Major Minerals
advertisement

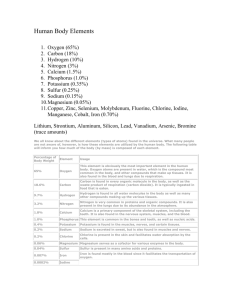
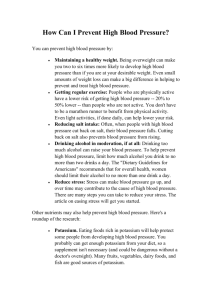
Major Minerals Chapter 11 Major Minerals • A major mineral is required in the diet and present in the body in large amounts compared with the trace minerals. • Minerals are inorganic elemental atoms or ions. • Minerals are not changed during digestion or when the body uses them. Major Minerals • Minerals are not destroyed by heat, light, or alkalinity. • Some minerals assist enzymes. • Some minerals have structural roles. Minerals In the Human Body Minerals in Foods • Foods from both plants and animals are sources of minerals. • Animal tissues contain minerals in the proportions that animals need. Minerals in Foods • The mineral content of plants can vary dramatically depending upon the minerals in the soil where the plant is found. • The maturity of the vegetable, fruit, or grain can affect the mineral content. Mineral Bioavailability • The GI tract absorbs a much smaller proportion of minerals than vitamins. • Once absorbed, excess minerals are difficult for the body to flush out. • The body adjusts mineral absorption in relation to needs. Mineral Bioavailability • Some minerals compete for absorption sites. Megadosing with one mineral can impede absorption of another. • High-fiber diets reduce absorption of iron, calcium, zinc, and magnesium. • Phytate (a component of whole grains) binds minerals and carries them out of the intestine unabsorbed. • Oxalate (found in spinach and rhubarb) binds calcium, reducing its absorption. Mineral Bioavailability Sodium • Sodium (Na) is an essential nutrient. • Sodium is a component of sodium chloride (table salt). • Sodium in the diet is essential for normal body function, but we shouldn’t eat too much salt. • Major extracellular cation. Sodium Functions • Fluid balance. Maintains proper body water distribution and blood pressure. • Nerve transmission and muscle function. • Control’s the body’s acidity. Sodium Food Sources and Recommended Intake • • • • Limit to 2,300 milligrams / day (DV) Processed foods contribute the most sodium. Table salt contributes some. Sauces, pickled foods, salty meats, cheese, salted snack foods, bouillon cubes, canned and instant foods, and seasonings based on salt can all be high sources. • The GI tract absorbs nearly all dietary sodium. • The kidneys excrete excess. Sources of Dietary Sodium Hyponatremia • Hyponatremia – abnormally low sodium concentrations in the blood due to excessive excretion of sodium (by the kidenys), prolonged vomiting, or diarrhea. • Replacement of water without sodium. Hyponatremia • Symptoms of hyponatremia resemble dehydration. • Treatment involves replacement of fluids and minerals through liquids and foods or intravenous solutions if necessary. Hyponatremia • Severe hyponatremia causes extracellular fluid to move into cells, causing them to swell. • Brain cells swell – headache, confusion, seizures, coma. • Cancer, kidney disease, and heart disease can cause hyponatremia. Hypernatremia • Hypernatremia – abnormally high sodium concentrations in the blood due to increased kidney retention of sodium or rapid ingestion of large amounts of salt. • Hypervolemia – an abnormal increase in the circulating blood volume. Hypernatremia • Hypervolemia leads to edema (swelling) and a rise in blood pressure. • A healthy person with normal kidneys and ample water intake rapidly excretes excess sodium. Hypernatremia • Hypernatremia is seen in patients with congestive heart failure and kidney disease. • Eating too much sodium over a long period of time can contribute to hypertension (high blood pressure) in some people. • Excess dietary sodium can contribute to osteoporosis by increasing calcium loss in the urine. Exercise and Sodium Sensitivity • A recent study sought to examine if aerobic exercise training in older people with hypertension changes sodium sensitivity with individuals switching from sodium sensitive to sodium resistant. • The study was validated and shows that that aerobic training in older hypertensive people can alter blood pressure sensitivity. ADA Dietary Guidelines for Americans • Consume less than 2,300 mg (approximately 1 teaspoon of salt) of sodium per day. • Choose and prepare foods with little