HuP 191B – Advanced Assessment of Upper Extremity Injuries
advertisement

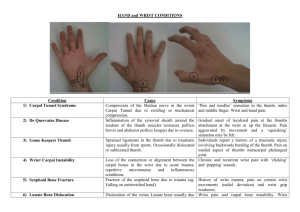
HuP 191B – Advanced Assessment of Upper Extremity Injuries Wrist, Hand and Finger Evaluation and Pathologies History History Location of pain Mechanism of injury/etiology Unusual sounds/sensations Onset/duration and description of symptoms Prior history/general health concerns Location of Pain Generally, local injury represented by local symptoms – sometimes difficult to identify specific structure/s Must be aware of possible referred pain from cervical, shoulder and/or elbow pathologies Mechanism of Injury Direct trauma Hyperextension/hyperflexion injuries of wrist and/or fingers Insiduous onset increases likelihood of chronic conditions Identify factors which increase or decrease symptoms Unusual Sounds or Sensations Numbness/tingling indicative of neurological pathology – must establish if local or referred Fractures, dislocations and tendon ruptures often accompanied by “popping” sensation Some overuse conditions (tendonitis) may present with “snapping” sensation Onset/Duration and Description of Symptoms Type of pain (ache, throb, etc.) Intensity of pain (objectify) Immediate vs. gradual onset of symptoms Changes in symptoms (better, worse) Prior History and General Health Concerns Any previous injury, especially if neurological in nature, may have lasting effect on function, etc. Hand is typically first part of body to be affected by: – Arthritis – Peripheral vascular disease (PVD) Insufficient vascular structures to provide adequate circulation – Raynaud’s phenomenon Reaction to cold temps – alternating bouts of pallor and cyanosis (vascular responses) Inspection/Observation Inspection/Observation General inspection Inspection of wrist and hand Inspection of thumb and fingers General Inspection Hand posture – Relaxed normal hand is slightly flexed with subtle palmar arch Gross deformity – Associated with fractures and/or dislocations Palmar creases – May not be visible if severe swelling Cuts, scars, lacerations – Superficial nature of neurovascular structures makes them susceptible to injury even with superficial wounds Inspection of Wrist and Hand Distal radioulnar continuity Carpal and metacarpal continuity/contour MP joint alignment – Depressed knuckle = Boxer’s fracture Wrist and hand posturing – Neurovascular conditions may prompt abnormalities (drop wrist, Volkmann’s ischemic contracture) Inspection of Wrist and Hand Ganglion cyst – Defined as benign collection of thick fluid within a tendinous sheath or joint capsule – Most commonly found in wrist and hand – Painful with motions that impinge upon when symptomatic Inspection of Thumb and Fingers Skin and fingernails – Subungual hematoma – Paronychia – infection at nail periphery – Felon – infection/abscess at or distal to DIP Finger alignment and deformity – If finger out of alignment, may be spiral fracture of phalanx/metacarpal – Secondary to fracture, dislocation or tendon injury Skin and Fingernail Conditions Palpation Palpation Wrist and finger flexors Wrist and finger extensors Bony anatomy – Non-carpal bones – Carpal bones Ligamentous and intrinsic muscular structures Wrist and Finger Flexors Flexor carpi ulnaris tendon Flexor carpi radialis tendon Tendons of finger flexors – Superficialis vs. profundus Palmaris longus tendon Wrist and Finger Extensors Extensor digitorum tendons Anatomical snuffbox – Extensor pollicis longus – medial (ulnar) border – Abductor pollicis longus and extensor pollicis brevis – lateral (radial) border – Scaphoid - floor Anatomic Snuffbox Non-Carpal Bony Anatomy Distal radius/radial styloid process Lister’s tubercle (dorsal and distal radius) Ulnar head/ulnar styloid process Metacarpals Phalanges Carpal Bony Anatomy Scaphoid – Floor of snuffbox, easier with ulnar deviation Lunate – Typically aligned with 3rd metacarpal, distal to Lister’s tubercle and flex wrist Triquetrum – Just distal to ulnar styloid process Pisiform – Small, rounded prominence at proximal aspect of hypothenar eminence in palm Carpal Bony Anatomy Trapezium – Between scaphoid and 1st metacarpal Trapezoid – Base of 2nd metacarpal Capitate – Move toward thumb from hamate, base of 3rd metacarpal Hamate – “hook” of hamate is large prominence at distal hypothenar eminence on palm Ligamentous and Intrinsic Muscular Anatomy Radial collateral ligaments – Radiocarpal joint, MP/IP/PIP/DIP joints Ulnar collateral ligaments – Ulnocarpal joint, MP/IP/PIP/DIP joints Carpal tunnel (transverse carpal ligament) Thenar eminence Hypothenar eminence Range of Motion Range of Motion Active/passive/resistive – Wrist Flexion/extension, ulnar/radial deviation – Thumb (carpometacarpal joint)\ Flexion/extension, abduction/adduction, opposition – Fingers MP joints: flexion/extension, abduction/adduction IP/PIP/DIP joints: flexion/extension Wrist Ranges of Motion Flexion – normally 80-90 degrees, firm end feel Extension – normally 75-85 degrees, firm end feel Radial deviation – normally 20 degrees, hard end feel (scaphoid on radial styloid) Ulnar deviation – normally 35 degrees, firm end feel Wrist Ranges of Motion Thumb Ranges of Motion Flexion – normally 60-70 degrees, soft end feel Extension – 0 degrees, firm end feel Abduction – 70-80 degrees, firm end feel Adduction – 0 degrees, soft end feel Opposition – flexion/adduction/rotation, touch thumb to little finger, firm end feel Thumb Motions Finger Ranges of Motion MP joints – Flexion – 85-105 degrees, hard end feel (proximal phalanges on distal metacarpal) – Extension – 20-30 degrees, firm end feel – Abduction/adduction – total of 20-25 degrees, firm end feel IP/PIP/DIP joints – Flexion – IP: 80-90 degrees, PIP: 110-120 degrees, DIP: 80-90 degrees, firm end feels except PIP is hard end feel (middle phalanges on proximal phalanges) – Extension – 0 degrees, firm end feels Ligamentous/Capsular Testing Ligamentous/Capsular Testing Carpal glide tests – Attempts to elicit abnormal glide of carpal bones Varus/valgus stress tests (do at multiple joint positions) – Wrist UCL limits radial deviation and flexion/extension RCL limits ulnar deviation and flexion/extension Can also assess with glide between radius/ulna and proximal row of carpal bones – MP/IP/PIP/DIP joints Thumb UCL is common injury site Neurovascular Evaluation Neurological Evaluation Peripheral nerve distributions – Median, ulnar and radial nerve sensory and motor functions Nerve root level distributions – Dermatomes and myotomes Vascular Evaluation Radial artery Capillary refill Skin temperature and color Allen test? Pathologies Pathologies Wrist injuries Hand injuries Finger injuries Thumb injuries Wrist Injuries Wrist sprains Triangular fibrocartilage complex (TFCC) injury Carpal tunnel syndrome Wrist fractures Scaphoid fractures Lunate/perilunate dislocations Neurological injuries Wrist Sprains Most common etiology is hyperflexion or hyperextension (fall on outstretched arm) Must rule out carpal fracture, neurological injury and TFCC injury before assessing as wrist sprain Most common presentation involves limited ROM to all wrist movements due to pain, usually also presents with weakness – assess with radiocarpal and carpal glide tests - treated conservatively in nearly all cases TFCC Injury Sprain to ligamentous structures on dorsal and medial aspect of wrist – injury occurs acutely, but often not reported until later Most common etiology is hyperextension with ulnar deviation Presents with tenderness to dorsal medial wrist distal to ulna, limited ROM (especially radial and ulnar deviation), possibility of avulsion fracture Must be referred to MD – often surgically repaired TFCC Injury Carpal Tunnel Syndrome Compression of median nerve in carpal tunnel – must be able to differentiate from nerve root injury Typically secondary to overuse conditions (tendonitis, etc.) but may be due to acute trauma Most common presentation is neurological deficit/symptoms to median nerve distribution (sensory and motor) Carpal Tunnel Syndrome Evaluate with Tinel’s sign to carpal tunnel – positive if symptoms reproduced Evaluate with Phalen’s test – wrist flexion for ~1 minute – positive if symptoms reproduced Almost always treated conservatively initially with rest, splinting (night), NSAIDs Failure of conservative