Management of the Pediatric Airway
advertisement

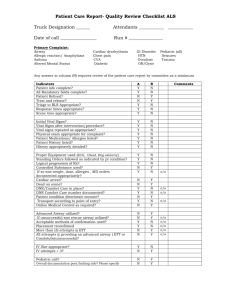
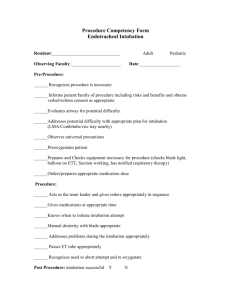
Management of the Pediatric Airway Paul W. Sheeran, MD Dept of Pediatrics Division of Critical Care Dept of Anesthesiology & Pain Management UTSW Medical Center Outline Differences in pulmonary physiology and airway anatomy Mask ventilation and intubation techniques Evaluation of the upper airway Pediatric laryngoscope blades Sizing of ETT and depth of ETT Predictors of difficult intubation Management of the difficult airway Pulmonary Physiology Differences Compliant chest wall Airway collapse at low lung volumes Low FRC (desaturate quickly) High oxygen consumption (6-10 cc O2/kg/min) TV same; minute ventilation increased Airway Anatomy Differences Relatively larger head and tongue More cephalad larynx (C3-4 vs. C5-6) “More anterior larynx” Narrowest part of the airway: cricoid cartilage Long epiglottis (floppy, omega shaped) Easily compressed trachea Adult Glottis Pediatric and Adult airways Mask Ventilation Technique Sizing of Oral Airway Intubation Technique for Neonate Induction Techniques Mask induction (most children): Place monitors 8% sevoflurane in oxygen/nitrous oxide (5L/2L) When asleep: decrease sevoflurane to 4-6%, place PIV, 100% O2, administer NMB, and intubate IV induction (RSI, adolescents, in situ PIV): Place monitors and pre-oxygenate Administer: Pentothal 6 mg/kg or propofol 3 mg/kg and NMB Intubate Upper Airway Evaluation Mouth opening Size of the jaw Thyromental distance Mallampati classification Class I: entire uvula visible Class II: part of uvula hidden by tongue Class III: only soft palate visible Class IV: only hard palate visible Neck range of motion (extension AO joint) Mallampati Classification Cormack and Lehane Grades Miller laryngoscope blades Phillips laryngoscope blades Mac laryngoscope blades Pediatric Laryngoscope Blades Types: Miller Philips Mac Newborn: Miller 0 1 month - 1 year: Miller 1 1–3 years: Philips 1 4-8 years: Mac 2 >8 years: Mac 3, Philips 2, or Miller 2 Difficult Airway due to Dysmorphia Decreased mandibular space (limited mouth opening) Micrognathia, retrognathia, mandibular hypoplasia Pierre- Robin, Treacher Collins Decreased head extension (RA, Klippel-Feil) Increased tongue size or space-occupying lesion (e.g., cystic hygroma) Guides for Proper ETT Sizing ETT size: Newborn: 3.5 mm 4 months-1 year: 4.0 mm Older child: 4 + (age in years/4) Depth of ETT Direct visualization (2nd notch) ETT ID X 3 Loss of breath sounds (carina), pull out 2 cm Cuff palpable in sternal notch Treacher Collins Syndrome Treacher Collins Syndrome Klippel-Feil Syndrome Hunter’s Syndrome Hunter’s Syndrome Other Indicators of Difficult Airway Burns to the face and neck A history of radiation to the head and neck A history of difficult intubation (i.e., read old anesthesia records if available) Other Causes of Difficult Intubation Oral bleeding and swelling (e.g., mucositis, Steven’s Johnson Syndrome, or recent T&A) Copious oral secretions (e.g., RSV, ARDS, pulmonary hemorrhage) Severe cardiac dysfunction (e.g., myocarditis, sepsis) Difficult Airway Management Anticipate problems: Call for help Place PIV pre-op Administer glycopyrolate (10 mcg/kg IV or IM) one hour prior to intubation Keep patient spontaneously breathing (no NMB) Techniques Fiberoptic intubation (FOI) LMA placement alone (no ETT) LMA placement followed by FOI Light wand-assisted oral intubation Acquired Difficult Airway Epiglottitis/supraglottitis Croup Foreign body Trauma Epiglottitis/supraglottitis Acute inflammation of the epiglottis, aryepiglottic folds, arytenoids, and supraglotis School-aged child presents with high fever, drooling, and inspiratory stridor Causes: bacteria or caustic ingestion Do not examine with a tongue blade Take to the OR Mask or IV induction without paralysis Rigid bronchoscopy by ENT Croup Gradual onset of inspiratory stridor and “barky” cough in young children (<3 years) Subglottic narrowing (steeple sign on CXR) Treatment: Cool mist Nebulized racemic epinephrine Intubate if patient is in respiratory failure (smaller ETT than expected is typically needed) Foreign Body Aspiration Young child with either Acute h/o choking Chronic h/o pneumonia or refractory wheezing/cough Stable patients may be X-rayed Unstable patients: intubated and then taken to the OR For esophageal FB: RSI, intubation, and esophagoscopy For laryngeal FB: Mask or IV induction (without NMB) Rigid bronchoscopy by ENT surgeon Upper Airway Trauma Neck trauma may cause laryngeal and/or tracheal injuries Presenting symptoms: SQ air, neck swelling, hypoxia If the patient is in extremis in the E.R. IV ketamine and glycopyrolate Intubate orally Confirm ETT location prior to NMB If the patient is stable, then take to the O.R. Mask or IV induction without paralysis Tracheotomy by ENT Oral intubation is controversial Summary Pediatric patients have a small FRC and increased O2 consumption: pre-oxygenate with CPAP It is imperative to evaluate the airway prior to administering paralytic agents Difficult intubation associated with micrognathia, decreased head extension, and a large tongue Problems with patients with a difficult airway should be expected: “Don’t go down alone”