salt. At the same time, consume potassium-rich foods, such as fruits and vegetables. • Key recommendations for Specific Population Groups: Individuals with hypertension, blacks, and middle-aged and older adults. Aim to consume no more than 1,500 mg of sodium per day, and meet the potassium recommendation (4,700 mg/day) with food. Potassium • Major intracellular cation. • If people with hypertension eat a diet rich in potassium containing foods (fruits and vegetables), their blood pressure often improves. Potassium Functions • Muscle contractions • Transmission of nerve impulses • Helps regulate blood pressure Potassium Food Sources and Recommended Intake • Fresh vegetables and fruits. – Especially potatoes, spinach, melons, and bananas. • Fresh meat, milk, coffee, and tea also contain some potassium. Food Sources of Potassium Hypokalemia • Hypokalemia – low levels of blood potassium. • Low intake can disrupt acid-base balance, contribute to bone loss and kidney stones. • Severe deficiency results from potassium depletion (excessive losses). – Prolonged vomiting, chronic diarrhea, laxative abuse, use of diuretics. • Risk factor for hypertension. Hypokalemia • People with poor diets, such as alcoholics and individuals who suffer from anorexia nervosa or bulimia nervosa, are at highest risk of potassium deficiency. • Athletes doing physical labor in high temperatures have high water losses, so they also risk potassium deficiency. Hypokalemia Symptoms • • • • Muscle weakness Loss of appetite Confusion Severe or rapid potassium depletion can disrupt heart rhythms Hyperkalemia • Hyperkalemia – abnormally high blood potassium. • Malfunctioning kidneys or an excess of intravenous potassium can cause hyperkalemia. • Hyperkalemia can slow and eventually stop the heart. Banana Facts • You may know that bananas are high in potassium, but did you also know that they have an unusually high-carbohydrate content? • Before ripening, a banana is almost entirely starch. After ripening, certain varieties are almost entirely sugar—as much as 20 percent by weight. Chloride • Chloride (Cl-) – anion in table salt. • Chlorine (Cl2) – poisonous gas – highly reactive, used to treat water to kill bacteria and other pathogens. • Chloride is a major extracellular anion. Chloride Functions • Fluid balance. • Combines with H+ to form HCl (hydrochloric acid in the stomach). • White blood cells use chloride to kill invading bacteria. • Assists in the transmission of nerve impulses. Chloride Food Source • Most of our chloride comes from salt. • The kidneys secrete excess chloride and some is lost in sweat. • The only known cause of high blood chloride is severe dehydration. Hypochloremia • Vomiting removes hydrochloric acid from the stomach. • Frequent vomiting (bulimia nervosa) can cause a chloride deficiency. • Frequent vomiting with inadequate fluid and mineral consumption can lead to dehydration and metabolic alkalosis (high blood pH). Hypochloremia • Metabolic alkalosis – abnormal pH of body fluids usually caused by significant loss of acid from the body or increased levels of bicarbonate. – Causes abnormal heart rhythm, substantial drop in blood flow to the brain, decreased oxygen delivery to the tissues, abnormal metabolic activity. – 5 percent rise in pH can be fatal. Calcium • About 1.5 to 2% of total body weight. • Essential for healthy bones and teeth. Calcium Functions • Bones and tooth structure (99%) of calcium. • Remaining 1% in blood and soft tissues. – Muscle contraction. – Nerve impulse transmission. – Blood clotting. – Cell metabolism. Calcium Functions Bone Structure • Bone is made up of cells and an extracellular matrix. • Osteoblasts and osteoclasts continually remodel our bones. Bone Structure • Osteoblasts secrete the collagen protein matrix that forms the framework. • Minerals in the form of hydroxyapatite (calcium and phosphorus) surround the collagen fibers. • We achieve peak bone mass at around 30 years of age. Calcium Food Sources • Dairy products. • Green leafy vegetables such as spinach have high levels of calcium, but it is mostly bound to oxalate and therefore cannot be absorbed. • Chinese cabbage, kale, and turnip greens have significant amounts of bioavailable calcium. • Some food products are fortified with calcium. Calcium