Central Nervous System Depressants. Anticonvulsants (Antiepileptic
advertisement

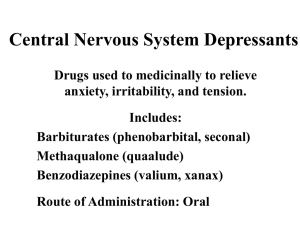
Central Nervous System Depressants CNS Depressants Sedatives • Drugs that have an inhibitory effect on the CNS to the degree that they reduce: – – – – Nervousness Excitability Irritability without causing sleep CNS Depressants Hypnotics • Calm or soothe the CNS to the point that they cause sleep CNS Depressants Sedative-Hypnotics—dose dependent: • At low doses, calm or soothe the CNS without inducing sleep • At high doses, calm or soothe the CNS • to the point of causing sleep Sedative-Hypnotics: Barbiturates • First introduced in 1903, standard agents for insomnia and sedation • Habit-forming • Only a handful commonly used today due in part to the safety and efficacy of: BENZODIAZEPINES Sedative-Hypnotics: Barbiturates Four categories: • Ultrashort – mephobexital, thiamylal, thiopental • Short – pentobarbital, secobarbital • Intermediate – aprobarbital, butabarbital • Long – phenobarbital Sedative-Hypnotics: Barbiturates Barbiturates have a very narrow therapeutic index. Therapeutic Index • Dosage range within which the drug is effective but above which is rapidly toxic. Sedative-Hypnotics: Barbiturates Mechanism of Action • Site of action: – Brain stem (reticular formation) – Cerebral cortex • By inhibiting GABA, nerve impulses traveling in the cerebral cortex are also inhibited. Sedative-Hypnotics: Barbiturates Drug Effects • Low doses: Sedative effects • High doses: Hypnotic effects (also lowers respiratory rate) Notorious enzyme inducers Sedative-Hypnotics: Barbiturates Therapeutic Uses • • • • Hypnotics Sedatives Anticonvulsants Surgical procedures Sedative-Hypnotics: Barbiturates Side Effects Body System Effects CNS Drowsiness, lethargy, vertigo mental depression, coma Respiratory Respiratory depression, apnea, bronchospasms, cough Sedative-Hypnotics: Barbiturates Side Effects Body System GI Other Effects Nausea, vomiting, diarrhea Agranulocytosis, vasodilation, hypotension, Stevens-Johnson syndrome Sedative-Hypnotics: Barbiturates Toxicology • Overdose frequently leads to respiratory depression, and subsequently, respiratory arrest. • Can be therapeutic: – Anesthesia induction – Uncontrollable seizures: “phenobarbital coma” Sedative-Hypnotics: Barbiturates Drug Interactions • Additive effects: – ETOH, antihistamines, benzodiazepines, narcotics, tranquilizers • Inhibited metabolism: – MAOIs will prolong effects of barbiturates • Increased metabolism: – Reduces anticoagulant response, leading to possible clot formation CNS Depressants: Benzodiazepines Most frequently prescribed sedative-hypnotics • • • • Most commonly prescribed drug classes Favorable side effects Efficacy Safety CNS Depressants: Benzodiazepines Classified as either: • Sedative-hypnotic or Anxiolytic (Medication that relieves anxiety) CNS Depressants: Benzodiazepines Sedative-Hypnotic Type • Long-Acting: – flurazepam (Dalmane), quazepam (Doral) • Short-Acting: – estazolam (Prosom), temazepam (Restoril), – triazolam (Halcion) CNS Depressants: Benzodiazepines Anxiolytic Type • alprazolam (Xanax) • chloridiazepoxide (Librium) • diazepam (Valium) • lorazepam (Ativan) • midazolam (Versed) zolpidem (Ambien) and zaleplon (Sonata) CNS Depressants: Benzodiazepines Mechanism of Action • Depress CNS activity • Affect hypothalamic, thalamic, and limbic systems of the brain • Benzodiazepine receptors CNS Depressants: Benzodiazepines Drug Effects • Calming effect on the CNS • Useful in controlling agitation and anxiety CNS Depressants: Benzodiazepines Therapeutic Uses • Sedation • • • • Sleep induction Skeletal muscle relaxation Anxiety relief Treatment of alcohol withdrawal • Agitation • Depression • Epilepsy • Balanced anesthesia CNS Depressants: Benzodiazepines Side Effects • Mild and infrequent Headache (nervousness) Drowsiness Dizziness Vertigo Lethargy Paradoxical excitement “Hangover effect” CNS Depressants: Nursing Implications • Before beginning therapy, perform a thorough history regarding allergies, use of other medications,health history, and medical history. • Obtain baseline vital signs and I & O, including supine and erect BPs. • Assess for potential disorders or conditions that may be contraindications, and for potential drug interactions. CNS Depressants: Nursing Implications • Give 