Preventive Services Improvement Initiative
advertisement

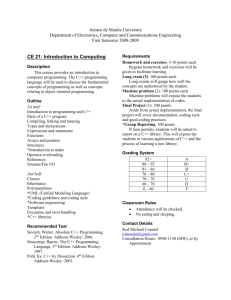
Coding 101 The Partnership TOT, September 22, 2008 Taken from “Beginning Coding”, “Intermediate Coding”, and “I Hate Coding” by Dianne Demers Welcome and Expectations 2 Objectives The Participant will be able to ● Define CPT, ICD 9, and DSM 4 Coding ● Explain the reasons why appropriate coding and documentation is so important in SBHC settings. ● Demonstrate correct use of CPT and ICD 9 codes ● Explain the rational for conducting routine medical record review and coding compliance audits in SBHC settings 3 Coding Background and Terminology 4 Coding Definition Coding is an alphanumeric system used to translate medical procedures and services into data 5 Types of Coding Current Procedural Terminology (CPT) International Classification of Diseases (ICD-9 Clinical Modification - CM) Diagnostic and Statistical Manual of Mental Disorders (DSM IV-TR) 6 Coding Is Not The Same As Billing 7 Coding is Medicare Drive Pediatrics was not considered in original coding guidelines, so some of the things we do in SBHCs may not fit well 8 SBHC Coding There is no difference between coding in a SBHC and any other setting – the coding assumptions are the same. You provide the same level of care regardless of the location. 9 Why Code Correctly? ● Reimbursement depends on it. ● Codes describe the services you provide ● Codes justify these services ● Services not documented “never happened” PS: Never code for the purpose of getting more money 10 The Coding Process has 2 Parts 1. “What you did” = CPT 2. “Why you did it” = ICD-9 or DSM-4 TR YOU MUST ALWAYS USE BOTH a what and a why (NO EXCEPTIONS) 11 When a provider is undercoding they tell the wrong story This wrong story is: SBHC Providers are seeing very few patients with multiple problems. SBHC Providers should see more patients since they are not seeing complicated patients. The SBHC should decrease the number of physicians and add more mid-level providers. 12 There Are Two Coding Guidelines - 1995 & 1997 Both 1995 and 1997 guidelines are approved for use by CMS Agencies may specify use of 1995 or 1997 guidelines 1997 guidelines are more specific than 1995 in the examination portion (they are more computer friendly) New guidelines have been proposed, but have not yet been accepted 13 Coding Guidelines 1995 vs. 1997 This lecture is based on the 1995 guidelines because they are 15 pages long vs. 57 pages of the 1997 version. www.cms.hhs.gov/MLNProducts/Download s/1995dg.pdf 14 Fraud Intentional deception or misrepresentation ● Deliberately billing for services not performed ● Unbundling of services ● Intentionally submitting duplicate claims 15 Abuse Improper billing practices ● Billing for non-covered services ● Misusing codes on a claim form 16 Errors Accept it, you will make them. Your best defense is having a plan for your coding and being able to explain it. 17 Coding Does Not Equal Good Medicine 18 But - Coding is Good Documentation 19 CPT Codes document: Level of Service Procedures Provided 20 Examples of CPT codes Evaluation & Management 99211 99212 99213 99214 99215 Preventive Health 99391 99392 99393 99394 99395 99397 99397 21 ICD-9 and DSM4 Codes document: The reason behind the visit (They must support the CPT codes) 22 General Coding Principles Coding gets you paid for your services Coding can be used to justify the need for services to your funders 23 Coding with ICD-9 ICD-9 codes have 3, 4 or 5 digits ● The greater the number of digits, the higher the specificity ● Use a 5-digit code when it exists ● Use a 4-digit code only if there is no 5digit code with the same category ● Use a 3-digit code only if there is no 4digit code within the same category PS: Omitting the required 4th or 5th digit will result in the denial of a claim. Do not add any additional digits, even zero 24 ICD-9-CM Codes Range from 001.0 to V82.9 They identify: ● Diagnoses ● Symptoms ● Conditions ● Problems ● Complaints ● Other reason for the procedure, service, or supply provided 25 ICD-9-CM Codes Three volumes ● Volume 1 Tabular List of Diseases ● Notes all exclusive terms and 5th-digit instructions ● Volume 2 Alphabetic Index of Diseases ● Does not contain detail – Do Not code from this volume ● Volume 3 Procedures ● Used almost exclusively for hospital services PS: (All 3 Volumes are generally found in one binding) 26 “V” Codes For circumstances other than disease or injury Three categories: ● Problem – Could affect overall health status, but is not a current illness or injury ● Ex.: V14.2 Personal history of allergy to sulfonamines ● Service – Circumstances other than illness or injury ● Ex.: V68.1 Issue of a repeat prescription ● Factual – Certain facts that do not fall into the “problem” or “service” categories 27 “V” Codes Can be used as a: ● Solo Code ● Principal code ● Secondary code May represent check-ups, screenings, administrative requests, prescription refills 28 Rules for Coding Outpatient Visits 29 Determine Type of Office Visit Evaluation and Management New Patients vs. Established Patients Preventive Health Visits New Patients vs. Established Patients Counseling Visits Medical Visit – talker only Mental Health Visits New Patients vs. Established Patients 30 Determine Medical Necessity Services are reasonable and necessary for the diagnosis and treatment of illness or injury. All payors define necessity differently Clinical rationale must be documented through coding. You cannot write more, to get paid more. 31 Determine Chief Complaint The reason for the patient’s visit ● S of a SOAP note Codes used must relate to chief complaint or they are invalid And, the chief complaint must be documented in the chart 32 Evaluation/Management (E / M) Services Used for acute care visits Five levels of service Seven components within the levels ● Key components – history, exam and medical decision making ● Contributory components – counseling, coordination of care, nature of presenting problem, and time 33 Evaluation/Management (E / M) Services Beginning information about coding deals with the three key components: ● History ● Examination ● Medical Decision Making 34 Evaluation/Management (E / M) Services There are 5 Levels of service 1. Minimal 2. Self-Limited or Minor 3. Low Severity 4. Moderate Severity 5. High Severity 35 CPT Codes Used for E/M Visits New Patients Level 1 Level 2 Level 3 Level 4 Level 5 99201 99202 99203 99204 99205 Established Patients 99211 99212 99213 99214 99215 37 Coding Steps 38 Coding Steps First Step - Determine if your patient is: A New Patient or An Established Patient 39 Definition of a new patient: It is the patient’s first visit to the provider The patient has not received any professional services from the provider or another provider of the same specialty who belongs to the same group practice, within the past three years. PS: Any time a patient is seen in an Emergency Room they are considered a new patient 40 If your patient does not meet the definition of a New Patient, then they are an Established Patient 41 Coding Steps Second Step - determine the level of service for the visit, To do this you need to determine the level of service for each key component separately There are 3 key components They are: 1. History (HPI, ROS, PFSH) 2. Examination 3. Medical Decision Making 42 Coding Steps New Patients Within the 3 key components, there are 5 levels of service Remember to Consider the Key Components separately: ● HPI, ROS, PFSH ● Examination ● Medical Decision Making 43 Example - New Patient The Level of Service for a new patient visit is determined by the lowest level of service (1 through 5) of the three key components HPI, ROS, PFSH 4 Examination 4 3 Medical Decision Making This is the lowest level 44 Coding Steps Established Patients Again Consider the Key Components Separately: ● HPI, ROS, PFSH ● Examination ● Medical Decision Making The level of service (1 – 5) is determined by the level that appears in 2 of the three components, or by the middle level 45 Example – Established Patient HPI, ROS, PFSH 3 This is the middle level EXAM 2 Medical Decision Making 4 46 Why is this? 47 Answer . . . There has to be a system, and this is what AMA came up with. 48 Coding Jeopardy/ Match Game 49 How to Steps of Coding 50 How to Steps of Coding: Determine Level of Medical Decision Making Determine Level of History Component Determine Level of Physical Examination (You will need to reference the chart – examination notes for this) 51 Determine Level of Medical Decision Making Medical Decision Making consists of three sections: ● Diagnosis or Management Problems ● Diagnostic Procedures ● Treatment of Management Options Level is determined by the level found in two of the three categories – or the middle number if all three are different 52 Determine Level of Medical Decision Making Section I: Diagnosis or Management of Problems 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 One selflimited or minor problem Two or more selflimited or minor problems One stable chronic condition Acute uncomplicated illness One or more chronic