Documenting Rehab Services for a Medicare Reviewer
advertisement

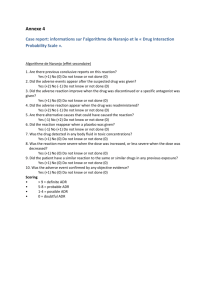
Documenting Rehab Services for a Medicare Reviewer PACAH 2015 Colleen Williams, MS, CCC-SLP, Clinical Specialist Michelle Seeley, COTA, Director of Rehab Jaclyn Warshauer, PT, Sr. Clinical Claims Review Specialist OBJECTIVES • Gain a better understanding of the medical review process • Recognize key pieces of documentation a Medicare reviewer uses to make Rehab coverage decisions • Learn pros and cons of electronic documentation CMS Medicare Claims Review Entities - Medicare Administrative Contractor (MAC) - Recovery Audit Program (RAs-formerly the RAC) - Supplemental Medical Review Contractor (SMRC) - Comprehensive Error Rate Testing Contractors (CERT) - Zone Program Integrity Contractor (ZPIC) Coming in the future: • Unified Program Integrity Contractor 4 Medicare – From ADR to ALJ Additional Development Request (ADR) Phase* **An ADR Request is NOT a “Denial” • • • • You May or May Not receive a Probe Notification Letter You will receive an ADR Request for Medical Records You typically have 30 days to submit You will receive your Initial Determination Decision within 60 days if ADR is from MAC or RA; Indefinite time period for CERT, ZPIC, or OIG. 5 Medicare – From ADR to ALJ Level Summary of Review Process Who performs the Review? When must you request an appeal? When should you get a decision? AIC 1st Level Redetermina tion Document review of initial claim determination MAC Up to 120 days after receipt of initial determination 60 days No • Info for slides 6 – 10 taken from “Medicare Parts A and B Appeals Process” CMS publication. • AIC = Amount in Controversy Threshold 6 Medicare – From ADR to ALJ Level Summary of Review Process Who performs the Review? 2nd Level Reconsideration Document QIC review of redetermination (you should submit any evidence not previously presented at this level) When must you request an appeal? When should you get a decision? AIC Up to 180 days after you receive MRN/RA 60 days No 7 Medicare – From ADR to ALJ Level Summary of Review Process Who performs the Review? When must you request an appeal? When should you get a decision? AIC 3rd Level – ALJ Hearing May be an on-therecord review or an interactive hearing between parties ALJ Up to 60 days May be after you delayed due to receive notice volume of QIC decision or after expiration of the applicable QIC reconsiderati on timeframe if you do not receive a decision Yes 8 Medicare – From ADR to ALJ Level Summary of Review Process Who performs the Review? When must you request an appeal? When should you get a decision? AIC 4th Level – Medicare Appeals Council Review Document review of ALJ’s decision or dismissal (but you may request oral arguments) Appeals Council Up to 60 days after you receive notice of ALJ decision or after expiration of the applicable ALJ hearing timeframe if you do not receive a decision 90 days if appealing ALJ decision or 180 days if ALJ review time expired w/o a decision No 9 Medicare – From ADR to ALJ Level Summary of Review Process Who performs the Review? When must you request an appeal? When should you get a decision? AIC 5th Level – Judicial Review Judicial review U.S. District Court Up to 60 days No statutory after you time limit receive notice of Appeals Council decision or after expiration of the applicable Appeals Council review timeframe if you do not receive a decision Yes 10 2015 Part B Therapy Cap and Therapy Threshold • $1940 - Medicare Part B therapy cap for OT • $1940 - The combined cap for PT and SLP • Exceptions to the therapy cap are allowed for reasonable and necessary therapy services by appending the KX modifier • Per beneficiary, services above the $3,700 threshold for PT and SLP services combined and/or $3,700 threshold for OT services are subject to manual medical review 11 Best Practices - System for tracking when you are approaching $3700, based on “burn rate” and projected therapy - Anticipate which claims will be ADR’d - Pro-active assignment of tasks - Communication that ADR received and results received - Responsibility for assembling ADR packet - Tracking of ADR / Appeals 12 Responding to the Part B Therapy ADR Requests • Have a system to assign accountability for assembling the ADR packet: • • • • Who will print the signed orders (as applicable) Who will make a copy of the signed physician certification Who will print the therapy medical records Who will review the physician and nursing notes to determine which notes to include • Who will organize, assemble, tab the ADR packet • Who will review the packet for legibility and completeness • Who will send the ADR packet to the FI/MAC • Be sure to make a copy first 13 Tracking Part B Therapy ADRs • Assign accountability for Tracking the ADRs and Appeals • Record specific claims ADR’d, services under review • Date sent to FI/MAC • Verify delivery via certified mail, Fed-Ex signatures and/or fax receipts • Date claim adjudicated / response received • Results of medical review • Follow same format for tracking through each level of appeal, as applicable 14 SNF Part A Coverage – Four Required Conditions 1. Requires skilled nursing or rehabilitation services • Ordered by a physician • Condition for which the patient received inpatient services or for a condition that arose while receiving care in a SNF for a condition in which the patient received inpatient hospital services • “In this context, the applicable hospital condition need not have been the principal diagnosis that actually precipitated the beneficiary’s admission to the hospital, but could be any one of the conditions present during the qualifying hospital stay.” 15 Daily Skilled Services 2. Requires Skilled Services Daily DAILY Defined: “A patient whose inpatient stay is based solely on the need for skilled rehabilitation services would meet the “daily basis” requirement when they need and receive those services on at least 5 days a week.” 16 Daily Skilled Services • “The daily basis requirement can be met by furnishing a single type of skilled service every day, or by furnishing various types of skilled services on different days of the week that collectively add up to “daily” skilled services.” • “Arbitrarily staggering the timing of various therapy modalities through the week, merely in order to have some type of therapy session occur each day, would not satisfy the SNF coverage requirement for skilled care to be needed on a “daily basis.” 