yoga has many advantages including weight loss, muscular strength, flexibility, & most importantly, relaxation. Once yoga moves are learned the participant can train in the home or yard alone or with friends & family. Balance: People with visual impairment have a higher risk of falling compared to people without visual impairment. Since balance programs have been demonstrated to reduce fall risk it is essential to incorporate a balance component into the exercise program. Balance may be improved by working on lower extremity strength, such as squats, lunges, hip flexion, & knee flexion/extension. Flexibility on lower extremities should also be performed to ensure adequate walking-mechanics to avoid obstacles & everyday situations. Such flexibility exercises may include working on toes or heels. Stance positions are a great way to challenge the different sensory mechanisms incorporated with balance (vision, proprioception, & vestibular function). Stances that can be performed include: single leg, tandem, wide, narrow, & stagger stance. Gym based equipment / Environmental modifications Pictorials/Braille instructions: Allow time for the person to look at performance pictorials &/or the opportunity to read about it. Use large print Braille on/off switches. Visual perimeter: For safety, mark the perimeter of the exercise machines with rope or contrasting colored tape on the floor. Record performance: The participant should have some way of recording number of repetitions & weight on each exercise Vibrating timers can be worn around the neck or in the pocket. Cardiovascular Machines Issues: The display screens often have poor contrast or reflective plastic coverings that cause a significant amount of glare The flat panel controls are also often labelled in small fonts & poorly contrasting colours &, like the visual displays, are covered in highly reflective plastic A green Start button & a red Stop button are common on many exercise machines; although colour indicators such as these are helpful to people with low vision, the ability to start & stop the machines does not create accessibility Modifications: Handheld magnifier or reading control labels & visual displays Placing braille or other tactile markings on the various controls on the flat panel Using spin bikes with mechanical knobs to increase or decrease the resistance of the bikes' pedals, not having to use visual display screens Ensure well lit gym areas Weightlifting Machines Issues: Unable to read weights on plates Unable to determine weight of free weights Tripping over weights left lying on floor Modifications: Marking plates / weights with braille Teaching the client the weight of each plate & showing them how to manually count down the plates to the correct weight they require Using pneumatic system Ensuring free weights are placed into a specific order according to weight Educating clientele on putting weights / equipment away when finished & monitoring that this occurs When purchasing new equipment consider equipment with markings / adaptations for people with disabilities / vision loss (ie: tactile discernable control, larger labels on controls & higher-contrast colours on pedals, handgrips, larger-font, easier-toread visual displays) Ensure well lit gym areas Communication & Teaching Style: A person with a visual impairment is unable to pick up on many non-verbal communication cues. Make sure you describe to them what is happening throughout the session Avoid standing near windows or spaces with glare, as this will impede their ability to see you When introducing an individual to a new machine, allow time for tactile &/or visual exploration. The instructor should demonstrate the movement & link the movement to language, including the name of the exercise & muscle involved. Provide any written material in larger fonts & if printing in colour choose colours that contrast strongly with each other Safety: A lot of strategies to ensure safety of clients with vision impairments have been addressed above. Fall-risk is the highest safely concern, particularly in older adults with a visual impairment. Ensure the environment is safe for the person with visual impairment. Guide them around the gym / workout area. Remove any clutter & have the area set up the same way each session so the client can familiarise themselves with the layout Ensure adequate supervision, especially in the early stages until the client is comfortable with the exercises & familiar with the environment Resources & Further information: Vision Australia http://www.visionaustralia.org/ Royal Institute for Deaf & Blind Children http://www.ridbc.org.au/blindness ADAPATIVE EQUIPMENT AND ASSESSMENT TOOLS ADAPTIVE EQUIPMENT & ACCESSIBILITY One of the major barriers to access for people with disabilities is inaccessible exercise