15 to 30 minutes before bedtime for maximum effectiveness in inducing sleep. • Most benzodiazepines (except flurazepam) cause REM rebound and a tired feeling the next day; use with caution in the elderly. • Patients should be instructed to avoid alcohol and other CNS depressants. CNS Depressants: Nursing Implications • Check with physician before taking any other medications, including OTC medications. • It may take 2 to 3 weeks to notice improved sleep when taking barbiturates. • Abruptly stopping these medications, especially barbiturates, may cause rebound insomnia. CNS Depressants: Nursing Implications • Safety is important – Keep side rails up – Do not permit smoking – Assist patient with ambulation (especially the elderly) – Keep call light within reach • Monitor for side effects CNS Depressants: Nursing Implications • Monitor for therapeutic effects – – – – – Increased ability to sleep at night Fewer awakenings Shorter sleep induction time Few side effects, such as hangover effects Improved sense of well-being because of improved sleep Anticonvulsants and Drugs to Treat Other CNS Disorders Chapter 8 Topics • • • • • • • Epilepsy Parkinson’s Disease Myasthenia Gravis Attention-Deficit Disorders Amyotrophic Lateral Sclerosis (ALS) Multiple Sclerosis (MS) Alzheimer’s Disease Learning Objectives • Develop an understanding of the physiologic processes that occur in epilepsy. • Classify seizures and the goals of their therapy. • Understand that specific drugs are used in different classes of seizures. Learning Objectives • Be familiar with Parkinson’s disease and the drugs used in its treatment. • Know the symptoms and treatments of – myasthenia gravis – attention-deficit disorders – amyotrophic lateral sclerosis – multiple sclerosis – Alzheimer’s disease Epilepsy • Common neurologic disorder with sudden and recurring seizures • Caused by abnormal electrical impulses in the brain Epilepsy • In the U.S., 2.5 million people are affected. • Not all seizure disorders are epilepsy. Epilepsy Seizure Abnormal electrical discharges in the cerebral cortex caused by sudden, excessive firing of neurons – Result in a change in behavior of which the patient is not aware – While conscious, the patient may or may not lose movement control – Loss of body control may affect one area or the entire body Epilepsy Causes of Seizures • Imbalance of excitatory and inhibitory neurotransmitters: – Glutamate – inhibitory – GABA – excitatory – Other neurotransmitters can be involved • Neurotransmitter levels are controlled by enzymes • Disruption in enzymes = disruption of neurotransmitters Epilepsy Causes of Seizures • • • • • ETOH withdrawal Cardiovascular disease High fever Hypocalcemia High or low blood sugar • Hypoxia • Infection (meningitis) • Metabolic abnormalities • Brain tumor • Toxic substances • Trauma or injury to the head Epilepsy Classes of Seizures • Partial • Generalized Epilepsy Classes of Seizures • Partial – Simple-partial – Complex-partial • Generalized Epilepsy Classes of Seizures • Partial – Simple-partial – Complex-partial • Generalized – – – – Tonic-clonic or grand mal Absence or petit mal Myoclonic Atonic Epilepsy Partial Seizures • Localized in a specific area of the brain • Occurs with 65% of epileptic patients • Can progress to generalized seizures Epilepsy Partial Seizures • Simple-Partial • Complex-Partial Epilepsy Partial Seizures • Simple-Partial – No loss of consciousness – May have muscle twitching or sensory hallucinations • Complex-Partial Epilepsy Partial Seizures • Simple-Partial – No loss of consciousness – May have muscle twitching or sensory hallucinations • Complex-Partial – Impaired consciousness – With confusion, blank stare, and postseizure amnesia Epilepsy Generalized Seizures • Involves both hemispheres of the brain, not one specific location • Types – – – – Tonic-Clonic Absense Myoclonic Atonic Generalized Seizures Tonic-Clonic Seizures • Tonic – body becomes rigid, lasts a minute or less • Clonic – initiated with muscle jerks, and may be accompanied by shallow breathing, loss of bladder control, and excess salivation Generalized Seizures Absence • Interruption of activities by blank stare, rotating eyes, uncontrolled facial movements, rapid eye blinking, and/or jerking of an arm or leg • No generalized convulsions • Usually lasts 30 seconds or less • Many