How to Prescribe Safely

Prescribing Safely
Kevin Gibbs
Pharmacy Manager: Clinical Services
University Hospitals Bristol NHS Foundation Trust
Aims of talk….
Discuss the pitfalls of drug history taking
Introduce medicines reconciliation
Help you to reduce risk from prescribing medicines
Identify sources of information which will help you prescribe safely
Revision from 3 rd year talk!
Give you pointers to ask on your placements
Why me?
You will do this every day
You will be responsible for your prescribing
You will make prescribing errors
You will be expected to prescribe to NPSA competencies (Eg Anticoagulant & IVs)
You need to be aware of potential pitfalls
You need to think about prescribing safely
You need to know when to ask for help
What is a medication error ?
‘ a medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of health professional, patient or consumer’
Incidence of errors
The precise incidence of medication errors in the NHS is unknown
~10-20% of all ADRs are due to errors
In USA 1.8% of hospital admissions have a harmful error leading to 7000 deaths per year
In Australia – 1% of all admissions suffer an ADR due to medication error
Common error types?
Wrong patient
Contra-indicted medicine
Wrong drug / ingredient
Wrong dose / freqency
Wrong formulation
Wrong route of administration
Poor handwriting on
Rx
Incorrect IV administration calculations or pump rates
Poor record keeping
Paediatric doses
Poor administration techniques
Most common types of medication error reported
Commonest causes of medication errors
Lack of knowledge of the drug – 29%
Lack of knowledge about the patient – 18%
“rule” violations – 10%
“Slip” or memory loss – 9%
JAMA 1995;274:35-43
Top Therapeutic
Groups Reported
Prescribing responsibilities
Drug
Dose
Route
Frequency
For parenteral therapy
Diluent and infusion volume
Access line for adminsitration
Rate of administration
Duration of treatment
Allergies and sensitivities
• Provide a prescription that is
LEGIBLE (!!!!!)
Legal
Signed
Giving ALL information to allow safe administration
Controlled drugs
In your handwriting:
1. Name and address of patient
2. Drug and dose
3. Form and strength of the drug
• Modified release
4.
• Strength if liquids/injections
Total quantity (or no. of dosage units) in WORDS and figures)
The requirements for a hospital take-home prescription are the same
Drug history taking
2.
3.
4.
1.
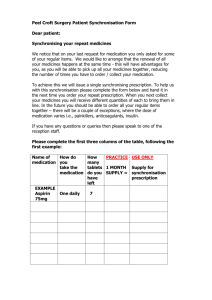
What information should be gathered during a drug history?
What is the aim of the drug history?
Where do you find the information?
What is “Medicines Reconciliation”?
Drug Histories: What information?
Current medication
Dose
Form
Strength
Frequency
Indication
Past medication and treatment failures
Over the counter medication
“Recreational” drugs
Adverse reactions
Allergies and sensitivities - with clinical detail
Estimate of patient adherence / concordance with their medicines
DHx: Information Sources
GP admission letter
GP records – From surgery / fax
Patients own tablets
“Dosetts” = Multi-compartment compliance aids
Written lists – Patient / carer
Nursing home form
Pharmacist patient records
Recent discharge letters
GP admission letter
Do not always contain a drug history
Can only contain those deemed relevant to admission
Out-of-hours
No information for out-of-hours GP services to call on; so incomplete or reliant on patient’s memory / own medication
GP records
Should be definitive; but:
May be inaccurate / incomplete if:
Recent discharge not reached GP and acted upon
Recent discharge had changed medicines with no explanation
Some drugs are secondary-care only or issued in specialist units eg post-transplantation / specialist clinics (CF, psychiatric etc)
These may not be on the GP record
The doses may be altered by the originating unit not the GP, so GP records may not be accurate
GP records - 2
Private prescriptions may not be recorded on GP computer
Watch the date last issued
Has this been stopped?
Is the patient no longer taking the medicine
Adverse reaction?
Lack of effect?
Will have allergies and sensitvities
Patient’s own medicines
Are these for the correct patient?
Easy to pick up a relative’s medicines by mistake
Easy to miss if the same surname
Are they still taking these?
