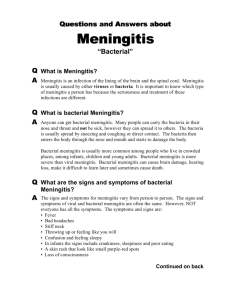
Meningitis
advertisement

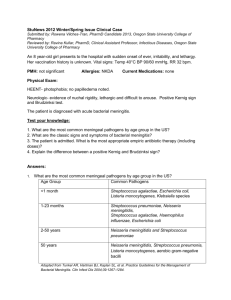
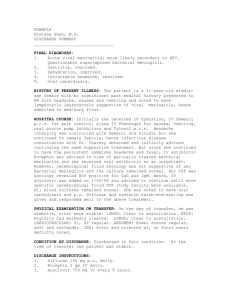
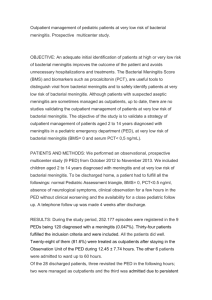
Meningitis A quick presentation of its bacterial form. - A Brief History Meningitis is caused by various types of microorganisms: • • • • • Bacterial Viral Fungal Parasitic Non-infectious Meningitis has been described by many people over the years and even dating back to Hippocrates over 25 centuries ago. In 1805, in Geneva, Switzerland, the first ever outbreak was recorded by Gaspard Vieusseux (17461814) and Andre Matthey (1778-1842) and the first in Africa was in 1840. However, it took another 40+ years before bacteria was linked to a cause of meningitis, by Anton Weichselbaum, an Austrian bacteriologist. In 1906, Simon Flexner, an American scientist, attempted a study using an anti-serum from horses, to treat meningitis and showed good success. With the development of penicillin, 1944 brought about a study confirming penicillin as a very effective treatment. Three major causes of bacterial meningitis include Streptococcus pneumoniae, Neisseria meningitides, Haemophilus influenzae type b. -A Recent Outbreak of Bacterial MeningitisSince January 13, 2015, six undergraduate students at the University of Oregon had come down with Meningococcal meningitis, type b. Recently, a 52 year old father visiting the campus has now tested positive. One of the undergraduate students passed away from the disease, but the other five students have since recovered. The sixth case was a 20 year old student who reported to an outpatient clinic with flu-like symptoms. The school has been attempting to vaccinate all their undergraduate students. As of June 2, 2015, only 10, 000 of the 22, 000 students have received the vaccine. With the recent infection of a girl’s father, it’s evidence that the disease is still present and that’s why the school is pushing for everyone to get vaccinated. Description of the Etiologic Agents and Virulence Factors As stated before, the three types of bacteria causing meningitis are: 1. Streptococcus pneumonia 2. Neisseria meningitides 3. Haemophilus influenzae type b Streptococcus pneumoniae: Virulence Factors: This is a lancet shaped gram-positive coccus that come in pairs or short chains and is the most common cause of bacterial meningitis, affecting mainly the elderly. They are usually anywhere from 0.5-1.2um. They are non-motile bacteria and our usually cultured on a blood agar plate. The cultures grow best at 35-37 ⁰C and will show small, grey, moist colonies and usually contain a zone of alpha-hemolysis. This bacteria has three main factors: This cerebrospinal fluid from a child with meningitis contains many neutrophils and oval gram-positive cocci singly and in pairs. • Cell wall – this serves to protect the bacteria from phagocytosis by white blood cells. • Pneumolysin – this does a variety of things, but including inhibits lymphocytes and antibody proliferation. • IgA protease – counteracts mucosal defenses. Growth of N. meningitidis on lower left and S. pneumoniae on upper left of a BAP Neisseria meningitides This is a gram-negative, coffee bean shaped diplococcus. They are roughly 0.6-1.0um. This particular bacteria typically causes meningitis in adolescents and young adults. They are nonmotile, aerobic bacteria. It is fastidious and grows best under 35-37⁰C. The cultures are usually grown on a blood agar plate and tend to present grey, round, smooth, and smooth with defined edges. Virulence Factors: • Cell wall - this serves to protect the bacteria from phagocytosis by white blood cells. • Capsule/Slime layer – this layer makes it more difficult for the phagocytes to engulf the bacteria. • IgA protease – counteracts mucosal defenses. • Endotoxin – lipopolysaccharides cause the white blood cells to release cytokines into the blood leading to vascular collapse and hemorrhages. Growth of N. meningitidis on lower left, S. pneumoniae on top, and H. influenzae on lower right of a CAP Haemophilus influenzae type b. This is a pleomorphic, Gram-negative bacilli or coccobacilli. It can grow as facultative anaerobe, but usually via aerobic. It lacks motility. Type b occurs mainly in children 5 and under and accounts for 95% of invasive disease. Haemophilus influenzae type b cultures