equipment. Gyms often have obstacles, such as stairs preventing disabled members from reaching parts of the club, and others lack equipment that could be used by people with disabilities or staff members who are willing to help such members. There are various simple ways to ensure that the gym environment is accessible & numerous different types of adaptive equipment & aids that can assist with people with disabilities. Some of these solutions are commercially manufactured; others are very simple & require a slight adaptation or different way of thinking when using a standard piece of equipment. Access: Access routes free from obstacles Wheelchair accessibility – including lift access if needed Routes clearly marked, including Braille Large turning circle for moving and transferring next to equipment Large turning space between rows of equipment Gym Environment & Equipment Minimise trip hazards & put away all equipment after use Provide space for mobility objects and service animals next to machines Handles and grips for transfer/ support Removable and adjustable seats to help with people who use wheelchairs Keep equipment and objects in the same place Machine may need to be labelled with pictures, braille & large print words Large green start button & a red stop button on exercise machines Bright / adequate lighting, including access to darkened cycle rooms Use of technology (applications for I Pads and I Phones) Marking the perimeter of the exercise machines or designated area with contrasting colored tape on the floor Change rooms / showers Provide space for mobility devices and service animals Accessible shower, toilet, locker, changing area, sink, and water dispenser Entrance doors and stall doors have low knobs or handles, or are automatic Assistance Animals A Guide Dog or Service Dog is a vital means of independence for many people living with a disability. It is illegal to discriminate against or refuse entry to a person with an Assistance Dog and anyone who does so can be prosecuted. SPECIALISED EQUIPMENT: People with disabilities will often require specialised equipment or modifications to standard equipment in order to allow them to safely & effectively use it. Cuffs, Velcro Straps & Gripping Gloves Useful for quadriplegics, paraplegics, and individuals with compromised grip and cerebral palsy Velcro gloves can be used to attach the hands to equipment Use with bats, racquets, mits etc Wheelchair gloves Great for propelling wheelchair, allowing speed & quick movements whilst decreasing risk of injury to hands Cuff weights Can add resistance to movements & allow people with reduced grip be able to safely perform resistance exercises Auditory / noise balls Allows participant to hear rather than see ball Arm Cycle Large free standing machines Smaller table top models Great for warm ups, loosening shoulder joints, improving circulation & upper body fitness Pedal Straps For bikes to keep feet attached to pedals Flotation Devices To improve buoyancy in water Kickboards, water running / floatation belts, buoyancy vests Theraband Resistance varies according to colour Medicine Balls With or without handles Can use with gripping gloves if hand function is limited Heavy bag / speed ball with stand Able to use these whilst seated in a wheelchair Lower / raise speed ball to various heights to allow for different styles of boxing Can do a very similar boxing workout to able bodied participants, with the ability to incorporate a wheelchair bound participant into a mainstream class Gym Equipment Pro Gym CT - all in one system allows for paraplegic, quadriplegic, and able bodied athletes to get a total body workout. Cybex - various cardiovascular and strength training equipment for people with disabilities (PWD). The Arc Trainer allows for a cardiovascular workout for PWD’s Funding There is often government & non-government funding & support available for both individuals with disabilities with disabilities, or organsiations who are wanting to make changes to allow access & integration of people with disabilities. The Aids and Equipment Program is a NSW Government initiative to assist eligible residents of NSW, who have a life-long or long-term disability, to live and participate within their community by providing appropriate equipment, aids and appliances. http://www.enable.health.nsw.gov.au/aep Resources & Further information: Independent Living Centre http://ilcaustralia.org.au Technical Aid to the Disabled http://www.tadaustralia.org.au Australian Institute of Sport (Inclusive Coaching) http://www.ausport.gov.au/participating/coaches/tools/coaching_specific_groups/Inclusive D-Ability http://www.d-ability.org Able Data www.abledata.com Physiotherapy Exercises https://www.physiotherapyexercises.com (A free tool to create exercise booklets for