Stopped without GP being aware
Stopped with GP agreement but still on GP list
Stopped a while ago but kept “just in case”
Contents of medicine cupboard emptied!
Compliance aid boxes have lists inside
Previous drug chart or discharge letter
How current are these?
More recent changes?
Check with the patient
Incidences of errors with typist-generated letters
Co-careldopa 3.125mg tds – Prescribed on next admission
Was 31.25 tds
Electronic discharge summaries
Errors from picking incorrect drop-down list
Nursing Home list
MARs sheet
Medication Administration Record
Similar to a hospital drug chart
Should be an accurate list
Community pharmacist records
If one pharmacy is used regularly this can be a additional source of information
Open on saturdays
Will include all prescriptions dispensed fo that patient including
But may also miss hospital-only medicines
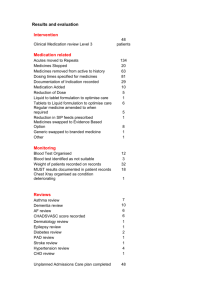
Top 10 drug groups most commonly associated with preventable drug-related admissions
Drug group
Antiplatelets
Diuretics
NSAIDs
Opioids
Beta-blockers
Drugs affecting renin
–angiotensin system
Drugs used in diabetes
Positive inotropes
Corticosteroids
Antidepressants
All preventable drugrelated admissions
(%)
16.0
15.9
11.0
8.5
4.6
4.4
3.5
3.2
3.1
3.0
ADRs and over treatment
(%)
17.3
16.0
12.0
8.9
4.4
4.6
3.2
3.2
3.2
3.2
Patient adherence problems (%)
4.1
9.2
3.1
2.0
2.0
2.0
20.4
4.1
4.1
4.1
0
0
2.2
2.2
Under treatment
(%)
0
0
8.9
2.2
11.1
0
Howard et al Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin
Pharmacol 2006;63(2):136-147.
Other common pitfalls
Prescribed & labelled ‘As directed’
Own tablets not brought in
Several possible strengths eg inhalers
Trade names – beware duplicates
Patient can’t remember
“Dosett” boxes X tablet identification
Asking about “your tablets” – Patients will then miss off inhalers, creams etc!
Take extra care if:
Impaired renal function
Hepatic dysfunction
Children
The elderly
Drug is unknown to you
Very new drug
Medicines Reconciliation: Definition
Definition
“Collecting an accurate list of the patient's home medicines, using that list to write prescriptions; and documenting changes or discontinuation of medicines and doses”
• National Guidance
• National Institute for Health and Clinical
Excellence: Patient Safety Guidance 1.
Technical patient safety solutions for medicines reconciliation on admission of adults to hospital.
< http://www.nice.org.uk/guidance/index.jsp?action=byID&o=11897 >
Medicines Reconciliation: Process
1.
2.
3.
Verification:
Collection of the medication history
Obtaining a complete and accurate list of each patient's current medications (medication history) including name, dosage, frequency and route
Clarification :
Ensuring that the medications and doses are appropriate
Comparing the in-patient prescription or TTA to the medication history
Reconciliation :
Documentation of changes in the prescriptions
Resolving any discrepancies that may exist between the medication history list and prescribed medicines before an adverse drug event
(ADE) can occur
Note: ADEs can result from omitted drugs or doses
This is done at admission, on transfer between levels of care, on discharge
If we don’t reconcile medication?
Systematic review showed 30-70% for unintentional variances between the medication patients are taking and their subsequent in-patient prescriptions 1
Examples
Omeprazole started in ITU for prevention of stress ulceration. No
GI Hx.
Carried on for 3 years
Admitted for surgery. PMH: RA, HTN
GP history not used
Not given regular meds for 6 days
Prednisolone 5mg, Methotrerxate, Alendronic acid, ramipril,
Bendroflumethiazide, Alendronic acid, Folic Acid
Painful joints, stiffness, BP
1: Campbell etal. A systematic review of the effectiveness of interventions aimed at preventing medication error (medicines reconciliation) at hospital admission. University of Sheffield School of Health and Related
Research. September 2007
If we don’t give the GP full details?