times it progresses to tonic-clonic as the patient gets older Generalized Seizures Myoclonic • Occurs with sudden, massive, brief muscle jerks or non-massive, quick jerks • Consciousness is not lost • Can occur during sleep Generalized Seizures Atonic • Begins with sudden loss of muscle tone and consciousness • Muscles relax, limbs go limp • Lasts a few seconds to a minute, then patient can resume standing and walking Generalized Seizures Status Epilepticus • Continuous tonic-clonic seizures with or without return to consciousness • High fever and lack of oxygen severe enough to cause brain damage or death Discussion What percentage of status epilepticus patients die, regardless of treatment? Discussion What percentage of patients status epilepticus patients die, regardless of treatment? Answer: 10% Antiepileptic Drug Therapy Goals of Therapy 1. Seizure control or lessen the frequency 2. Prevent emotional and behavioral changes Discussion Note: 30% of patients are not compliant due to side effects (sedation and loss of cognitive processes). What are some possible strategies health care providers can use to help improve drug therapy compliance? Antiepileptic Drug Therapy Neuronal Activity 1. Polarized (resting) 2. Depolarized (firing) 1. Sodium and calcium enter the cell 2. When sufficient amounts cross, neurotransmitters are released 3. Neurotransmitter release leads to firing of the neuron 3. Repolarization (return to resting) Antiepileptic Drug Therapy Abnormal Neuronal Activity • Depolarization If excessive neurotransmitters are released it leads to uncontrollable firing of the neuron = seizure • Treatment Block the firing of the neuron by raising the threshold of depolarization Antiepileptic Drug Therapy • Start with monotherapy at a low dose and titrate up slowly • Medication must be maintained at steady therapeutic levels (no missed doses) • Polytherapy can be used if sufficient response is not seen with monotherapy Antiepileptic Drug Therapy Problems with Therapy • Wrong medication is used for the seizure type • Side effects may cause problems with patient compliance • If doses are missed, there is an increased risk of seizure activity Drug List Anticonvulsants • • • • • • • carbamazepine (Epitol, Tegretol) clonazepam (Klonopin) diazepam (Valium) divalproex (Depakote) ethosuximide (Zarontin) Fosphyenytoin (Cerebyx) gabapentin (Neurontin) Drug List Anticonvulsants • • • • • • lamotrigine (Lamictal) levetiracetam (Keppra) lorazepam (Ativan) oxcarbazepine (Trileptal) phenobarbital (Luminal Sodium) phenytoin (Dilantin) Drug List Anticonvulsants • • • • primidone (Mysoline) topiramate (Topamax) valproic acid (Depakene) zonisamide (Zonegran) Therapeutic Regimens for Seizures Seizure Type 1st Line 2nd Line 3rd Line Partial Tegretol or Dilantin Neurontin Luminal, or Lamictal Mysoline, or Depakene Absence Zarontin or Depakene Depakene Klonopin Atonic, Atypical Absence, Myoclonic Klonopin or Lamictal Therapeutic Regimens for Seizures 1st Line 2nd Line Tonic-Clonic, Tonic, Clonic Tegretol, Dilantin, or Depakene Luminal or Mysoline Status Epilepticus Valium, Ativan, or Dilantin Seizure Type 3rd Line valproic acid (Depakene) and divalproex (Depakote) • Increases the availability of GABA (inhibitory) • Take with water, not a carbonated drink • Do not use aspirin Dispensing Issues Warning! • Depakote and Depakene can easily be confused. • Be careful with Depakote and Depakote ER. • Depakote ER is only once a day. phenytoin (Dilantin) • May be used to prevent seizures • Promotes sodium outflow from cells – stabilizes the neuronal membrane • Be cautious of drug interactions • Intravenous phenytoin must be mixed carefully Phenytoin Side Effects Dose Related – – – – – – Ataxia Diplopia Dizziness Drowsiness Encephalopathy Involuntary movements Phenytoin Side Effects Non-Dose-Related – Gingival hyperplasia – Peripheral neuropathy – Vitamin deficiencies Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Cerebyx (anticonvulsant) – Celexa (antidepressant) – Celebrex (for pain and arthritis) carbamazepine (Epitol, Tegretol) • Has effect on sodium channels which may alter synaptic transmission. • Blood monitoring must be done regularly. • Be cautious of interactions and side effects. gabapentin (Neurontin) • Used in conjunction with other medications • No significant drug interactions • Used for many