people with disabilities) Opening Doors http://www.ausport.gov.au/__data/assets/pdf_file/0004/448645/Opening_Doors.pdf Online equipment suppliers Achievable Concepts Adaptive Sports Equipment FAS Therapeutic Equipment Active Hands Infinitec The Hand Cycle Store http://www.achievableconcepts.com.au http://www.adaptivesportsequipment.com http://www.fasequipment.com www.activehands.co.uk http://www.infinitec.org http://bike-on.com ASSESSMENT TOOLS Assessing physical fitness with a person with a disability can pose various challenges, including: inability to complete usual fitness tests due to restrictions difficulty with comparing results to normative data impact of various medications on results Goals: Often exercise based goals for people with disabilities can be quite different than their able bodied counterparts. They may be more functional & less aesthetic, such as: Improve co-ordination & general function Be able to complete a specific task or activity (eg: able to get self in & out of bed, catch a wave with a boogie board) Used as a social outing & community participation Freedom of movement (eg: when in water) Feeling like a ‘normal’ person & doing what they do Questions….. What is the goal of the client? What is the goal of your training program? How are you going to achieve this? Considerations when assessing & designing a program Look at client’s functional abilities (outside of gym), as well as fitness based tasks Look at activity preferences, family engagement in social & recreational activities, & family activity preferences Determine what modifications will need to be made to ensure effective delivery & outcome of program, including: o Communication, language & literacy skills o Physical limitations – access, modification to exercises o Psychological considerations – best time to attend gym, cancellation policy o Medical – is clearance required Assessment A person with a disability should undergo a thorough physical fitness assessment prior to commencing a fitness program. This should include the same core components that their able bodied companions would complete. Adaptations to the standard assessment format will need to be undertaken to ensure a holistic assessment & functional results. Assessment of physical activity & fitness can be determined using a variety of strategies, including direct observation, self-report measures, electronic monitoring & physiological measures Liaison with treating doctor, therapist, family members & carer is invaluable The assessment tool should be valid, reliable & objective Less likely to be able to score against general population norms o Various norms available for people with disabilities o Data also used for baseline information & comparison at each re-test Include health status, secondary health issues, medication as often this will change before ‘fitness’ levels May need several sessions & observations to get a good overall assessment Task Analysis – break down activities to work out core issues / areas that need to be focused on for greatest improvement MODIFICATIONS TO STANDARD FITNESS TESTING Traditional Assessments Modifications & Considerations Health Screen - Questionnaire - Resting Heart Rate - Blood Pressure - Medication Provide questionnaire to client prior to appointment to get filled out before session & include authority to talk with doctor / therapist etc if needed Talk with carer & get a history of medication & recent BP & HR recordings Talk with doctor & see if any long standing issues Nutrition & Lifestyle - Food diary Talk with carer / family member Body Composition - Skin folds - BMI - Height & Weight Skinfolds - Measurements should not be taken at sites with scar tissue, at sites where injections have been received repeatedly, or on limbs that have muscular atrophy. - In some instances, it may not be possible to attain skinfold measurements at a site - often difficult to measure in people who are obese due to the difficulty in finding the landmarks, & due to callipers not able to record large numbers. Consider additional girth measurements until accurately able to measure skinfolds Height - individual who wears prosthetic devices or braces should be measured whilst they wear the items - Clients who are unable to support their body weight in a standing position can lie on a mat while body length is measured with a tape measure. - Liaise with doctor or carer to obtain height Weight - If wearing a prosthetic device or brace, weight is taken with the items removed or by subtracting the weight of the item. - In in a wheelchair, weight can be determined either by taking the individual out of the wheelchair or by weighing the individual in the wheelchair & then subtracting the weight of the wheelchair Aerobic Capacity Blind – run with a partner, guide rope or wire - Timed walk /run Beep test Step test Intellectual - take additional time to explain & check understanding Hearing Impaired – visual cue (flashing light) to indicate timing / pacing Wheelchair – find a big hill! Use flight of stairs with handrails for safety & balance Allow practice sessions, including listening to any audio, to ensure comfort & minimise stress If unable to walk / run change to a swim, cycle or hand ergometer test Use modified standardised tests (see below) Muscular strength - Bench Press - Military Press - Push Ups Intellectual – check understanding on how to perform the test. Take whatever time is necessary for the participant to learn the test Participants can be held or secured as necessary & appropriate for stability Stay within the client’s range of motion. If complete elbow extension is not possible due to impairment, record a successful lift each time the participant lifts the weight with his or her maximal elbow range of motion Choose machines / exercises that the client can safely use & use these for testing each & every time. To measure leg strength you may wish to perform a 1RM seated leg press, & for upper body strength a wall push up test or repetition max bench press may be suitable Use a grip dynamometer to assess & record grip strength • Visual - Considerable time is required to teach the test to individuals with visual disability if they have not already learned how to perform a push-up. Provide tactual or kinesthetic cues to help participants know correct arm positions & recognize a straight back during the push-up To help participants learn the exercises, (eg: pushup) have them watch themselves in a mirror Seated push up in chair Core - Curl ups - Plank Use a pressure biofeedback unit Modified plank position Supine single leg lift STANDARDISED TESTS: Wheelchair Aerobic Test Aerobic fitness test for wheelchair users 400m running track, recording distance over 12 minutes Rockport Walk Test Aerobic fitness test for those of low fitness level, calculates rough VO2max Time taken to complete 1 mile. Recording of heart rate upon completion 2 Minute Step in Place Test Alternative to the 6 minute walk test for people who use walking aids or who have difficulty balancing. Client marches in place, next to wall, raising knee to pre-determined height. Can hold onto wall for support 6 Minute Walk Test Aim is to walk as quickly as possible for six minutes to cover as much ground as possible. Can walk outside or on treadmill Astrand-Rhyming Cycle Ergometer Test Submaximal cycle ergometer aerobic fitness test Uses cycle ergometer, with client pedalling at a constant workload for 7 minutes. Heart rate is measured every minute, & the steady state heart rate is determined. Variations of the Beep Test There are many variations of the standard 20 metre beep test Multistage Field Test (MFT) for wheelchair users o Wheelchair version of the beep test o 15 m x 15 m square, with each corner modified to create a long turning zone, avoiding necessity to make a sharp 90 degree turn Williams Swimming Beep Test o The test is based on a 1500m swim. The 1500 is broken down into 15 x 100, each 100 is then broken down into 8 x 12.5m swims. 10m Shuttle Test o Aerobic fitness test designed for children with cerebral palsy (CP). Variation of the 20m beep test 10m Incremental Shuttle Walk Test (ISWT) o Aerobic fitness test designed to assess functional capacity of patients with COPD. This test is a variation of the 20m beep test Groningen Walking Test o Adapted in order to suit an elderly population. Modified to eliminate the sharp turns at both ends of the 20m shuttle may strain the knees & joints of the elderly participants. HOLISTIC ASSESSMENT & TRACKING Area of testing General observations & feedback Medical & Health Energy levels Sleep patterns Health complaints Medication Weight Foods eaten Self Care Performance of ADL’s Assistance Required Mobility & Balance Gait pattern Use of mobility aids Need for physical assistance Ability to transfer Walking up stairs, hills, uneven ground Social outings Trips or falls sustained Strength Performance of tasks at home Cardiovascular Energy levels Naps / rests required during the day Flexibility Functional tasks – can reach to shoulder but not overhead (can’t reach top shelf in cupboard) Sport Specific Throwing, catching & bouncing ball Running & jumping Forward, backward, lateral movement Fitness, endurance & speed Psychological Attendance / cancellation of sessions Behaviour Emotional upsets Mood swings Change in medication Resources & further information: Brockport Physical Fitness Test (BPFT) A criterion-referenced health-related test of physical fitness, appropriate for use with young people with disabilities Physical Activity Scale for Individuals with Physical Disability (PASIPD) Top End Sports