How will she know what we have done?
What we have stopped and why
What we have started and why
What they should look out for or monitor, Tx goals
Their records will not be up-to-date
Patients are confused
Different lists from hospital and the GP
Medication is stopped by GP as no idea why started
There will be errors on the next admission
Minimum information to be supplied at discharge
Complete and accurate patient details (full name, date of birth, weight if under 16 years, NHS number, consultant, ward discharged from, date of admission, date of discharge)
The diagnosis of the presenting condition plus co-morbidities
Procedures carried out
A list of all the medicines prescribed for the patient on discharge
(and not just those dispensed at the time of discharge which are in addition to the regular medication)
Dose, frequency, formulation and route of all the medicines listed
Medicines stopped and started, with reasons
Lengths of courses where appropriate (e.g. antibiotics, clopidogrel)
Details of variable dosage regimens (e.g. oral corticosteroids, warfarin etc)
Known allergies, hypersensitivities and previous drug interactions
Any additional patient information provided such as corticosteroid record cards, anticoagulant books etc.
Further inflromation available at url:
< http://npci.org.uk/medicines_management/safety/reconcil/process_tools/pt_data_r econciliation.php
>
Safer Prescribing
Know your patients
Know your medicines
Use a limited number if possible to aid familarisation –
Prescribing Formularies
Use your resources
Peers
Pharmacists
Specialists (medical & non-medical)
Guidelines and decision support help
National help
National Patient safety Agency – Alerts and reports
MHRA – Monthly newsletter for prescribing and adverse reactions
Sign-up for this on website
Alert 20:Promoting Safer Practice
With Injectable Medicines
NPSA receives 800 incident reports a month concerning injectable medicines.
24% of all medication incident reports.
58% of incident reports leading to death and severe harm.
Decision-making with pharmacological therapy:
ENCoRE
E xplore
identify patient nature of symptoms other medicines or treatment allergies and ADRs adherence to treatment exclude serious disease
N o medication option
unnecessary contra-indicated
C are over
older people children pregnancy/lactation
R efer
potentially serious problems persistent symptoms
E xplain
suggested course of action
Pharmacy help
View charts daily
Check doses, calculations etc
Check interactions
Check appropriateness
Provide advice and information
Help with prudent antibiotic use
Medication reviews for patients
On admissions units
Take medication histories
Help with reconciliation
Medicines Information Dept.
All hospitals have access to one - phone/bleep
Any medicines-related enquiry eg
Treatment options
Drugs in pregnancy
Evidence collection and collation
There to help you prescribe safely
Prescribing guidelines and resources
Developed to standardise treatment
Especially: If evidence is conflicting / high risk / high cost
Evidence based use of medicines
Find out what is available in your Trust
Usually intranet-based
BNF / Medusa intravenous drugs guide
Policies
Medicines codes or policies
MUST read and follow
Intranet-based BNF – Localised with Formulary/Local text
Intranet IV administration Guide “Medusa”
Management of Acute Hyperkalaemia in Adults
• tingling clinical features of acute hyperkalaemia hyperkalaemia is defined as a serum potassium greater than 5.2 mmol/L other signs and symptoms ( 1 ) usually asymptomatic but can include;
• paraesthesia • muscle weakness • flaccid paralysis
ECG signs if present treat urgently
• tall, peaked T-waves, followed by flattening of P-wave, prolongation of PR interval, QRS widening, and development of S-wave,
• arrhythmias (bradycardia, VT, VF)
• deterioration to asystole at a serum potassium around 7mmol/L or more
potential precipitant causes i
8
G uide
P oint
QUIT
START BACK INFO PRINTING OPTIONS
PAGE ALL
Page 46 of 11
Prescribing Quiz
Teams of 4/5 people
‘
If need additional information write need info on . . .’
Question 1
A frail 80 year old lady is admitted with falls, a chest infection and feeling sick.
PMH AF and Hypertension
DHx Bendroflumethazide 5mg daily
Atenolol 50mg daily
Ramipril 1.25mg daily
Aspirin 75mg daily
Warfarin 3mg daily
Digoxin 250 micrograms daily
O/A Benzylpenicillin IV 2.4g qds and
Ciprofloxacin po 400mg bd
List 5 potential problems or issues with this prescription….
