Osteoporosis Update - Amazon Web Services
advertisement

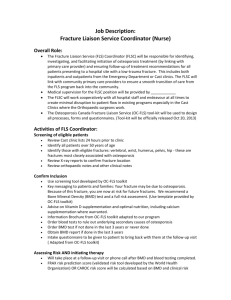
FLS in the USA ISCD Annual Meeting February 26-28, 2015 Chicago, IL, USA E. Michael Lewiecki, MD New Mexico Clinical Research & Osteoporosis Center University of New Mexico School of Medicine Albuquerque, NM Disclosure Institutional Grant / Research Support Amgen, Eli Lilly, Merck Scientific Advisory Boards / Consulting Amgen, Eli Lilly, Merck, Radius Health, AgNovos Healthcare, NPS Outline • Identify incentives and barriers for FLS in the USA • Describe strategies for initiating FLS • Understand available FLS resources Why do we need FLS in the US? • Current management of high risk patients is poor • FLS can reduce fracture risk in high risk patients • It is cost-effective • Financial penalties for not doing it and incentives for doing it well Osteoporosis Treatment After Hip Fx Review of US insurance claims data (commercial + Medicare) in 96,887 patients hospitalized with hip fracture, 2002-2011 Solomon DH et al. J Bone Miner Res. 2014;29:1929–1937. 2014 HEDIS Report Card HEDIS measure The percentage of women age ≥ 67 years with a fracture who had either a BMD test or prescription for a drug to treat or prevent osteoporosis in the 6 months after the fracture. http://www.ncqa.org/ReportCards/HealthPlans/StateofHealthCareQuality/2014TableofContents/ Post-fracture Bermuda Triangle Interested in surgery Orthopedic Surgeon Limited time, clinical uncertainty, competing priorities Limited availability, patient not referred Patient Bone Disease Specialist Primary Care Provider Other Barriers to Osteoporosis Care in the USA • DXA – Limitations of insurance overage – Low reimbursement • Bone turnover markers – Declared experimental by major insurers – High cost • Medications – Limitations of insurance coverage – High cost for some “Tex” FLS is Cost-effective in Integrated Healthcare Systems • Kaiser Southern California Healthy Bones Program – Identifying and treating high risk patients reduced hip fracture risk by 37%, preventing 935 hip fractures in 2006, saving $30.8 million – Dell R et al. J Bone Joint Surgery Am. 2008;980(Suppl 4):188-194 • Geisinger Health System Osteoporosis Disease Management Program – Identifying and treating high risk patients reduced fracture-related expenses by $7.8 million over 5 years – Newman ED et al. Osteoporos Int. 2003;14:146-151 Kaiser Permanente Estimation of FLS Cost Savings If implemented nationally, the Kaiser strategy could reduce the annual number of hip fractures in the USA by over 100,000 and save over $5 billion/year in fracture related expenses NBHA Estimation of Cost Savings • For every 100 patients in FLS, 1 hip fracture and 2-3 other fractures are prevented, with cost savings of $35,000 to $40,000 • If FLS coordinator manages 500 patients, then 5 hip fractures and 10-15 other fractures will be prevented, saving $175,000 to $200,000 • Markov computer simulation model • Projection of lifetime costs and benefits of FLS in men and women with hip fracture • Assumptions – CNP FLS coordinator paid ~ $100,000/yr. – 42% of patients treated with BP with 58% adherence at 1 yr. – Estimated that CNP could manage 500-1000 patients/yr. Solomon DH et al. J Bone Miner Res. 2014;29:1667-1674. FLS is Cost-effective in the USA • FLS results in 153 fewer fractures, 37 more QALYs, and saves $66,879 per 10,000 post fracture patients compared with typical care • With 2.5 million osteoporotic fractures per year in the USA, total annual cost savings: up to $16.7 million Solomon DH et al. J Bone Miner Res. 2014;29:1667-1674. Financial Drivers of FLS • US healthcare reform (“Affordable Care Act”) is transforming the healthcare system from fee for service to paying for quality, outcomes and care coordination • Centers for Medicare & Medicaid Services (CMS) initiatives include: – – – – – – Accountable Care Organizations Patient-Centered Medical Home model Bundled payment initiatives Qualified Clinical Data Registries (QCDR) Medicare Advantage “5 Star” program Meaningful use electronic medical record incentive program FLS Effectiveness Depends on Its Intensity Review of published literature: Fully coordinated, intensive models of post-fracture care are more effective in improving patient outcomes than approaches involving alerts and/or education only. Ganda K et al. Osteoporos Int. 2013;24:393-406. Osteoporosis Canada. “Make the FIRST break the LAST with Fracture Liaison Services”. FLS Resources • International Osteoporosis Foundation (IOF) – Capture the Fracture – www.iofbonehealth.org/capture-fracture • National Bone Health Alliance (NBHA) – Fracture Prevention Central – www.nbha.org/fpc • American Orthopaedic Association (AOA) – Own the Bone – www.ownthebone.org History of NBHA Created from 2 major bone health activities 2004 2008 FLS Timeline