Recommended Intake • Adequate Intake (AI) for adults 19 to 50 – 1,000 milligrams per day. • AI for adults aged 51 and older – 1,200 milligrams per day. • AI for adolescents 9 to 18 – 1,300 milligrams per day. Regulation of Blood Calcium • Circulating blood calcium performs many essential functions; therefore, the body will demineralize bone tissue to prevent even minor changes in blood calcium. • Three hormones regulate blood calcium: – Calcitriol (active form of vitamin D) – Parathyroid hormone – Calcitonin Regulation of Blood Calcium • These hormones control intestinal absorption of calcium, bone calcium release, and calcium excretion by the kidneys. • Inadequate calcium intake, high sodium intake, excess caffeine, and other diuretics can effect calcium balance by altering the excretion of calcium in the urine. Vitamin D (calcitriol – active form) • Increases absorption of calcium into the intestine. • Increases the production of calcium binding proteins in the small intestine. Parathyroid Hormone • Parathyroid Hormone (PTH) is secreted when plasma calcium levels fall too low. • PTH activates osteoclasts, which break down bone and release calcium and phosphorus into the blood. • Increases kidney reabsorption of calcium. • Increases phosphorus excretion. • Stimulates calcitriol production. Calcitonin • The thyroid gland secretes calcitonin when plasma calcium is too high. • Acts in opposition to PTH. • Weak effects on blood calcium. • Inhibits formation and activity of osteoclasts. • High calcitonin concentrations decreases PTH production and thus decreases calitriol production. Calcium Absorption • • • • • Between 25 to 75 percent of dietary calcium. High during pregnancy and infancy. Low during old age. Requires adequate levels of vitamin D. Inversely related to calcium intake. Calcium Absorption • Phytates (in nuts, seeds, grains) decrease absorption. • Oxalates decrease absorption. • High levels of phosphorus and magnesium decrease absorption. • Wheat bran decreases absorption (other dietary fibers do not seem to decrease absorption). • Low estrogen levels after menopause decrease absorption. • Calcium from supplements taken between meals and at lower doses of 500 milligrams or less assists in absorption. Hypocalcemia • Hypocalcemia – deficiency of calcium in the blood. • Rare because the body uses bone calcium to maintain blood levels. • Caused by kidney failure, parathyroid disorders, and vitamin D deficiency. Hypocalcemia • Can cause muscle spasms, facial grimacing, and convulsions. • Chronic dietary deficiency causes osteoporosis. • Increased risk of hypertension, colon cancer, and preeclampsia. Hypercalcemia • Major Causes – Cancer – Overproduction of PTH by the parathyroid gland Hypercalcemia • Clinical Signs and Symptoms – Fatigue – Confusion – Loss of appetite – Constipation – Calcium may be deposited in the soft tissue where it can impair organ function. Excess Calcium Supplementation • Excess calcium supplementation usually does not result in hypercalcemia, but may cause mineral imbalances by interfering with the absorption of other minerals, such as iron, magnesium, and zinc. • Calcium supplements that contain citrate and ascorbic acid enhance iron absorption, but other forms cut iron absorption in half. Phosphorus • Widespread in the food supply. • Phosphorus is the most abundant intracellular anion. Phosphorus Functions • Phosphorus plays an important role in bone as part of the mineral complex hydroxyapatite. • Phosphorus helps activate and deactivate enzymes in a process known as phosphorylation. • Essential component of ATP. • Component of DNA, RNA, and phospholipids in cell membranes and lipoproteins. Phosphorus Food Sources and Recommended Intake • Phosphorus is abundant in the food supply. • Foods rich in protein (milk, meat, eggs) are also rich in phosphorus. • Food additives in processed meats and sodas contain phosphorus. • RDA for adults is 700 milligrams per day. Adolescents need about 1,250 milligrams per day. Hypophosphatemia • Phosphorus is so abundant in foods that only near-total starvation will cause a dietary deficiency. Hypophosphatemia • Underlying disorders affect absorption or excretion and cause hypophosphatemia. – Hyperparathyroidism (often due to a tumor) – Vitamin D