appear as large, round, smooth, convex, colorless-to-grey, opaque colonies on a chocolate agar plate (the preferred medium). Virulence Factors: • Polyribosyl Ribitol Phosphate (PRP) capsule – Makes bacteria resistant to phagocytosis. • Cell wall – contains lipooligosaccharide which is similar to lipopolysaccharide, but shorter. • IgA protease – inhibits mucosal defenses. • Pili – these help the bacteria to bind to other cells and surfaces. This cerebrospinal fluid contains many neutrophils and gramnegative coccobacilli, primarily in the cytoplasm of the white cells. Meningitis: A Brief Description Bacterial meningitis is an infection that causes an inflammation of the meninges. The meninges are the membranous layers surrounding and protecting the brain and spinal cord. People often present with head aches, neck pain, fever, and nausea. Who is affected by which bacteria: • Children under 5 years of age – Haemophilus influenzae • Adolescents/young adults - Neisseria meningitides • Elderly - Streptococcus pneumoniae Steps to Invasion: 1) 2) 3) 4) Bacteria invades through the nasal mucosa Colonizes in the nasopharynx Disrupts the cilia and epithelial cells and invades the bloodstream Crosses the blood-brain barrier and enters the meninges of the brain and spinal cord. - Signs and Symptoms As stated before, the main symptoms are headache, sore/stiff neck, fever, and nausea. According to the Mayo Clinic they can also include: • Confusion • Difficulty sleeping • Sleepiness • Sensitivity to light *** In the case of Neisseria meningitides, the patient may develop skin rashes called petechiae. With babies these symptoms can also include poor eating, excessive crying, and a bulge in the soft spot at the top of a baby’s head. The cerebral spinal fluid of the meninges are a great place for bacteria to grow, due to lots of nutrients and few phagocytic cells. The bacteria help to damage the blood brain barrier allowing for cerebral edema, increased intracranial pressure. The meninges becomes inflamed and accumulating neutrophils have the capacity to destroy brain tissue, nerves, and blood vessels. Potential complications (according to Risk Factors: the Mayo Clinic: • Skipping Vaccinations • Hearing loss • Age (under 20 years old) • Brain damage • Living in a community setting (i.e. college dorms) • Kidney failure • Compromised immune system • Shock • Death Incubation Times: Neisseria meningitides - The average incubation period is 4 days, but can range between 2 and 10 days. Haemophilus influenzae - The incubation period is not certain, but could be as short as a few days. Streptococcus pneumoniae - The incubation period of pneumococcal pneumoniae is short, about 1 to 3 days. The germs that cause bacterial meningitis can be contagious. Some bacteria can spread through the exchange (e.g., by kissing) of respiratory and throat secretions (e.g., saliva or mucus). Fortunately, most of the bacteria that cause meningitis are not as contagious as viruses that cause the common cold or the flu. Also, the bacteria are not spread by casual contact or by simply breathing the air where a person with meningitis has been. Other meningitis-causing bacteria are not spread person-to-person, but can cause disease because the person has certain risk factors (such as a weak immune system or head trauma) Healthy people can carry the bacteria in their nose or throat without getting sick. Rarely, these bacteria can invade the body and cause disease. Most people who ‘carry’ the bacteria never become sick. Diagnostic Process: Four Main Ways to Diagnose Meningitis: • Blood Cultures – blood is drawn and cultured to see if microorganisms, and in particular bacteria, are growing. • Imaging – CT scans and MRIs can help detect inflammation in the head, sinuses, and spine. • Cerebrospinal Tap – The definitive diagnosis of meningitis requires an analysis of your cerebrospinal fluid (CSF), which is collected during a procedure known as a spinal tap. In people with meningitis, the CSF fluid often shows a low sugar (glucose) level along with an increased white blood cell count and increased protein. This test can also help distinguish which bacteria is causing meningitis. • Nasal swab – samples from the nasopharyngeal area are swabbed and stained. *** Gram staining is the stain used for diagnosis. MRI scan of frontal sinusitis, empyema, and abscess formation in a patient with bacterial meningitis. - Treatment and Prevention Prevention: • There are various vaccines for each bacterial strain that causes meningitis – 1. Neisseria meningitides – conjugated vaccine (also may use rifampin or tetracycline). The CDC recommends all college students be vaccinated for this bacterial strain. 