measures can lead to surgery – resection of transverse carpal ligament Phalen’s Test Wrist Fractures Typically occur from fall on outstretched arm – must consider neurovascular implications Colles’ fracture – Fracture of distal radius proximal to radiocarpal joint with dorsal displacement of fracture Smith’s fracture (reverse Colles’) – Fracture of distal radius proximal to radiocarpal joint with palmar/volar displacement of fracture Colles’ Fracture Smith’s Fracture Scaphoid Fracture Easily the most commonly fractured carpal bone Most common etiology is hyperextension Blood supply comes from distal aspect and fracture in mid-substance often compromises proximal blood supply – high incidence of nonunion/malunion fractures Scaphoid Fracture Scaphoid Fracture Common presentation is pain/tenderness to snuffbox, limited ROM due to pain (especially extension/radial deviation), decreased grip strength Conservative management involves immobilization of wrist/thumb/forearm for 6-8 weeks, then progressive ROM/strengthening exercises Surgical intervention occasionally done in acute situation, but usually after failed conservative approach Perilunate and Lunate Dislocations Hyperextension is mechanism of injury – leads to 2 dislocation types (progressive severity of injury): perilunate dislocation vs. lunate dislocation Common presentation is either palmar or dorsal wrist pain/swelling, visible/palpable deformity, 3rd knuckle level with others, neurological symptoms (3rd finger) Perilunate Dislocation Palmar/volar displacement of proximal row of carpal bones on lunate so that lunate is dorsal to the other bones Rupture of palmar/volar radiocarpal ligaments and promimal row of carpals “stripped” away from lunate May spontaneously reduce, but usually remains displaced Perilunate Dislocation Lunate Dislocation Palmar/volar displacement of lunate relative to carpals (really vice versa – carpals displaced dorsally on lunate) Further hyperextension forces ruptures dorsal radiocarpal ligaments and the carpals are subsequently displaced May spontaneously reduce, but usually remains displaced Lunate Dislocation Perilunate and Lunate Dislocations If closed reduction is stable, immobilized in slight flexion for 6-8 weeks – regular reevaluation to maintain reduction stability Requires surgical stabilization if closed reduction not stable acutely or if conservative attempts fail Neurological Injuries Median nerve – carpal tunnel syndrome Ulnar nerve – Passes in tunnel of Guyon between hook of hamate and pisiform, can be compressed Radial nerve – Drop wrist syndrome from inability to extend wrist/fingers if radial nerve injured Hand and Finger Injuries Metacarpal fractures Collateral ligament injuries Posturing and deformities Finger fractures Dislocations Metacarpal Fractures Etiology is direct trauma – injury to 4th and 5th are most common – Boxer’s fracture: 5th metacarpal fracture with “depression or shortening” of knuckle Often reports of hearing/feeling “pop or snap” at time of injury Common presentation is localized tenderness/swelling/crepitus, possible displacement, abnormal hand ROM, weakness to affected area Boxer’s Fracture Metacarpal Fractures Metacarpal Fractures If no displacement, treat with cast immobilization for 4-6 weeks followed by progressive ROM/flexibility/strengthening If displacement and/or fragmented, surgical intervention necessary to re-establish normal anatomical positioning – then treated same as conservative approach Collateral Ligament Injuries Etiology is acute force application Present with localized pain/swelling, ROM limited due to pain/swelling Varus and valgus stress tests often not informative unless 3rd degree injury Generally conservatively managed with splint and symptomatic treatment Posturing and Deformities Ape hand Bishop’s deformity Claw hand Dupuytern’s contracture Swan neck deformity Volkmann’s ischemic contracture Boutonniere deformity Trigger finger Posturing and Deformities Ape hand – Median nerve inhibition resulting in thenar eminence atrophy – inability to flex and oppose thumb Bishop’s deformity – Ulnar nerve inhibition resulting in hypothenar