Headaches

Headache Management
Fariborz Khorvash
Associate Professor of
Neurology
Why talk about headaches?
Headaches are a common problem
They are sometimes difficult to treat
Can usually be treated well by internists
Headache management is often not optimal
Recent advances can translate into better treatment
Problems in management
Chest pain approach
– Does this patient have a brain tumor?
Episodic care
Underdiagnosis of migraine headache
Ineffective treatments are commonly used
– Acetaminophen, Butalbital/ASA/Caffeine
Inappropriate use of analgesics
Red Flag Signs:
Thunderclap headache
New onset headache
Headache with neurologic signs
Headaches in pregnancy
Headaches in elderly
Progressing headaches
Changes in frequenc or quality of headache
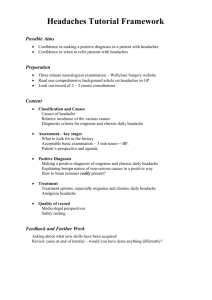
Internal medicine residents
Prepared to manage migraines 48%
Prepared to manage MI, DKA, Asthma 95%
Sinus Headache?
What is a sinus headache?
Many patients with migraines have sinus symptoms.
– Rhinorrhea, congestion, ocular symptoms occur in up to 46% of patients with migraines
Study of 2991 patients with sinus headaches
– Self or physician diagnosed
– 88% met IHI criteria for migraine
Patients reported
–
–
–
Sinus pressure – 84%
Sinus pain – 82%
Nasal congestion – 64%
Diagnosis of sinus headache should be reserved for those patients who meet diagnostic criteria for sinusitis.
Brain Imaging:
New onset headache
Headache with neurologic sign
Headache with seizure
Headache with elevated ICP
Patient request
…….
Headaches
3.
4.
1.
2.
5.
6.
Intracranial pathology
Contiguous structures
Migraine
Cluster
Tension type
Chronic daily/Rebound
Intracranial pathology
Tumor
Subarachnoid hemorrhage
Meningitis
Pseudotumor cerebri
Tumor
–
–
–
–
–
111 consecutive patients with primary or metastatic brain tumor
Classic early morning headache is uncommon
Primary symptom in only - 44%
Worse with bending over - 33%
Similar to TTH in 77%; migraine in 9%
Nausea and vomiting – 40%
Forsyth, Neurology, 1993
Imaging
Relatively solid recommendations
– Not indicated in patients with migraines and normal exam
– Indicated in patients with headache and abnormal exam
Less solid recommendations
Headache worsened by valsalva, exertion, sex
Abrupt onset or awakens patient from sleep
Change in established pattern
New headache in patient >50
Progressively worsening headache
Comorbidities: HIV, cancer, immune suppression
Contiguous structures
Sinuses?
Eyes
Ears
TMJ
Teeth
Temporal artery
Cervical spine
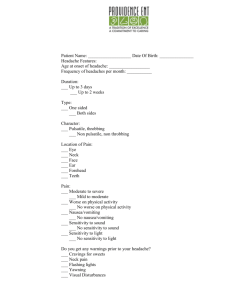
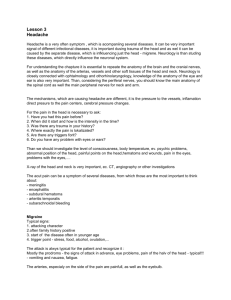
IHS criteria for migraine without aura
Duration 4-72 hours
Two of the following characteristics
–
–
–
–
Unilateral
Moderate – severe intensity
Pulsating
Aggravated by routine physical activity
Headache accompanied by one the following
–
–
Nausea or vomiting
Photophobia or phonophobia
5 attacks
No other explanation
Pathophysiology of migraine
Old theory: vasoconstriction triggers vasodilation
Current concepts
– Originates as a neurologic event in the brain stem
–
–
–
Trigeminal nerve ganglion is stimulated
Vasodilation occurs
Serotonin release contributes
Treatment of migraines
Acute
Preventive
– Life style
– Pharmacologic
Principles of management
Establish a diagnosis
Treat early
Use adequate doses
Tailor treatment to the severity of attack
Use migraine specific therapies
Use preventive strategies
Form a therapeutic alliance with the patient
Empower the patient
Avoid narcotics
Acute treatment
Mild - oral
–
–
–
–
–
–
ASA 975 mg
Naproxen 500-1250 mg
Ibuprofen 800-2400 mg
Cataflam
Ergotamine 2 mg + caffeine 200 mg
Brufen/caffeine/codeine
Mild with nausea
– Add metaclopramide 10 mg
Severe
– Tryptans: oral, nasal, wafer, subQ
–
–
–
–
DHE 1mg subQ, IV, nasal spray
Alternatives
Ketorolac 60 mg IM
Adjuncts
Promethazine
Chlorpromazine (phenergan)
Narcotics
Tryptans
Contraindications
– CAD
– CAD likely
Side effects
–
–
Chest and neck pressure
Dizziness
–
–
Warmth, numbness, tingling, tightness, flushing
Nausea and vomiting
Though sumatriptan may not be the most effective of the tryptans, it is available generically and should be the first choice.