illnesses with complications Two or more stable chronic conditions Undiagnosed new problem w/uncertain prognoses Acute illness with systemic symptoms One or more chronic illness with severe complications Acute or chronic illness or injury that is life or limb threatening Abrupt change in neurologic status Acute complicated injury 53 Determine Level of Medical Decision Making Section II: Diagnostic Procedures 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 Lab X-ray EKG UA Ultrasound, etc. Venipuncture KOH Physiologic tests not under stress Pulmonary Function Barium Enema Arterial puncture Skin biopsies Physiologic tests under stresscardiac stress tests Diagnostic endoscopies with no risk factors Deep needle or incisional biopsy Obtained fluid from body Cardiovascular imaging with contrast Cardiovascular imaging with contrast Invasive diagnostic tests Cardiac Electrophysiological tests Diagnostic endoscopies with identified risk factors Discography 54 Determine Level of Medical Decision Making Section III: Treatment or Management Options 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 Rest Gargles Elastic bandages Dressings OTCs Minor surgery PT OT IVs without additives Minor surgery with risk factors Elective major surgery— no risk factors Prescription drug management IV fluids with additives Closed facture or dislocation treatment w/o manipulation Therapeutic nuclear medicine Elective Surgery with identified risk factors Emergency major surgery Parenteral controlled substances Drug treatment requiring intensive monitoring Decision not to resuscitate or deescalate care because of poor prognosis 55 How to Steps of Coding: Determine Level of History Component History component consists of three sections: ● History of Present Illness (HPI) ● Review of Systems (ROS) ● Patient, Family, and Social History (PFSH) 56 Determine Level of History Component Section I: History of Present Illness Location Quality Severity Duration Timing Context Modifying factors Associated signs and symptoms 57 Determine Level of History Component Section II: Review of Systems Constitutional symptoms (fever, wt loss, etc.) Eyes Ears, nose, mouth, throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Integumentary (skin and/or breast) Neurologic Psychiatric Endocrine Hematologic/lymphatic Allergic/immunologic 58 Determine Level of History Component Section III: Patient, Family and Social History Past medical history ● Medication allergies Patient’s family history Patient’s social history ● Age-appropriate review of past and current activities ● Tobacco usage 59 History Component Matrix (Number of components of each HPI, ROS & PFSH required for each level) New 99201 99202 99203 99204 99205 Established 99211 99212 99213 99214 99215 HPI 0 1 1 4 4 ROS 0 0 1 2 10 PFSH 0 0 0 1 2 60 How to of Coding Steps: Determine Level of Physical Examination Constitutional Eyes Ears, Nose, Mouth, Throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskletal Skin Neurologic Psychiatric Hematologic/Lympatic/Immunologic 61 Determine Level of Physical Examination: # of body systems required for each level New 99201 99202 99203 99204 99205 Established 99211 99212 99213 99214 99215 Exam 0 1 4 5 8 62 Coding Matrix Example: New Patient History 3 Established Patient 3 Exam 2 2 Medical Decision Making Level of Coding 3 3 2 3 63 Coding Matrix Example: History New Patient Established Patient 4 4 Exam 2 2 Medical Decision Making 4 4 Level of Coding 2 4 64 Coding Exercise 65 Coding Exercise for Evaluation/ Management Services Suzy Q is a 16 y/o female with c/o severe “female” cramps - worse than usual. She states she took Midol and it only helped a little. She is a new patient. Document on the exam and encounter form to a level 3, using audit sheet as reference. 66 67 68 How to Verify this is correct level of documentation to support level 3 69 70 Count the components HRI 1 - Midol Exam 1-const Med Decision ROS 1 - cramps 2-Abd - acute/uncomp PFSH - 0 3-back - OTCs 4-genito ___________ ____________ ___________ Level 3 Level 3 Level 3 71 72 Preventive Services 73 Preventive Services These visits include a comprehensive history and examination, as well as appropriate counseling/anticipatory guidance/risk factor reduction, interventions, and the ordering of age-appropriate laboratory/diagnostic procedures. 74 Preventive Services “Comprehensive” in a preventive service examination is not synonymous with a “comprehensive” E/M examination. 