2. Streptococcus pneumoniae – Prevnar 13 (children) and Pneumovax (adults) 3. Haemophilus influenzae – Hib vaccine (routine child vaccination) Other Precautions: 1. 2. 3. 4. Wash your hands Practice good hygiene Stay healthy Cover mouth when coughing and sneezing Treatment: For bacterial meningitis, antibiotics are effective. Often times, suspected bacterial meningitis will be treated with broad-spectrum antibiotics before confirming diagnosis. Meningococcal meningitis is of biggest concern and is often treated until ruled out. Cefotaxime is usually effective in all three bacteria, but Penicillin can be used with Neisseria meningitides. - Number of Cases Total in the United States - Due to Neisseria meningitides: Due to Haemophilus influenzae: Strain: 2010 2011 2012 2013 A, C, Y, W-135 280 257 161 115 Other serogroups 12 20 20 12 Type B 135 159 110 68 Unknown 406 323 260 310 2010 2011 2012 2013 23 14 30 19 *** Contrast this to the Democratic Republic of Congo, who the National Meningitis Association reported that there were 9339 cases of Meningococcal meningitis in 2013. *** According to the Centers for Disease Control. - Local Cases of Meningitis State of Oregon: Type: 2013 Neisseria meningitides 12 Haemophilus influenzae 138 (not necessarily caused meningitis Marion County: Type: 2013 Neisseria meningitides 3 Haemophilus influenzae 4 *** According to the Oregon Department of Health Why Should we spend money on research and prevention/treatment? Although other types of meningitis are usually less severe, it is important that we are up to date on our knowledge of bacterial meningitis (especially due to Neisseria meningitides). As stated before, if untreated, meningitis can cause hearing loss, brain damage, kidney failure, and even death. Bacteria have the capability to mutate over time and therefore keeping up with newer and more effective vaccines are extremely important. In sub-Saharan Africa, many of these countries have deaths due to meningitis in much greater numbers than the United States. Spending money to help vaccinate more people is also of vital importance. References: De Velasco, Alonso. (December 1995). Streptococcus pneumoniae: Virulence Factors, Pathogenesis, and Vaccines. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC239389/pdf/590591.pdf Identification and Characterization of Streptococcus pneumoniae. Retrieved from http://www.cdc.gov/meningitis/lab-manual/chpt08-id-characterization-streppneumo.pdf Identification and Characterization of Neisseria meningitidis. Retrieved from http://www.cdc.gov/meningitis/lab-manual/chpt07-id-characterization-nm.html Identification and Characterization of Haemophilus influenzae. Retrieved from http://www.cdc.gov/meningitis/lab-manual/chpt09-id-characterization-hi.html Community Acquired Pneumonia. Retrieved from https://meded.ucsd.edu/isp/1999/CAP/hflu.html Mayo Clinic Staff. (March 19, 2013). Diseases and Conditions: Meningitis. Retrieved from http://www.mayoclinic.org/diseases-conditions/meningitis/basics/definition/con-20019713 Bacterial Meningitis. (April 1, 2014). Retrieved from http://www.cdc.gov/meningitis/bacterial.html Epidemiology of Meningitis Caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenza. (April 1, 2014). Retrieved from http://www.cdc.gov/meningitis/lab-manual/chpt02-epi.html Cowan, Marjorie Kelly. Microbiology Fundamentals: A Clinical Approach. (2013). pp. 464-467. Meningococcal Meningitis. (February 2015). Retrieved from http://www.who.int/mediacentre/factsheets/fs141/en/ References Continued: Haemophilus influenzae Disease: Causes and Transmission. (April 2, 2014). Retrieved from http://www.cdc.gov/hi-disease/about/causes-transmission.html Pneumoccal Disease: Clinical Features. (June 10, 2015). Retrieved from http://www.cdc.gov/pneumococcal/clinicians/clinical-features.html 2015 Meningococcal Update. (May 29, 2015). Retrieved from https://public.health.oregon.gov/DiseasesConditions/DiseasesAZ/MeningococcalDisease/Pages/Meningococcal-Update.aspx