http://www.topendsports.com/testing/specific-groups.htm# Physiotherapy Exercises https://www.physiotherapyexercises.com (A free tool to create exercise booklets for people with disabilities) Australian Institute of Sport (Inclusive Coaching) http://www.ausport.gov.au/participating/coaches/tools/coaching_specific_groups/Inclusive TASK ANALYSIS How to write a Task Analysis 1. Write down steps 2. Have someone perform it 3. Watch others and research 4. Do the task 5. Watch your client perform the task 6. Adjust analysis to include missing steps TASK ANALYSIS TASK Participate in Deep Sea Fishing LEARNING CONSIDERATIONS Intellectual Disability PREREQUISITE SKILLS OBJECTIVE 1. Able to tread water for 10 mins in life jacket and clothes unaided 2. Cast a rod while standing Safely participate in deep sea fishing excursion RELATABLE SKILLS 1. Comfortable in deep water 2. Knowledge of fishing equipment and their use gained from beach fishing 3. Experience of open water from Harbour ferry trip in Sydney BARRIERS 1. Cannot tread water for extended period of time ADAPTIONS / SOLUTIONS 1. Build on existing water skills with time in water, initially local swimming pool then open ocean in The Jetty area. 2. Engage a swimming instructor to assist with water skills and to increase confidence around open water 3. When beach fishing, practice casting rod while standing instead of using current preferred method of sitting 4. Time on fishing boat in a moored situation 5. Spending time at Deep Sea Fishing Club on fishing mornings to become familiar with routines prior to first outing EQUIPMENT COMMUNITY ENGAGEMENT Life jacket 1. Deep Sea Fishing Club member to assist with familiarisation of boat, club activities and provide life jacket or information to enable purchase of a jacket 2. Swimming Instructor from local swimming pool 3. Personal trainer from local gym to assist with overall fitness eg increase in cardio capacity and upper body strength INCLUSIVE COACHING INCLUSIVE COACHING Good coaches adapt and modify aspects of their coaching to create an environment that caters for individual needs, allowing everyone to take part and experience success within the activity. The onus of inclusion rests with the coach. Many people think that you need special skills or knowledge to coach participants with a disability. This is not the case. The basic skills of good coaching, when applied with an inclusive philosophy, will ensure that all participants including people with disability can participate. Qualities and skills of an inclusive coach Qualities Attributes Patience Recognising some participants will take longer to develop skills or make progress than others Respect Acknowledging difference and treating all participants as individuals Adaptability Having a flexible approach to coaching and communication that recognises individual differences Skills Attributes Organisation Recognising the importance of preparation and planning Safe practices Ensuring every session, whether with groups or individuals, is carried out with the participants’ safety in mind Knowledge Utilising knowledge of training activities and how to modify them in order to maximise the potential of every participant Planning for inclusion When preparing a coaching program, examine what, if anything, needs to be adapted or modified. Two strategies coaches can use when planning and conducting activities are TREE and CHANGE IT. By modifying the factors listed, coaches can meet the individual needs of the participants. TREE T Teaching / Coaching Style R Rules / Regulations E Environment E Equipment CHANGE IT Example C Coaching Style Demonstrations, use of questions, role models, verbal instructions H How to Score Rules A Area Size, shape or surface of the playing environment N Numbers Number of participants involved in the activity G Game Rules Number of bounces or passes E Equipment Softer or larger balls, or lighter, smaller bats/racquets I Inclusion Everyone has to touch the ball before the team can score T Time ‘How many … in 30 seconds?’ Sports CONNECT Coaches looking at furthering their knowledge in inclusive coaching can contact their sport or attend Inclusive Coaching workshops as part of Sports CONNECT Education. For more information visit: ausport.gov.au/disability Tips for coaches working with participants with disability • The basic principles of coaching apply when coaching participants with disability. • Accept each participant as an individual. • Ask the participant what they are able to do; the needs, strengths and weaknesses of individuals will differ. • Assess each participant’s aspirations, needs and ability and plan a training program accordingly. • Understand how the impairment (disability) affects the participant’s performance; it is not necessary to acquire extensive knowledge of the disability. • Set