deficiency – Overuse of aluminum, magnesium, or calcium containing antacids that bind phosphate. Hypophosphatemia • Clinical Signs and Symptoms – Anorexia – Dizziness – Bone pain – Muscle weakness – Waddling gait Hypophosphatemia • Chronic – Affects the musculoskeletal system causing muscle weakness and damage including respiratory problems due to poor diaphragm function. • Long-standing – Can cause rickets and osteomalacia Hyperphosphatemia • Causes – Kidney disease – Underactive parathyroid gland – Too many vitamin D supplements – Overuse of phosphorus containing laxatives – Excessive dietary intake (i.e. too much soda) Hyperphosphatemia • Clinical signs and symptoms – Excessive phosphorus can bind calcium – Low calcium can cause nerve fibers to discharge repeatedly without provocation. This can lead to muscle spasms and convulsions. – Excess phosphorus and not enough calcium can lead to increased bone loss. – Increased phosphorus intake may lead to osteoporosis later in life. Magnesium • Magnesium (Mg) • 50 – 60% is in bone, remainder distributed between muscle and other soft tissues. • Most resides in cells. Only 1% is extracellular. Magnesium Functions • Participates in more than 300 types of enzyme-mediated functions. • Assists in DNA synthesis. • Assists in protein synthesis. • Assists in energy production in the ETS and glycolysis. • Participates in muscle contraction. • Participates in blood clotting. Magnesium Recommended Intake • RDA for adults 19 – 30 years 400 mgs / day for men and 310 mgs / day for women. • Ages 31-70 -- 420mg / day men 320 mg / day women. Magnesium Food Sources • Dietary intake comes primarily from plants. • Whole grains and vegetables such as spinach and potatoes are goods sources. • Legumes, tofu, and some seafood. • Sesame seeds, cashews, almonds. • Processed grains lose up to 80 % of the magnesium and enrichment does not replace Magnesium Food Sources • “Hard” water can contain some magnesium. • High-fiber diets often have a negative effect on mineral absorption. • High calcium intake from supplements can interfere with magnesium absorption. Hypomagnesemia Causes • • • • • Kidney disease Associated with alcoholism Diuretic drugs Prolonged diarrhea Chronically poor diets Mineral Deficiencies • Deficiency in any of the three major intracellular minerals (magnesium, potassium, and phosphorus) usually is associated with deficiencies of the other two. Hypomagnesemia Clinical Signs and Symptoms • Healthy people whose diets are deficient in magnesium usually have no signs or symptoms for a few weeks because of the large supply of magnesium stored in the bone. • Short term deficiency: – Loss of appetite, nausea, and weakness. • Long-term deficiency: – Muscle cramps, irritability, and confusion. Hypomagnesemia Clinical Signs and Symptoms • Extreme: – Death due to heart rhythm problems. Hypermagnesemia • Causes – Uncommon in the absence of Kidney disease – Use of magnesium containing antacids or laxatives • Clinical Signs and Symptoms – Nausea – General weakness Hypermagnesemia • Physicians sometimes prescribe high doses during pregnancy to stop premature labor – Frequent monitoring is required to avoid toxicity that can lead to respiratory paralysis Sulfur • Sulfur is not used alone as a nutrient. • Sulfur is present in certain organic compounds (vitamins biotin and thiamine and amino acids methionine and cysteine) • Disulfide bridges help proteins form their tertiary and quartenary structures. • Adequate protein intake ensures enough sulfur. Deficiency is unknown in humans. Hypertension • Hypertension – high blood pressure. • Major risk factor for heart disease, kidney disease, and stroke. • Genetic predisposition and high sodium diets. • Excess weight tends to raise blood pressure. • Exercise and weight loss tend to lower BP. Hypertension • Reducing alcohol tends to decrease BP. • Diets rich in calcium, magnesium, and potassium reduce blood pressure. Osteoporosis • Osteoporosis means “porous bone”. • In osteoporosis, bone mass or density declines and bone quality deteriorates. Osteoporosis • The bones become fragile and vulnerable to fractures. • Normal development and mineralization of bones requires calcium, phosphorus, flouride, magnesium, vitamin D, vitamin A, vitamin K, and protein.