Question 2
Drug chart =
Benzylpenicillin 2.4G IV qds
Ciprofloxacin 750mg bd
After 2 days therapy the patient can be discharged – write the take home prescription
(TTO – T o T ake H ome)
(TTA – T o T ake A way)
Question 3
A patient is admitted on-call via GP cover service. The admissions letter states the medicines as:
ISMN 60mg / day
Nifedipine 30mg /day
Atorvastatin 30mg / day
Fill in the ‘in-patient’ drug chart for this patient
Question 4
2001 NHS goal – By how much did the number of serious errors in the use of prescribed medicines need to reduced by 2005?
Question 5
Give the generic names of the following
Zocor
Tegretol
Istin
Losec
Question 6
A patient is going home and needs the following:
MST 40mg bd for 14 days
Please write the prescription (excluding name and address)
Question 7
A patient needs Vancomycin 500mg bd IV
Write up in patient drug chart
Question 8
Patient is due to go home and has the following on in patient Rx:
Amiodarone 200mg tds (started 4 days ago)
Simvastatin 10mg on
Furosemide 40mg bd (for post-op peripheral oedema)
Zopiclone 7.5mg on (started in hospital)
Write patients TTO for 1 mth
Answer: Question 1
Bendroflumethazide 5mg daily Dose for HTN is 2.5mg
Atenolol 50mg daily ? cause of falls
Ramipril 1.25mg daily
Aspirin 75mg daily
Seems low, has this been dose-titrated?
Aspirin and warfarin interaction
Warfarin 3mg daily Warfarin and antibiotic interactions
Digoxin 250 micrograms daily Dose ? high as elderly – check levels
Benzylpenicillin IV 2.4G qds
Ciprofloxacin po 400mg bd = IV dose, oral dose is 750mg bd
1 mark per green answer
Answer: Question 2
Change IV to oral
Amoxycillin 500mg tds for 5 days
Ciprofloxacin 750mg bd for 5 days
-1 if unsigned
1 marks each
Answer: Question 3
Isosorbide mononitrate MR 60mg prescribed at 8am
Nifedipine 30mg MR prescribed daily
Atorvastatin 30mg prescribed at night
But an unlikely dose as generally 10mg,
20mg or 40mg (No 30mg tablet) - Check
1 mark each
-1 if no signature included
-1 mark if no routes included
Answer: Question 4
40%
Answer: Question 5
Zocor simvastatin
Tegretol carbamazepine
Istin amlodipine
Losec omeprazole
Answer: Question 6
Morphine (Sulphate) MR (SR) 40mg
BD (for 14 days)
28 (twenty eight) 30mg MR tablets
28 (twenty eight) 10mg MR tablets
(1120mg – one thousand, one hundred and twenty milligrams)
Sign, date and print name
Answer: Question 7
Drug
Vancomycin
Dose
500mg
Route
IV
Start Date
6.1.9
Stop Date
Review
10.1.9
Signature
Squiggle
Pharm
Additional instructions
In 100mls Sodium chloride 0.9% over 60 minutes via peripheral line
8
12
18
24 x x
Answer: Question 8
-
-
Amiodarone 200mg tds for 4 days then bd for 7 days then daily
Simvastatin 10mg on
Frusemide 40mg bd for a set time
Add a note to the GP for review will accept a dose change eg 40mg om
No zopiclone should be required as started in hospital
Summary: Safe prescribing
Clear and unambiguous
Use approved names
No abbreviations eg ISMN
Unless G or mg then write units in full
(micrograms or nanograms)
Avoid decimal points – if needed then make very clear: .5ml X 0.5ml
Avoid a trailing zero: 1.0mg X 1mg
Avoid fractions: 0.5mg X 500 micrograms
Rewrite charts regularly
If amend prescription re-write or sign and date amendment
For frequency use standard abbreviations eg od
/ bd / tds etc
If using a dose by weight calculate the dose needed (NOT 1.5mg/kg)
Take time (e.g. to read patient information)
Use your resources
When in doubt - ASK