eminence, interossei, and medial 2 lumbricale atrophy – 4th and 5th fingers assume flexed posture Claw hand – Ulnar and median nerve pathology resulting in flexion of PIP and DIP joints with associated extension of MP joints Dupuytren’s Contracture Flexion contracture of MP and PIP joints from shortening/adhesions in palmar aponeurosis – most common at 4th and 5th fingers Swan-Neck Deformity Flexion of MP and DIP joints with associated hyperextension of PIP joint – usually due to volar plate injury, but can have many causes Volkmann’s Ischemic Contracture Flexion contracture of wrist and fingers from decreased blood supply to forearm muscles secondary to fracture, dislocation or compartment syndrome Boutonniere Deformity Extension of MP and DIP joints with associated flexion of PIP joint – due to rupture of extensor tendon from middle phalanx causing it to slip laterally at PIP joint changing line of pull from extension to flexion Trigger Finger “Locking” of ROM during finger flexion from adhesions in flexor tendon sheaths With flexion movements, adhesions require additional effort to allow for flexion ROM Tendon “release” often presents as an audible “snap” as finger moves into flexion Trigger Finger Finger Fractures Distal phalanx most commonly fractured due to flexor/extensor tendon attachments (avulsion) and crushing trauma Middle phalanx uncommonly injured Proximal phalanx injury usually not isolated and has associated tendon and/or skin injury Presentation and treatment similar to metacarpal fracture discussion Finger Fracture Finger Fractures Avulsion fractures of the fingers – Mallet finger Avulsion of extensor tendon from distal phalanx, inability to actively extend DIP joint (passive OK), commonly occurs if fingertip hits ball – Jersey finger Avulsion of profundus tendon from distal phalanx, inability to actively flex DIP joint if PIP joint stabilized, commonly occurs when grabbing jersey and joint forcefully extended against active motion Mallet Finger Jersey Finger Finger Dislocations Interphalangeal joint dislocations result in obvious deformity Must rule out associated fracture – refer to MD for imaging prior to reduction Generally, easy to reduce – must be splinted after reduction Finger Dislocations Thumb Injuries DeQuervain’s syndrome Sprains MP joint dislocations Fractures DeQuervain’s Syndrome Tenosynovitis of extensor pollicis brevis and abductor pollicis longus tendons from repetitive stress (radial deviation) Presents with pain/swelling to proximal thumb/distal radius, pain with radial/ulnar wrist deviation and thumb extension and abduction Treated conservatively with rest (immobilization), NSAIDs, modalities DeQuervain’s Syndrome Finkelstein’s Test Evaluative for DeQuervain’s syndrome Thumb flexed across palm and locked in by finger flexion – wrist placed in ulnar deviation – positive if pain reproduced or increased Can present with false-positive results Finkelstein’s Test Thumb Sprains Medial (ulnar) collateral ligament of 1st MP joint is easily most commonly injured – must rule out avulsion fracture May be due to repetitive stress, but typically etiology is acute hyperextension and/or hyperabduction (skiing, etc.) – Gamekeeper’s thumb Thumb Sprains Commonly presents with localized tenderness/swelling, may see ecchymosis in thenar eminence, inability to pinch or grasp objects, positive valgus stress test If mild or moderate injury with good end point, often treat conservatively with splint for 4-6 weeks If rupture, early surgical intervention indicated to provide acceptable joint stability 1st MP Joint UCL Sprain 1st MP Joint Dislocation Etiology usually hyperextension and/or hyperabduction – may have associated fracture Rupture of volar (palmar) ligamentous structure Presents with obvious deformity and inability to perform ROM Refer to MD for reduction Thumb Dislocation Thumb Fractures 1st metacarpal fractures due to acute trauma If fracture extends into articular surface (joint space), known as Bennett’s fracture Bennett’s fracture often requires surgical intervention to fixate fracture segment to allow for normal bony alignment and stability Bennett’s Fracture