BASIC HUMAN NEEDS SKIN INTEGRITY & WOUND CARE
advertisement
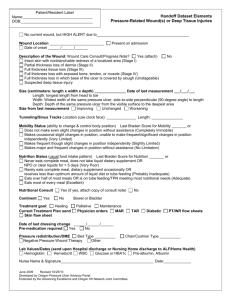
BASIC HUMAN NEEDS ALTERATIONS IN SKIN INTEGRITY PRESSURE ULCERS Donna M Penn RN MSN CNE Skin Integrity Skin/Integumentary system is the body’s largest organ, 1/6th of TBW Protects against disease causing organisms Sensory organ for temp, pain, touch Synthesizes Vitamin D Injury to skin poses a risk to safety and triggers a complex healing process Normal Integument 2 principle layers in relation to wound healing Epidermis Dermis Separated by basement membrane Epidermis Outer layer has several layers within it Stratum Corneum Stratum Lucidem Stratum Granulosum Stratum Spinosum Basal cell layer Dermis Inner layer of skin Provides tensile strength & mechanical support & protection to underlying muscle, bones, and organs Contains mostly connective tissue Also includes blood vessels, nerves, sensory nerve cells, lymphatics, collagen Skin Functions Epidermis-functions to re-surface wounds & restore the barrier against bacteria Dermis-functions to restore structural integritycollagen& physical properties of skin Pressure Ulcers New NPUAP terminology (2007) A pressure ulcer is a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction. A number of contributing factors are also associated with pressure ulcers Pressure Ulcers Tissues receive oxygen and nutrients and eliminates metabolic wastes via the blood Any factor that interferes with this affects cellular metabolism and cell life Pressure affects cellular metabolism by decreasing or stopping tissue circulation resulting in tissue ischemia Causes of Pressure Ulcers Pressure > ischemia > edema > inflammation > small vessel thrombosis > cell death Shear – trauma caused by tissue layers sliding across each other, results in disruption or angulation of blood vessels Pressure Ulcer Contributing Factors Friction Poor Nutrition Incontinence Moisture Co-existing Medical Conditions Pressure Tissue damage occurs when pressure exerted on the capillaries is high enough to close the capillaries Capillary closing pressure is the pressure needed to close the capillary > 32 mmHg After a period of ischemia light toned skin undergoes 2 hyperemic changes Hyperemia Normal Reactive Hyperemia-visible effect of localized vasodilatation (REDNESS) area will blanch with fingertip pressure and redness lasts less than 1 hour Abnormal Reactive Hyperemia-excessive vasodilatation and induration (edema) in response to pressure. Skin appears bright pinkred. Lasts 1 hour to 2 weeks Risk Factors for Pressure Ulcer Development Impaired Sensory Input Impaired Motor Function Altered Level of Consciousness Orthopedic Devices Pathogenesis of Pressure Ulcers Intensity of pressure and capillary closing pressure Duration and sustenance of pressure Tissue Tolerance Pathogenesis of Pressure Ulcers Bony prominences are most at risk (sacrum, heels, elbows, lateral malleoli, greater trochanter, ischial tuberosities Pressure ulcer forms as a result of time/pressure relationship Greater the pressure and duration of pressure, the greater the incidence of ulcer formation Pathogenesis of Pressure Ulcers Skin and subcutaneous tissue can withstand some pressure Tissue will over time become hypoxic and ischemic injury will occur If the pressure is above 32mmHg and remains unrelieved to the point of tissue hypoxia, the vessel will collapse and thrombose Pathogenesis of Pressure Ulcers If circulation is restored before this critical point, circulation to tissue is restored (Reactive Hyperemia) Skin has a greater ability to tolerate ischemia than does muscle, hence true pressure ulcers begin at bone with pressure related to muscle ischemia eventually coming through to epidermis (Shear injury) Sacrum and heels most susceptible Pressure Ulcer Staging Depth of destroyed tissue Does not indicate healing Ulcer covered by necrotic tissue or eschar cannot be staged until debrided NPUAP system used most clinically Other staging systems exist Stage 1 Pressure Ulcer Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have blanching: its color may differ from the surrounding area The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Stage I may be difficult to detect in individuals with darker skin tones Stage I Treatment Off-load pressure Transparent film dressing Hydrocolloid dressing Moisture barrier Stage 2 Pressure Ulcer Partial thickness skin loss involving the epidermis and/or dermis. The ulcer is superficial and presents clinically as an abrasion, blister, or shallow open ulcer Presents as shiny or shallow ulcer (red/pink wound bed) without slough or bruising. This stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation Stage II Treatment Hydrocolloid dressing: dressing of choice in minimally draining stage 2 ulcer Absorptive dressings (Foam) draining wounds Hydrogel: Healing wounds Off-load pressure Stage III Full thickness skin loss involving damage or necrosis to subcutaneous tissue that may extend down to, but not through underlying fascia Ulcer presents as a deep crater with or without undermining or tunneling of adjacent tissue Slough tissue may be present but does not obscure the depth of tissue loss Depth varies by anatomical location Stage III Treatment Requires physician order for Stage III or IV Draining vs. Non-draining Necrotic vs. Granulating Draining wounds-Absorptive dressings Granulating wounds-Hydrogel Necrotic wounds-Require debridement (Chemical. Mechanical, Autolytic, Sharp) Stage IV