other disorders, particularly neuropathic pain Dispensing Issues Warning! Neurontin (anticonvulsant) and Noroxin (antibiotic) are sound-alike drugs, but they are easy to distinguish by strength. clonazepam (Klonopin) • Only indication is prophylaxis of seizures • Depresses nerve transmission in the motor cortex • C-IV controlled substance (benzodiazepine) Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Lamictal (anticonvulsant) – Lamisil (antifungal) – Lomotil (for diarrhea) topiramate (Topamax) • Is thought to alter sodium channels and thereby increases GABA activity and decreases glutamine activity • Causes significant cognitive effects • Drink fluids to decrease risk of kidney stones Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Kaletra (antiviral for HIV) – Keflex (antibiotic) – Keppra (anticonvulsant) Discussion Which neurotransmitters play the greatest role in seizures? Discussion Which neurotransmitters play the greatest role in seizures? Answer • Glutamate (excitatory) • GABA (inhibitory) Parkinson’s Disease • Characteristic Signs – Resting tremor – Rigidity – Akinesia • Usually affects people over 60 Parkinson’s Disease Physiology • Result of pathologic alterations in the extrapyramidal system (part of the CNS that controls motor activities) • Distinguishing feature: Lewy bodies (protein masses) found in the midbrain Parkinson’s Disease Physiology • Normal muscle movement requires balance of dopamine (inhibitor) and ACh (stimulator) • In the substantia nigra, enough dopamine is released to counteract the effects of ACh • In parkinsonism, enough dopamine is not released which leads to excessive motor nerve stimulation Cutaway View of the Brain Substantia Nigra Parkinson’s Disease Drug Therapy • Improves the functional ability and clinical status of patients • Aims at symptomatic relief, does not alter the disease process • Patients may have temporary or prolonged remission • Side effects can be a problem Drug List Anti-Parkinson Agents • • • • • • amantadine (Symmetrel) benztropine (Cogentin) bromocriptine (Parlodel) entacapone (Comtan) levodopa (Dopar) levodopa-carbidopa (Sinemet) Drug List Anti-Parkinson Agents • • • • • • levodopa-carbidopa-entacapone (Stalevo) pergolide (Permax) pramipexole (Mirapex) ropinirole (ReQuip) selegiline (Eldepryl) tolcapone (Tasmar) levodopa (Dopar) • Metabolized to dopamine in the brain, but the brain does not receive a full dose • Drug has very undesirable effects • After about 5 years of therapy, 2/3 of patients experience “on-off” phenomenon levodopa-carbidopa (Sinemet) • Probably the most common drug used for parkinsonism • Carbidopa allows for lower doses of levodopa to be used which decreases side effects Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Amantadine (for Parkinson’s) – Ranitidine (for the stomach) – Rimantadine (for the flu) entacapone (Comtan) • Indicated for patients who have a deteriorating response to levodopa • Less toxic than tolcapone • Take without regard to food Discussion What are the two primary neurotransmitters involved in Parkinson’s disease and what role do they play? Discussion What are the two primary neurotransmitters involved in Parkinson’s disease and what role do they play? Answer • ACh (excitatory) • Dopamine (inhibitory) Myasthenia Gravis • Autoimmune disorder of the neuromuscular junction • ACh receptors are destroyed at the motor end plate • Characterized by weakness and fatigability, especially of the skeletal muscles Motor End Plate Myasthenia Gravis Presenting Signs • Ptosis (drooping eyelid) • Diplopia (double vision) • Dyarthria (speech) • Dysphagia (swallowing) Myasthenia Gravis Treatment Blocking the destruction of ACh causes improvement for the patient Drug List Myasthenia Gravis Agents • • • • • azathioprine (Imuran) cyclophosphamide (Cytoxan) edrophonium (Enlon, Reversol) neostigmine (Prostigmin) pyridostigmine (Mestinon) pyridostigmine (Mestinon) • Blocks destruction of ACh • Allows for ACh accumulation at the synaptic junction cyclophosphamide (Cytoxan) • Prevents cell division by targeting the autoimmune portion of the disease • Use chemotherapeutic precautions Attention-Deficit Disorders • Attention-Deficit Hyperactivity Disorder (ADHD) • Attention-Deficit Disorder (ADD) Attention-Deficit Disorders Attention-Deficit Hyperactivity Disorder (ADHD) Characterized by