17 “Daily” Requirement • “It is not sufficient for the scheduling of therapy sessions to be arranged so that some therapy is furnished each day, unless the patient's medical needs indicate that daily therapy is required. For example, if physical therapy is furnished on 3 days each week and occupational therapy is furnished on 2 other days each week, the “daily basis” requirement would be satisfied only if there is a valid medical reason why both cannot be furnished on the same day.” • “The basic issue here is not whether the services are needed, but when they are needed. Unless there is a legitimate medical need for scheduling a therapy session each day, the “daily basis” requirement for SNF coverage would not be met.” 18 Four Required Conditions 3. Can only be provided in a SNF on an inpatient basis • “The services must be ones that, as a practical matter, can only be provided in a SNF on an inpatient basis” • This applies not only at the time of admission, but also through the SNF stay 19 Four Required Conditions 4. The services must be reasonable and necessary for the treatment of a patient’s illness or injury • • • be consistent with the nature and severity of the individual’s illness of injury the particular medical needs and accepted standard’s of medical practice The services must also be reasonable in terms of duration and quantity. 20 Skilled Rehabilitation – All Must be Met • Directly and specifically related to an active written treatment plan...approved by the physician • A level of complexity and sophistication, or the condition of the patient must be of a nature that requires the judgment, knowledge, and skills of a therapist • Will improve materially in a reasonable and generally predictable period of time; or must be necessary for the establishment of a safe and effective maintenance program; or the services must require the skills of a therapist for performance of a safe and effective maintenance program 21 Skilled Rehabilitation • Be reasonable and necessary for the treatment of the patient’s condition • Amount, frequency, and duration of the services must be reasonable • Therapy services are not reasonable and necessary and would not be covered if the expected results are insignificant in relation to the extent and duration of physical therapy services that would be required to achieve those results • Accepted standards of practice to be specific and effective treatment for the patient’s condition 22 Skilled Rehabilitation • When rehabilitation services are the primary services, the key issue is whether the skills of a therapist are needed • The deciding factor is not the patient’s potential for recovery, but whether the services needed require the skills of a therapist or whether they can be provided by non-skilled personnel 23 Medical Review • When a Medical Reviewer looks at Records…they are concerned about: • The Bill Type – tells the reviewer if this is an outpatient hospital clinic, a home health agency, a SNF Part A claim or a SNF part B claim, an outpatient rehab facility claim, and there are more bill types…the bill type is important because it tells the reviewer what coverage guidelines need to be applied in the review • The Edit Number - might tell them if this is a provider specific probe for outpatient PT services, or maybe it’s a widespread probe for say, lower SNF RUGS. The edit number tells the reviewer which service are to be audited • Dates of Service • The patient as described in the record in front of them 24 Medical Review • When a Medical Reviewer looks at Records…they are NOT concerned about: • The Facility Name – It doesn’t matter WHO they are reviewing….they are reviewing a service. • The other thing to keep in mind is that in the Part B therapy world it doesn’t matter to a reviewer what type of facility you are • Medicare calls Part B therapy “outpatient therapy” even if the patient is not an “outpatient” • The outpatient therapy coverage and general billing guidelines are the same whether the patient is receiving services in an outpatient hospital, a PT/OT/SLP private practice, as a resident in a NF or ALF, or as Home Health part B services. The guidelines are all the same. 25 Productivity • Reviewers have productivity expectations too! • How you can help • Document payable services • Quality, not Quantity • Clear, concise, objective, measurable, functional and legible • Paint the complexity of the patient’s condition • Describe the complex nature of the treatment provided • Assessment of the activity and the treatment adjustments made 26 Reviewers love to PAY claims! Simple Two Step Process 27 “I never got a denial so I must be doing everything right!” 28 Documentation… Convincing the Reviewer 29 Coverage Determinations • Medicare coverage determinations are made based on the documentation, and the documentation alone • The reviewer knows nothing else about the patient or the quality of your facility • The documentation is used to determine if the patient’s condition and level of function required the special knowledge and skills of a therapist/nurse • “Make it easy for me to pay this.” • Avoid making the reviewer search to determine if the services are medically necessary • Risks some important piece of information being missed • Risks findings of inconsistencies in the documentation = denials 30 a bit more detail…. 