Full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone , or supporting structures (tendons, joint) Undermining and tunneling are often associated with Stage IV ulcers Slough or eschar may be present in some on some parts of the wound bed Depth of wound varies by anatomical location Exposed bone or tendon is visible or directly palpable Unstagable Wounds Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown, black) in the wound bed The true depth of the wound cannot be determined until slough or eschar is removed, therefore stage cannot be determined. Stable eschars serve as the body’s natural biological cover and should not be removed Deep Tissue Injury Purple or maroon localized area of discolored intact or blood filled blister due to the damage of underlying soft tissue from pressure or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue May be difficult to detect with darker skin tones Evolution may include a thin blister over a dark wound bed Staging by Color Black Yellow Pink/Red Mixture of colors Process of Wound Healing Primary Intention Secondary Intention Healing by Primary Intention Inflammatory (Reaction) Proliferative (Regeneration) Maturation (Re-modeling) Healing by Secondary Intention Healing takes longer Wounds drain more fluids Inflammation phase is prolonged, chronic Wound becomes filled with fragile granulation tissue rather than collagen Wound Contraction takes place More susceptible to infection Complications of Wound Healing Hemorrhage Infection (Nosocomial) Dehiscence Evisceration Fistula Formation Risk Assessment for Pressure Ulcers Identify at risk population Norton Scale Gosnell Scale Braden Scale- most uses clinically, includes 6 subscales (sensory perception, moisture, activity, mobility, nutrition, friction & shear 6-23 score, <18 at risk in hospitalized patients Refer to P&P pg. 1496-1497 for Braden Scale Factors Affecting Pressure Ulcer Formation Shearing force Friction Moisture Tissue Tolerance Factors Nutrition Infection Impaired Peripheral Circulation Age Factors that Impair Wound Healing Age Malnutrition Obesity Impaired oxygenation Smoking Diabetes (blood glucose level) Drugs Radiation Wound Stress Nursing Process Assessment Predictive measures-Risk assessment tools Skin assessment- any areas susceptible to pressure sources, (NG, oxygen tubes, casts, bony prominences) Tactile Assessment-Blanching red areas Assess mobility Assess nutritional status Wound Assessment Location, Size, Stage Wound drainage Wound bed, tissue type Wound edges Periwound skin Presence of undermining, tunneling Wound Assessment Anatomical location Stage-NPUAP staging Staging is for pressure ulcers only, other wounds are classified as partial or full thickness Size- Measure length, width, depth in centimeters Wound Assessment Drainage Amount, color, consistency, odor Scant, moderate, large Serous, serosanguinous, purulent, yellow, brown, green, clear Odor to wound may be indicative of infection Wound Assessment Tissue Type When describing wound bed include % of each tissue type (50% slough, 50% granulation) Necrotic tissue-nonviable Eschar- dry, leathery, black or brown Slough- stringy, cheesy, loose, yellow, tan Granulation- healthy, viable pink to beefy red Epithelialization-occurs along wound edges or as islands inside wound bed, pale pink resurfacing of wound Wound Assessment Periwound Area Erythema-may mean infection Maceration-Whitish, wrinkled appearance Indicates presence of excessive moisture Rash- Macular or papular, may indicate fungal infection Wound Assessment Presence of Undermining/Tunneling Document location and depth Use hands of clock as descriptor Measure with cotton tipped applicator Staging Limitations Difficult to identify stage I in dark skinned patients Unable to stage when obscured by eschar Reverse Staging/Downstaging Nursing Process Diagnosis You tell me!!!!! Nursing Process Planning Preventing pressure ulcers-early identification of those at risk (Braden, Norton, Gosnell scales) Prevention protocols by hospital Positioning Hygiene and skin care (incontinence care) Support surfaces Nutritional support Prevent friction and shear Education Nursing Process Acute Care Implementation Management of Pressure Ulcers Culturing wound Cleansing wound Debridment of wound Moist Wound Healing Dressing selection Nutritional support Off-load pressure Wound Dressing Selection Goal: Promote moist wound healing Transparent dressing Hydrocolloid Hydrogel Calcium alginate Foam dressing Silver/Antimicrobial Collagen dressing Biological dressing (Regranex) Negative pressure wound therapy (VAC) Practice Scenario The nurse is assessing a bedridden client when a large erythemic area is noted on the client’s sacrum. In addition, the center of the injury looks like an abrasion with a shallow center. The nurse would classify this ulcer as: How will the nurse treat this type of pressure ulcer? What risk factors could have contributed to this patient developing a pressure ulcer? Practice Question A nurse is working in a geriatric screening clinic. The nurse would expect that the skin of the normal elderly client will demonstrate which of the following characteristics? A. Dehydration causing skin to swell. B. Moist skin turgor. C. Skin turgor showing a loss of elasticity D. Overhydration causing skin to wrinkle. Practice Question The nurse decides to treat a Stage II pressure ulcer with a hydrocolloid dressing. The nurse recognizes that the dressing will promote which type of wound debridement? A. Sharp B. Autolytic C. Chemical D. Mechanical