purposeless, chronic, pervasive, driven behavior that affects a child in social, emotional, and academic settings. Attention-Deficit Disorders Attention-Deficit Hyperactivity Disorder (ADHD) Characteristics for Assessment – Hyperactivity – Impulsivity – Distractibility Attention-Deficit Disorders Attention-Deficit Disorder (ADD) • Has less hyperactivity • Child is more lethargic and more easily distracted • Both disorders are more common in boys than girls • Some symptoms can persist into adulthood Drug List Attention-Deficit Disorder Agents • • • • • atomoxetine (Strattera) clonidine (Catapres, Catapres-TTS) desipramine (Norpramin) dexmethylphenidate (Focalin), C-II dextroamphetamine-amphetamine (Adderall), C-II Drug List Attention-Deficit Disorder Agents • imipramine (Tofranil) • methylphenidate (Concerta, Metadate, Ritalin, Ritalin-SR), C-II • nortriptyline (Aventyl, Pamelor) • pemoline (Cylert), C-IV methylphenidate (Concerta, Metadate, Ritalin, Ritalin-SR) • C-II controlled substance • Drug of choice to treat ADD, ADHD, and narcolepsy • Increases levels of neurotransmitters in the brain • Concerta is a QD dose – outer shell dissolves to release medication immediately, then drug is slowly released through pores in the tablet dextroamphetamine-amphetamine (Adderall) • C-II controlled substance • Effects last about 6 hours • Primary side effect is depression Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Adderall (ADD, ADHD) – Inderal (anxiety, hypertension) atomoxetine (Strattera) • Nonstimulant inhibitor of norepinephrine reuptake • Controls impulsivity and activity • Not a controlled substance, so refills can be called in • Side effects: weight loss and slowed growth Dispensing Issues Warning! Look-Alike and Sound-Alike Drugs – Clonidine (ADD, ADHD) – Klonopin (seizures) Discussion Compare and contrast ADHD and ADD. Discussion Compare and contrast ADHD and ADD. Answer • ADHD – hyperactivity, impulsivity, and distractability • ADD – more lethargic and easily distracted Amyotrophic Lateral Sclerosis (ALS) • Known as Lou Gehrig’s disease • Progressive degenerative disease of the nerves • Leads to muscle weakness, paralysis, and eventually death • Caused by excessive levels of glutamate Drug List ALS Agent • riluzole (Rilutek) riluzole (Rilutek) • First drug approved for ALS • Inhibits release of glutamate • Shown to improve survival rate by 3 months is some patients Multiple Sclerosis (MS) • Autoimmune disease in which myelin sheaths degenerate • Patient loses use of muscles and often eyesight is affected • Some drugs can slow progression, but there is no cure Drug List MS Agents • • • • • • baclofen (Lioresal) glatiramer acetate (Copaxone) interferon beta-1a (Avonex, Rebif) interferon beta-1b (Betaseron) mitoxantrone (Novantrone) tizanidine (Zanaflex) interferon beta-1a (Avonex, Rebif) • • • • Used for ambulatory patients Reduces frequency of attacks Delays disability Drug should be taken at night with APAP to prevent flu-like side effects baclofen (Lioresal) • Skeletal muscle relaxant • Inhibits transmission of reflexes at the spinal cord • Onset requires three to four days Alzheimer’s Disease • • Degenerative disorder of the brain that leads to progressive dementia and changes in personality and behavior Progression 1. Minor forgetfulness 2. Inability to complete complex tasks 3. Complete incapacitation, disorientation, and failure to thrive Alzheimer’s Disease • There are no treatments that can reverse this disease • Depression should be treated according to symptoms Drug List Alzheimer’s Agents • • • • • • donepezil (Aricept) galantamine (Reminyl) ginkgo memantine (Namenda) rivastigmine (Exelon) tacrine (Cognex) donepezil (Aricept) • Convenient with few side effects • Improves memory and alertness • Give once a day at bedtime memantine (Namenda) • May have fewer side effects than other drugs • Approved for moderate to severe conditions • Evidence that the drug does slow disease rivastigmine (Exelon) • Has fewer interactions than Aricept • More difficult to dose and administer Discussion How does Alzheimer’s disease affect patients’ families? Has the disease affected someone in your family? Discussion Several of the diseases presented in this chapter are degenerative and there is yet no known cure. How might this affect patients with a diagnosis of one of these conditions?