Narcotics
Not more effective
Not specific for underlying pathophysiology
Sedating
Positive reinforcement?
Potential for abuse
Public health crisis
Preventive therapies
Amitriptyline 25-150 mg
Propranolol 80-240 mg
Divalproex sodium 500-1500 mg
Sodium valproate 800-1500 mg
Venlafaxine 75-150 mg
Fluoxetine 20-40 mg??????
Dysport
All are 70% effective
Reduce frequency and severity of attacks
Response cannot be predicted
Dose adjustments necessary
Calcium channel blockers less effective
Decision process
Life style changes
Establish and maintain routines
– Sleep
–
–
Meals
Exercise
Dietary triggers
– Caffeine, chocolate, alcohol, aged cheeses, monosodium glutamate
Nonpharmacologic management
Effective
–
–
Relaxation training
Cognitive behavioral therapy
Ineffective
–
–
–
–
–
Acupuncture
Hypnosis
Manipulation
TENS
Hyperbaric oxygen
Aspirin for migraine prevention?
Observations from the Physicians’ Health Study
– 22,071 doctors randomized to 325 mg of ASA or control
Treatment group: 6% experienced migraine after randomization
Control group: 7.4% experienced migraine
Treatment effect: 20%
Buring, JAMA, 1990
Cluster headaches
“A healthy robust man of middle age was suffering from troublesome pain which came on every day at the same hour at the same spot above the orbit of the left eye: after a short time the left eye began to redden, and to overflow with tears; then he felt as if his eye was slowly forced out of its orbit with so much pain, that he nearly went mad. After a few hours all these evils ceased, and nothing in the eye appeared at all changed.”
Textbook 1745
Clinical features
Unilateral – 100%
Restlessness – 93%
Retroorbital – 92%, (temporal – 70%)
Lacrimation – 91%
Conjuctival injections – 77%
Nasal congestion/rhinorrhea – 75%
Ptosis/eyelid swelling – 74%
Phonophobia/phophobia – 50%
Periodicity
Duration: 8 weeks
Bouts per year: 1
Maximum attacks per day: 4
Attack duration: 15-180 min
Nocturnal: 73%
Treatment
Acute
–
–
Subcut tryptans
74% effective within 15 min
Nasal may be effective
Zolmitriptan 10 mg po – 60% response within 30 min
Oxygen
Treatment
Prophylactic – a small trial involving 30 patients
– Verapamil 120 tid
80% of patients responded
– 40% at the end of one week
Attacks per day after one week
–
–
Verapamil - .6
Placebo
– 1.6
Leone, Neurology, 2000
Other effective therapy
–
–
Prednisone
Bridge to verapamil
Tapered over 3 week
Lithium
– Sodium valproate
– Methysergide
Tension-type headaches
Duration 30 min – 7 days
Two of the following characteristics
–
–
–
Pressing or tightening ( not pulsatile)
Mild to moderate intensity (nonprohibitive)
Bilateral
– No aggravations from walking stairs
Both of the following
–
–
No nausea or vomiting
Photophobia and phonophobia absent (or only one present)
10 previous attacks
Management of TT headaches
Acute headaches
– Minor analgesics
Chronic tension type headaches
– Same diagnostic criteria
– Occur 15 days per month
CTTH: An RCT
Amitriptyline vs stress management vs combination
– 409 patients recruited from primary care practices and randomized to one of 4 treatment groups
Amitriptyline – 48
Stress management – 38
Amitriptyline and stress management – 45
Placebo – 38
Holroyd, JAMA, 2001
Results: All three treatment groups effective
– Mean headache index score
–
–
–
Days of at least moderate pain
Analgesic medication use
Headache disability
Amitriptyline produced results more quickly.
Combination treatment (AM+SM) produced greater than 50% reduction in HA severity in 2/3 of patients
Treatment goals for CTTH
Identify and eliminate triggers
Amitriptyline
Symptomatic treatment with NSAID
Avoid overuse
Stress management
Analgesic abuse or rebound headaches
¾ of patients with chronic daily headaches overuse analgesics
Transformed migraines
– Past history of discrete migraines
Analgesics implicated
Butalbital/aspirin/acetomenophen/caffeine
Codeine, propoxyphene, oxycodone, hydrocodone
Aspirin, acetomenophen
NSAID
Nasal decongestants and antihistamines
Ergotamine
Tryptans
Management strategies
Make a diagnosis
Establish and maintain a relationship
Inform the patients
Stop symptomatic treatment
Start prophylaxis – amitriptyline
Steroid taper (ranitidine 300 bid)
Recognize and treat the underlying headache disorder
Guard against overuse
Effectiveness of treatment
Most patients will stop symptomatic treatment
Steroids seem to reduce withdrawal symptoms
60-70% of patients improve
Improvement occurs over 6 months
30% of patients relapse
Conclusion
How do we diagnose migraine headaches?
How should we treat migraines?
What causes migraines?
Who needs a CT scan?
How do we recognize cluster headaches?
How do we diagnose tension type headaches?
Does anything work for chronic daily headaches?