Repatriation General Hospital Falls Assessment Clinic
advertisement

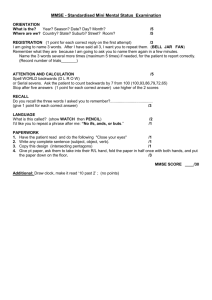
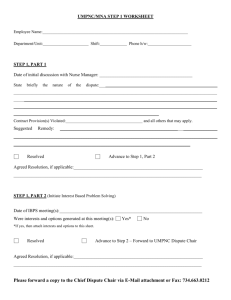
Repatriation General Hospital Falls Assessment Clinic Falls Assessment Clinic The RGH Falls Assessment Clinic provides specialised multidisciplinary assessments for older clients with more complex needs around falls prevention. The program is for older adults living in the community who have more complex issues around falls and frailty who would benefit from a comprehensive assessment and coordination of falls prevention services. What does the service offer? The service offers a specialised, comprehensive, Geriatrician led multidisciplinary assessment: • To identify falls risk factors • Offer services/interventions to address these risk factors • Access to a specialised Day Rehabilitation Service (FIT Program) • To link in with other community services as required • Follow up with geriatrician as required What is the criteria for referral? • • • • • • • • Need for more detailed specialist medical assessment Uncertain diagnosis Unexplained falls/gait disturbances Untreated osteoporosis Declining function with mod-severe disability Unexplained syncope or collapse Complex medication issues Cognitive issues affecting mobility Falls Clinic Decision Making Support Protocol This flow chart provides information on the most appropriate service to meet the patient’s needs, depending on their presentation. Assessments used • The following assessments will be used in the clinic to assess the patient: • Subjective assessment • Mini Mental State Examination (MMSE) • Mini Nutritional Assessment (MNA) • Modified Falls Efficacy Scale (MFES) • Timed Up and Go (TUG) • OT / Continence screen • Lying and standing BP Then: Goal Setting Case Conference Discussion Subjective Assessment Falls Clinic FIT Screening Falls History Number of falls: Have you had near misses? Yes How often? Have you sustained any injuries from falls? No Pattern and History of Falls: Mobility What walking aids do you use? Indoors: Outdoors: Are you able to get up off the floor on your own? Yes No Do you have any pain, stiffness, weakness or lack of sensation in your legs or feet? (check footwear) Yes No Do you have difficulty with or avoid walking in the community? (eg steps, slopes, uneven ground, shopping centres, catching your toes on obstacles) Yes No Do you participate in any regular exercise or activity programs or have you in the past? What are your goals? Gait/Other balance: Yes No Falls Clinic FIT Screening TUG : BP: Lying Standing- During assessment, did the patient show any signs of cognitive deficit? MMSE score: Referral To OT indicated: Yes/No MNA score: Referral to Dietitian indicated: Yes/No Other comments: Appropriate for FIT Yes/No Plan: Signed: Date: Mini Mental State Examination (MMSE) • The Mini Mental State Examination (MMSE) is a valid and reliable instrument used to screen for cognitive impairment in older adults.. • The MMSE provides a global score of cognitive ability that correlates with function in activities of daily living • The MMSE measures various domains of cognitive function including orientation to time and place; registration; concentration; short-term recall; naming familiar items; repeating a common expression; and the ability to read and follow written instructions, write a sentence, construct a diagram, and follow a three-step verbal command. • The MMSE takes approximately 10 minutes to administer, provides a baseline score of cognitive function, and pinpoints specific deficits that can aid in forming a diagnosis • Click on the following website for more information on administering the MMSE. • http://www.unc.edu/~vreddy/index_fil es/Medical%20Resources/Clinical%20To pics//Geriatrics/MMSE%20MANUAL.pdf Mini Nutritional Assessment (MNA) • The Mini-Nutritional Assessment Short-Form (MNA®-SF) is a screening tool used to identify older adults (> 65 years) who are malnourished or at risk of malnutrition. • The MNA®-SF is based on the full MNA®, the original 18-item questionnaire published in 1994 by Guigoz, et al. • The MNA®-SF consists of 6 questions on food intake, weight loss, mobility, psychological stress or acute disease, presence of dementia or depression, and body mass index (BMI). When height and/or weight cannot be assessed, then an alternate scoring for BMI includes the measurement of calf circumference. • Scoring: • Scores of 12-14 are considered normal nutritional status; • 8-11 indicate at risk of malnutrition; • 0-7 indicate malnutrition. http://consultgerirn.org/uploads /File/trythis/try_this_9.pdf Modified Falls Efficacy Scale (MFES) • The Modified Falls Efficacy Scale (MFES) is a 14 item questionnaire, asking participants to rate their level of confidence on how they are able to undertake each activity without falling, on a scale of 0 (not confident at all) to 10 (completely confident). • Higher scores reflect more confidence and less fear of falling • Lower scores reflect less confidence and more fear of falling • An overall score is calculated by averaging the scores for all items which were rated (ie – score out of 10). • The test takes approximately 5 minutes to administer Timed Up and Go (TUG) • The Timed Up and Go test (TUG) is a simple test used to assess a person's mobility, requiring both static and dynamic balance. • The TUG measures the time that a person takes to rise from a chair, walk three metres, turn around, walk back to the chair, and sit down. During the test, the person is expected to wear their regular footwear and use any mobility aids that they would normally use. • The TUG is used frequently in the elderly population, as it is easy to administer and can generally be completed by most older adults. Timed Up and Go (TUG) Instructions: The person may wear their usual footwear and can use any assistive device they normally use. 1. Have the person sit in the chair with their back to the chair and their arms resting on the arm rests. 2. Ask the person to stand up from a standard chair and walk a distance of 10 ft. (3m). 3. Have the person turn around, walk back to the chair and sit down again. Timing begins when the person starts to rise from the chair and ends when he or she returns to the chair and sits down. The score is written in seconds. Predictive Results Seconds Rating • <10 Freely mobile • <20 Mostly independent • 20-29 Variable mobility • >20 Impaired mobility Podsiadlo, D., Richardson, S. The timed ‘Up and Go’ Test: a Test of Basic Functional Mobility for Frail Elderly Persons. Journal of American Geriatric Society. 1991; 39:142-148 OT / Continence Screen • Information on home environment, activity limitations, current supports, previous falls and ability to seek help, as well as continence issues, need to be obtained in order to determine if further advice or intervention is required. The following checklist provides a framework for identifying these issues. Measuring BP • A lying and standing BP needs to be measured on each patient. Goal Setting Following the assessment process, goal setting needs to be undertaken with each patient. • What does the patient feel is their main concern? What are their goals? • Are these goals realistic? • What is the best service to meet these goals? Case Conference Using the Falls Clinic Decision Making Support Protocol, provide a brief plan of action for the patient(s) you have assessed. For example, • Mrs X needs to be referred to a community therapy service because she has had 2 falls in the past year however she is currently independent at home with no significant decline in function. She would benefit from an ongoing community exercise program to maintain strength and balance. • Mr M has had 2 falls in his bathroom and 1 in the garden the past 6 months. He has no equipment in place, his toilet is off the back veranda, he has urge incontinence, poor vision and is malnourished. He would benefit from a FIT referral for multidisciplinary team input.