NBHA launch 2010 NBHA/Kaiser FLS Summit 2Million2Many launch Fracture Prevention CENTRAL launch QCDR Osteoporosis Registry launched (September) 2011 2012 2013 2014 FLS Demonstration Project (December) NBHA Now • Public-private partnership to improve the bone health of all Americans • 55 organizational participants – 35 non-profit member organizations – 16 private sector member organizations – 4 government agency liaisons (CDC, FDA, NASA, NIH) • Collective reach of over 100,000 health care professionals and 10 million consumers FLS Demonstration Project • 15 month demonstration project to assess performance improvement with FLS at 3 clinical sites - started December 2013 • Sponsored by NBHA/NOF and CECity (software company for healthcare performance improvement) • Funded by grant from Merck • Uses FLS app on CECity MedConcert platform (suite of apps) – – – – Automates data collection into central registry Benchmarks performance against core measures Enables transition of care from hospital to outpatient Provides prompts to coordinators for next step in care Demonstration Sites • Alegent Creighton Health/Catholic Health Initiatives (Omaha, NE) – Robert Recker, MD • Georgetown University Hospital/MedStar Health (Washington, DC) – Andrea Singer, MD • University of Pittsburgh Medical Center (Pittsburgh, PA) – Susan Greenspan, MD Completion date: April 2015 Report and manuscript: June 2015 Ostonics Quality Solutions • Joint venture LLC with NOF and CECity • Goal: 20% reduction in osteoporotic fractures in the US by 2020 (20/20) • Methods: Develop FLS software tools based on experience from demonstration sites Achieving 20/20 Vision • Currently 200 FLS programs in the USA • Need 800 more (1000 total) to reach the goal of 20% fracture reduction by 2020 • American Orthopedic Association FLS quality improvement initiative launched in 2009 • Currently implemented in more than 140 hospitals and medical practices • OTB subscribers receive ….. – Comprehensive start-up materials – Access to a national Web-based registry with reporting and benchmarking capabilities – Best practice library – Patient and physicians education tools – Public relations tools) – Web-based training – Ongoing best-practice sharing – E-newsletters www.ownthebone.org Challenge: Healthcare Capitalism • Convincing hospital administrators with limited resources and competing priorities • Convincing physicians this is not competition for patients • Conflicting financial interests with open (fragmented) healthcare delivery Funding Questions • Who pays for the nurse coordinator and computer systems to identify and manage fracture patients? • What is the return on investment for a hospital? • Won’t the hospital, orthopedists, and surgical support staff lose money if there are fewer admissions for fractures? Business Considerations with Initiation of FLS • Income at risk with current care – Medicare incentives and disincentives • FLS expenses – Nurse coordinator – Computer and software • Potential new income sources – Reimbursement for DXA – Reimbursement for coordinator services Projected Income and Expenses Capital Expenses Computer hardware and software (assume DXA already owned by hospital) $ Recurring Expenses FLS coordinator salary and benefits $ Clerical support $ IT support $ Patient education materials (development and distribution) $ Facility overhead (room, equipment, supplies, etc.) $ Revenue FLS coordinator insurance billing $ Additional DXA studies $ Additional outpatient appointments $ Additional treatment (injectables) $ Medicare penalties avoided and incentives received $ Revenue Surplus $ Intangible benefits: fractures prevented, community goodwill, public relations Hospital-based FLS From Fracture Prevention Central. NBHA Business Plan Template. FLS Coordinator Reimbursement Model Fracture patient admitted to ER or physician’s office • Hospital: EMR diagnosis and age trigger FLS Coordinator • Physician office: Office alerts FLS Coordinator Patient admitted to hospital for surgery (e.g. hip fracture) Upon identification, FLS Coordinator: • Meets with patient to review program, possible cost sharing • Collects patient medical history and enrolls patient through the FLS program website; an ID number is assigned to the patient • Begins patient tracking Osteoporosis / low bone mass confirmed by medical history FLS coordinator1 visit for osteoporosis assessment Patient treated for fracture and released (e.g., wrist fracture) Fracture patient discharged to home or FAC facility Osteoporosis / osteopenia not confirmed by medical history • If confirmed, assess patient’s treatment plan and adherence • If not confirmed, order tests and begin optimal treatment regimen as necessary FLS Coordinator services may be performed in person or over the phone. • If in person, report the appropriate