Concussion: Evaluation and Management of Sport Injury
advertisement
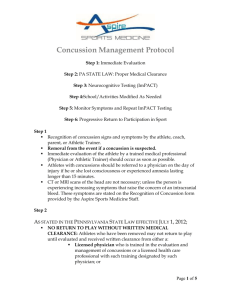
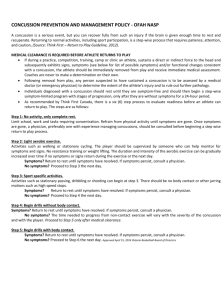
Jeffrey L. Tanji, MD Associate Medical Director, Sports Medicine, UC Davis Health System Melita Moore, MD Head Team Physician, UC Davis Intercollegiate Athletics Mindgame Disclosures I have no relevant financial relationships to any products discussed in this talk I do not intend to talk about an unapproved/investigative use of a commercial product in this presentation Rationale Standards of care for sport concussion have changed dramatically over the last two years New state law mandates certain actions in the management of concussion Sport concussion is under-recognized and underreported Community education and awareness are paramount Objectives Define a sport concussion List the key symptoms and findings of concussion Demonstrate the key aspects of the history and physical in the evaluation of concussion Define the three steps of medical clearance to begin rehab after concussion Objectives List the four steps of progression between medical clearance and true return to play Discuss several controversies in concussion management Mindgame is a multi-health system integrated approach to youth concussion care (Kaiser, Dignity Health, Sutter, UC Davis) in the Sacramento Valley Definition Mild traumatic brain injury (TBI) Metabolic, functional (not structural) damage from direct or indirect trauma Classically, attention, vision, balance, headache, memory are affected but only short term with relatively rapid recovery Useful data 1.5 to 4 million concussions/year in sport 80-90% -no- LOC 80-90% return to full activity in 1 week (NCAA data) We seek to avoid second impact syndrome which is associated with long term issues Younger and female athletes take longer to recover, the younger, the slower to return, discussion that high school athletes may need two weeks minimum Second impact syndrome A second concussion while still symptomatic Generally within the same season Mild trauma can have dramatic effect and long recovery Major brain injury in sport concussion is almost always associated with second impact Sport and concussion Football Ice hockey *Women’s soccer* Youth soccer Field hockey and lacrosse Wrestling Lingering metabolic effects 30 days of vascular spasm and decreased cerebral flow Hyperglycemia K and Ca channels are disrupted Generally a bleed is not found on MRI or CT The “neurometabolic cascade” Hovda DA and Giza CC, Clin Sport Med 2011:30(1):33-48 Neurometabolic cascade Concussion: signs LOC less than 10-20% Headache Visual difficulties Nausea/vomiting Balance issues Memory loss/confusion No return to play that day California AB 25 (2012) for a suspected concussion, there will be no return to play that day Medical clearance by a licensed professional must be given before return to activity California AB 2127 (Cooley law) Jan 1, 2015: 7 day mandatory no return to play and to follow protocols Role of advanced imaging Excludes severe bleed, critical structural damage Does not clear an athlete to return to play Misconception by family and athlete “I was told my concussion was normal and I was cleared to play” When they were told that they could go home and that the imaging study was normal Follow up No need to keep waking a person up hourly Tylenol is ok, no ASA or NSAIDs Worsening status -> ED 1-2 workday follow up through Mindgame Sacramento Rest and cognitive rest Concussion: established treatment Cognitive rest No cell phones, no games, no texting No television, no reading No physical activity www.cdc.gov/concussion Follow up symptoms Symptoms: Headache Visual issues Balance Sleep Emotions (short fuse?) Concentration Follow up physical findings Orientation, EOM and pupillary response Finger -> nose, heel to shin, rapid alternating movements Heel to toe walking Romberg Physical findings No Sx and examination WNL Neurocognitive testing (NCT): Ideally a baseline test has been done If no baseline, compare with age related norms, > 20 percentile Computer based NCT Three steps to clearance No symptoms Normal focused neurological examination Return to baseline or appropriate scores on neurocognitive testing Then work with coach or athletic trainer for the progressions to full competition Rehab progression Run, jog 20 minutes without symptoms Wait one day Sprint, interval speed work without Sx Wait one day Return to the field with no contact Wait one day Return to the field with full contact Variations in progression timing Zurich consensus conference 2013: one day between stages University of Pittsburgh: two days between stages National Basketball Association: one hour between stages Complex cases Persistent symptoms Formal neuropsychological assessment, work with a vestibular physical therapist ? ENG studies (as if for acoustic neuroma) Debate about gentle walking Formal neurologist, neuropsychologist or physiatrist evaluation Vestibular PT Take Home Points No return to play the same day Neurocognitive testing (NCT) is becoming the standard of care No symptoms, normal exam, normal NCT clears to begin the progression Progression: aerobic, sprint, on-field no contact and finally on-field with contact ED take home points The findings of a normal imaging study do not clear an athlete to return to play Must keep follow up outpatient visit for clearance (state law AB25) No symptoms, normal physical exam and a normal neurocognitive test are needed Then an athlete begins a rehab progression before clearance to play Resources McCrory P, Meeuwisse W, Aubry M, et al. Consensus statement on concussion in sport, Br J of Sports Med 2013; 47:250-258. www.cdc.gov/concussion www.sacramentovalleyconcussion.com www.aroundthecapitol.com/bills/AB25 www.aroundthecapitol.com/bills/AB2127 www.sacramentovalleyconcussion.com