31 It’s all about the Initial Evaluation/Intake! • The initial evaluation sets the stage for all subsequent clinical services • Reviewers will begin to anticipate how much therapy/skilled nursing might be needed for the condition described • Poor or scant evaluation/intake documentation risks that ALL subsequent services will be denied 32 • Descriptive Initial Evaluation – Tell the patient’s STORY • Must have some sentences/phrases • Makes it a “real” patient for the reviewer • Limit the amount of check boxes/drop down boxes for describing the Reason for Referral, Recent History, and any Assessment Summaries • Connect the dots for the reviewer 33 • Complex • Describe the complex nature of the patient’s condition • Where not obvious describe the impact the complexities will have on the plan of treatment Complexity = Amount of therapy/treatment 34 • Logical • Must make the reviewer think, “Oh, I can see why this patient requires skilled services now.” • Logical flow from the reason for referral, to the assessment findings/scores, to the selected treatment interventions, and the subsequent goals 35 Initial Evaluation “Must Haves” 1. Reason for Referral in paragraph form This happened and then this happened and now the patient can’t do this and requires therapy in order to do this. 2. PLOF and CLOF for every area that you will be addressing in therapy 3. Comprehensive Underlying Impairment assessment If you don’t measure it – and re-measure it – you can’t treat it! 36 Ongoing Therapy Services • Must continue to support Medical Necessity and Skilled Services • Medical Necessity (the patient’s condition) • Progress Reports – minimum every 10 treatment visits for Medicare • Consistently include objective measures of every: • Functional Deficit addressed or going to be addressed • Underlying Impairment treated or going to be treated If you don’t measure it – and re-measure it – you can’t treat it! • Documentation needs to include descriptions of any treatment adaptations, changes, adjustments and progressions. This information can be in either daily notes or in progress reports. 37 • The services must be so inherently complex that they can only be safely and effectively performed by a therapist/assistant • Services that can be performed by or taught to nonskilled persons or can be completed as an independent program are NOT skilled therapy • Non-skilled: the patient, personal trainer, CNA, spouse, caregiver, aide, tech, etc 38 The Quick Hit Denial Repetitive Services 39 • Reviewers expect to see documentation of adjustments, progressions and/or modifications to the treatment techniques, activities and interventions 40 Supportive Documentation • Need to have supportive nursing documentation to support the need for therapy. • Also need documentation to support progress made in therapy. • Nursing documentation should be functional in nature and reflect the resident’s performance as it relates to their Rehab program. 41 A few samples of supportive documentation • PT - Ambulation: Address the resident’s ability to ambulate on the unit. Include distance and any assistance required. This could include staff or a device used, such as a walker. (example: Ambulates in hall with the assistance of a CNA. Resident ambulates 25 feet to and from the bathroom with a walker and contact guard of one.) • ST - Swallowing/Chewing: Notes should include mention of the resident’s ability to swallow including drooling, difficulty chewing, pocketing, coughing, choking, gagging. (example: Resident drools when give PO water. Resident coughs occasionally when given PO fluids.) 42 • OT - Bathing: Please note the resident’s ability to bathe or participate in the bathing/showering process. This should include the ability and degree of participation exhibited by the resident as well as any assistance required. (example: Resident needs assistance with tub and shower. Is able to wash face and upper body with set up and minimal cueing.) 43 Achieving Convincing Documentation • • • • Do documentation audits Increase documentation audits in high-risk facilities Increase documentation audits for “outliers” Provide FEEDBACK during audits • Feedback is effective in changing behavior • Validate • Provide feedback for auditors as well to assure they are providing a quality review with feedback 44 Avoid being an “outlier” • Do not to fall into treatment/documentation patterns of: • • • • • ICD-9 Codes CPT Codes RUG levels Frequency Duration • UNIQUE PATIENT UNIQUE/INDIVIDUALIZED PLAN OF CARE 45 • Recognize when you might be an outlier • There are valid reasons to be an outlier • Be diligent in your documentation and your documentation audits • If identified as an outlier and/or on probe review: • BE EXTRA diligent in documentation • All payment decisions are made based on the documentation, and the documentation alone 46 Electronic Documentation 47 Electronic Documentation Cons • The documentation is still only as good as the therapist making the entries • Even with controls for “required” fields and electronic mapping, need to do internal documentation audits • Difficult for the reviewer to obtain a unique picture of the patient (Significant con!) • Feels like there’s just a bunch of dots on the page and nothing is connected • Some documentation programs carry over entries from the previous days • Denial risk 48 Electronic Documentation Pros • LEGIBLE! • You can control the fields that are required • Allows for starter phrases or controlled entries using language suggestive of medical necessity or skilled services • Make use of the narrative entry areas! Show the individuality of the patient’s condition and their plan of care • Reports and alerts for missing or incomplete documentation • Can be accessed from a distance 49 Questions??? Contact Information: Colleen Williams, SLP, Clinical Specialist colleen.williams@aegistherapies.com Michelle Seeley, COTA, Director of Rehab michelle.seeley@aegistherapies.com 50 Thank you!