CPT code(s) from the following range: ‒ 99204, 99205, 99211-99215 (Office or outpatient)2 ‒ 99218-99226, 99231-99236 (Inpatient hospital) ‒ 99238-99239 (Hospital discharge day management) ‒ 99241-99245, 99251-99255 (Office and inpatient consultation)3 ‒ 99281-99285 (Emergency department) ‒ 99304-99310, 99315-99316, 99318 (Nursing facility management) ‒ 99324-99328, 99334-99337 (Long-term care facility E/M) ‒ 99341-99345, 99347-99350 (Home visit E/M) ‒ 99386, 99387, 99396, 99397, 99401-99404 (Prevention & risk factor reduction)3 ‒ 99495-99496 (Transitional care management)4 • If by phone, report the appropriate CPT code(s) from the following range: ‒ 99441-99443 (Telephone E/M service)3 ‒ 99487-99489 (Complex chronic care coordination)3 ‒ 99495-99496 (Transitional care management)4 ** Appended appropriate modifiers as necessary. Providers should confirm with facility and payers that services are reimbursable; if services are not reimbursable, FLS Coordinator must inform patient of potential financial responsibility** ≤4 weeks of discharge Obtain and interpret testing, determine appropriate management and initiate treatments in consultation with patient’s healthcare provider At discharge, FLS Coordinator: • Determines patient’s post-fracture location (i.e., inpatient stay, home, other PAC facility) and performs a fracture prevention assessment • Identifies patient’s PCP or other appropriate chronic care professional to order post-fracture tests, medications and develops patient care plan • Distributes patient education material from FLS stakeholders and champions 1 FLS Coordinator should be an allied health professional certified by CMS or other organization to be determined CPT codes 99213 and 99214 are typically used by specialists and may require 24 modifier (unrelated E/M service by same physician or qualified health professional during a postoperative period) 3 Not currently reimbursed by Medicare 4 Typically reported by PCPs 2 ≤8 weeks of discharge (and every 6 weeks until 6 months) Contact patient by phone to encourage medication adherence, answer questions and discuss fall prevention ≤6 months of discharge At 6 months and 1 year Obtain appropriate laboratory testing (e.g., BMD test, blood and urine) Ongoing patient assessment (i.e., reevaluation, repeat BMD tests, chronic health visits) EMR: Electronic Medical Record PAC: Post-Acute Care PCP: Primary Care Physician BMD: Bone Mineral Density E/M: Evaluation and Management Current Procedural Terminology (CPT®) is a registered trademark of the American Medical Association (AMA). Reimbursement for FLS Coordinator Services • CPT codes for face-to-face services – – – – – – – – – – • 99204, 99205, 99211-99215 (Office or putpatient) 99218-99226, 99231-99236 (Inpatient hospital) 99238-99239 (Hospital discharge day management) 99241-99245, 99251-99255 (Office and inpatient consultation) 99281-99285 (Emergency department) 99304-99310, 99315-99316, 99318 (Nursing facility management) 99324-99328, 99334-99337 (Long-term care facility E/M) 99341-99345, 99347-99350 (Home visit E/M) 99386, 99387, 99396, 99397, 99401-99404 (Prevention & risk factor reduction) 99495-99496 (Transitional care management) CPT codes for telephone services – 99441-99443 (Telephone E/M service) – 99487-99489 (Complex chronic care coordination) – 99495-99496 (Transitional care management) Use appropriate modifiers as necessary. Providers should confirm with facility and payers that services are reimbursable; if services are not reimbursable, FLS Coordinator must inform patient of potential financial responsibility. Pathway to FLS Local Champion Passionate, Perseverant, Persuasive Medical Director (Medical Rationale) Nurse Coordinator Hospital Administrator (Business Model) Systems Infrastructure Community Support Archived Webinar Series Available on Demand • • • • • • • • • • Introduction to Fracture Prevention CENTRAL/the Fracture Liaison Service Model Implementing a Secondary Fracture Prevention Program Convincing Administration to Support Your Fracture Prevention Program FLS Implementation in an Orthopaedic Practice Setting FLS Implementation in a Rheumatology/Endocrinology Practice Setting 2014/FLS Implementation in a Primary Care Setting Setting Up Your Fracture Liaison Service Program for Success Health Care Quality 101: What, Why and How How Transitioning to ICD-10 Coding Will Impact Your Osteoporosis Practice NBHA/NOF Qualified Clinical Data Registry (2 webinars) www.nbha.org/fpc/educational-webinars Learn More About FLS • ISCD Annual Meeting – Chicago, IL – Postconference Symposium – NOF FLS Model of Care Training – Sunday, March 1, 2015 (8:00 AM – 12:30 PM) • NOF Interdisciplinary Symposium on Osteoporosis (ISO) – Washington, DC – Preconference Symposium – NOF FLS Model of Care Training – Tuesday, May 19, 2015 (7:30 – 12:30 pm)