realistic and challenging goals as you would for all participants • Be aware of the risks associated with all participants in your care, and be prepared to deal with emergencies should they arise. ausport.gov.au/coach © Australian Sports Commission 2010 FACT SHEET INCLUSION IN SPORT Inclusion of people with disability is about providing a wide range of options Being inclusive is about providing a range of options to cater for people of all ages, abilities and backgrounds, in the most appropriate manner possible. Inclusion encompasses a broad range of options in many different settings. The inclusion spectrum A common misconception about inclusion is that it is solely about including people with disability in regular sport activities without any modification. Inclusion encompasses many different options in different settings. Inclusion in sport can be viewed in terms of a spectrum. Each section of the spectrum is as important as the next, and ideally there would be programs for people with disability available in all sections to choose from. Examples of the inclusion spectrum • No modifications: an athlete with an intellectual disability may train and compete with athletes without intellectual disability at a local swimming club • Minor modifications: a vision impaired tenpin bowler using a rail for support • Major modifications: a seated shot-putter competing under separate rules using modified equipment against other athletes with disability in an integrated track and field competition • Primarily for people with disability: athletes with disability and their able-bodied peers combine to form teams for the purpose of developing a wheelchair basketball competition • Only for people with disability: goalball players participating in a competition exclusively for people with vision impairments • Non-playing role: people with disability can be officials, coaches, club presidents, volunteers and spectators. The following factors will influence the section/s of the spectrum an individual chooses to participate in: • their functional ability • the sport in which they are participating • the opportunities within their local environment • their personal preferences. The inclusion spectrum allows games and activities to be delivered in different ways, with more options. The aim is to encourage higher quality participation by people with disability, both with or away from their able-bodied peers. Clubs can provide a range of options by adapting and modifying their sport in different environments. ausport.gov.au/disability INCLUSION TIPS: ADAPTION & MODIFYING The effective teaching of skills and techniques are equally important for bowlers with a disability. People with a disability do not generally need to be treated differently to anyone else who participates in bowling. As a coach, leader or teacher you are in a great position to ensure that you take an inclusive approach. To do this you can use the TREE principle. The TREE principle can be used as a guide to modifying your activities and sessions so that you can be inclusive of not only people with a disability but people of all abilities. Teaching or Coaching Style: What can I modify about the way I am teaching / coaching? Think about how your methods can make the most of the abilities within the group. Rules and Regulations: What can I modify in the rules or regulations? Rules and regulations can be modified to ensure someone can participate. Equipment: What can I modify about the equipment used in the session ? Equipment can include things such as bumpers, guide rails, ramps, ball handles etc. Changing or including equipment in a session may allow a bowler to make the most of their abilities Environment: What can I modify about the environment to ensure no one is left out? Think about where your bowlers are positioned on the lanes or how easy is it to move around the approach. More information on the TREE principle can be found on the following web pages: Australian Sports Commission: www.ausport.gov.au/disability VicSport: www.vicsport.asn.au SPORTING ORGANISATIONS SPORTING ORGANISATIONS CATERING TO PEOPLE WITH DISABILITIES Australian Sports Commission http://www.ausport.gov.au http://www.ausport.gov.au/__data/assets/pdf_file/0004/448645/Opening_Doors.pdf Developed or supported national sporting organisations, state departments of sport and recreation and Sporting Wheelies and Disabled Association to develop programs and resources to assist sporting organisations and schools to create safe, fun and inclusive sport environments. Burn Rubber http://www.pcycnsw.org/prime_sparts_burn_rubber A health and fitness program developed for individuals with a physical disability. Operates within the PCYC across metropolitan Sydney. Community Care Options http://cco.net.au/community/connectable/community -directory Links to the list of partners in the ConnectABLE project. These clubs & groups have expressed their commitment to social inclusion and being accessible to everyone in the community. Disability Sports Australia http://www.sports.org.au/index.php Australia's peak national body representing athletes with a physical disability. Provide opportunities for development of athletes at a national level and supporting pathways from grassroots to national level. Administer the Wheelchair Rugby and Wheelchair Basketball National Leagues, and the Lawn Bowls Multi-Disability National Championships Disabled Surfers Association of Australia http://disabledsurfers.org The DSA is setting the world’s best practice for the sport of Disabled Surfing. Caters for all disabilities. Currently 15 branches across Australia and New Zealand. Disabled Wintersport Australia http://www.disabledwintersport.com.au DWA is an organisation with a national perspective taking responsibility for development of disability winter sport in Australia. The organisation has assisted thousands of individuals with disabilities to participate in winter sports annually. The organisations members range from recreational skiers to Australia’s Winter Paralympians. Gymbaroo http://www.gymbaroo.com.au Group exercise classes for young children based on sensory and movement experiences required for healthy brain development. NICAN http://nican.com.au Information on recreation, tourism, sport & the arts for people with disabilities. Funded by the Australian Government. Rainbow Club Providing swimming lessons for children with a disability. Located throughout NSW. Reclink http://www.reclink.org Reclink is a non profit organisation whose mission is to provide and promote sport and art programs for people experiencing disadvantage Riding for the Disabled (NSW) http://www.rdansw.org.au Provides supervised access to horse riding for people with disabilities at 38 centres throughout NSW. Sailability http://www.yachting.org.au/participation/sailability http://www.sailabilitynsw.org An entry level program for people of all-abilities to get into sailing and activities at clubs. Special Olympics http://www.specialolympics.com.au Special Olympics provide sports opportunities for all people with an intellectual disability regardless of their skills, every week in communities right across Australia. While some Special Olympics athletes strive to win medals, others enjoy the chance to get active, have fun, make friends and be part of a family. Whatever their motivation, we cater for them by providing meaningful sports programs delivered within a supportive environment where people with an intellectual disability are accepted and can feel proud. People with an intellectual disability are often ridiculed, misunderstood, isolated or simply ignored. Yet, with the understanding and support of Special Olympics they discover the skills that allow them to improve their health, develop self-confidence and bring joy to themselves, their families and their community. Sporting Wheelies & Disabled Association http://www.sportingwheelies.org.au Queensland’s peak body for sport, recreation and fitness for people with a physical disability or vision impairment. Surf Life Saving http://sls.com.au/who-we-are/community-programs/inclusion/sportconnect Offers a range of activities regardless of ability or disability. SLS is part of the Sports Connect program through the Australian Sports Commission, aiming to enhance the opportunities for people with disabilities to access sport. Swimming NSW http://nsw.swimming.org.au Offers Multi Class swimming, which is a form of competition designed specifically for swimmers with disability. These events are normal swimming events with some minor modifications to the rules and regulations. Tennis Australia: http://www.tennis.com.au Provides a tennis program for people with disabilities Ten Pin Bowling http://www.tenpin.org.au Works closely with local centres and state associations to provide inclusive environments in all registered bowling centres. The sport is easily adaptable & can be done by using various adapted equipment & techniques. Provides information on inclusion & adapting the sport. Wheelchair Sports NSW http://wsnsw.org.au Provides a range of sporting programs, wheelchairs, facilities, financial assistance and support across a variety of sports. Programs are specifically designed to cater for people with disabilities & are delivered throughout regional and metropolitan NSW. Wheelchair Sports Group (Coffs Harbour) http://cco.net.au/suppclub/wheelchair-sports-group/ Offers inclusive games of balloon soccer, wheelchair basketball, wheelchair hockey or bocci. A range of activities to suit individual interests & abilities. Fully accessible venue (Sportz Central). Wheelchairs provided.