75 Preventive Service Codes Age <1 1-4 5-11 12-17 18-39 40-64 65+ New 99381 99382 99383 99384 99385 99387 99387 Established 99391 99392 99393 99394 99395 99397 99397 76 Preventive Services Appropriate ICD-9 codes would be: V20.2 for a Routine Infant or Child Health Check V70.3 for a Sports Physical 77 Preventive Services Additional services provided at the time of the visit should be reported with their specific CPT codes listed separately: ● Examples: ● Snellen Test ● Laboratory ● Immunizations ● Administration of Immunizations 78 Mental Health Services 79 How do you document mental health services? Who documents mental health services? Where are mental health services documented? ● (mental health chart, medical record, both charts, log sheet, database, encounter form) How do mental health providers and primary care providers share information about mental health services? “We can’t bill for mental health services, so why code?” You should still document in order to: ● Justify your position ● Assess mental health problems of school population ● Track treatment ● Track compliance ● Assist in measuring outcomes ● Demonstrate a need for mental health reimbursement Documentation Where to document codes? • • Encounter Form Database BOTH (if separate): mental health chart AND medical record Mental Health Diagnostic Codes Anxiety Disorders 300.01 Panic Disorder Without Agoraphobia 300.21 Panic Disorder With Agoraphobia 300.22 Agoraphobia Without History of Panic Disorder 300.29 Specific Phobia Specify type: Animal Type/Natural Environment Type/Blood-Injection-Injury Type/Situational Type/Other Type 300.23 Social Phobia Specify if Generalized 300.3Obsessive-Compulsive Disorder Specify if With Poor insight 309.81 Posttraumatic Stress Disorder Specify if Acute/Chronic Specify if With Delayed Onset 308.3 Acute Stress Disorder 300.02Generalized Anxiety Disorder 300.00Anxiety Disorder NOS Depressive Disorders 296.xx Major Depressive Disorder ● .2x Single Episode ● .3x Recurrent 300.4 Dysthymic Disorder Specify if Early Onset/Late Onset Specify With Atypical Features 311 Depressive Disorder NOS Disruptive Behavior Disorders 314.xx Attention-Deficit/Hyperactivity Disorder ● .01 Combined Type ● .00 Predominantly Inattentive Type ● .01 Predominantly Hyperactive-Impulsive Type 314.9 Attention-Deficit/Hyperactivity Disorder NOS 312.xx Conduct Disorder ● .81 Childhood-Onset Type ● .82 Adolescent-Onset Type ● .89 Unspecified Onset 313.81 Oppositional Defiant Disorder 312.9 Disruptive Behavior Disorder NOS Substance Abuse/Dependence 303.90 Alcohol Dependence/305.00 Alcohol Abuse 304.00Amphetamine Dependence/305.70 Amphetamine Abuse 304.30 Cannabis Dependence/305.20 Cannabis Abuse 304.20 Cocaine Dependence/305.60 Cocaine Abuse 304.50 Hallucinogen Dependence/305.30 Hallucinogen Abuse 304.60 Inhalant Dependence/305.90 Inhalant Abuse 305.1 Nicotine Dependence 304.00 Opioid Dependence/305.50 Opioid Abuse 304.60 Phencyclidine Dependence/305.90 Phencyclidine Abuse 304.10 Sedative, Hypnotic, or Anxiolytic Dependence/305.40 Sedative, Hypnotic, or Anxiolytic Abuse 304.80 Polysubstance Dependence 304.90 Other (or Unknown) Substance Dependence 305.90 Other (or Unknown) Substance Abuse The following specifiers apply to Substance Dependence as noted: With Psychological Dependence/Without Psychological Dependence Early Full Remission/Early Partial Remission/Sustained Full Remission/Sustained Partial Remission In a Contained Environment On Agonist Therapy Mental Health Procedural Codes Evaluation & Management (E&M) Codes 99201 – 99215 New and Established Patient Office Visits 99241 - 99245 Consultations 99361 - 99362 Case Management Services, Team Conferences 99371 - 99373 Case Management Services, Telephonic Mental Health Procedure Codes 90801 - 90802 Psychiatric Diagnostic or Evaluative Interview Procedures 90804 - 90829 Psychotherapy 90804 - 90815 Office or Other Outpatient Facility 90810 - 90815 Interactive Psychotherapy 90816 - 90829 Inpatient Hospital, Partial Hospital or Residential Care Facility 90845 - 90857 Other Psychotherapy 90862 - 90889 Other Psychiatric Services or Procedures Psychiatric Therapeutic Procedures CPT Codes 90804 – 90889 Psychotherapy is the treatment for mental illness and behavioral disturbances in which the clinician establishes a professional contract with the patient and, through definitive therapeutic communication, attempts to alleviate the emotional disturbances, reverse or change maladaptive patterns of behavior, and encourage personality growth and development. E&M Codes and MH Codes The Evaluation and Management services should not be reported separately, when reporting codes: 90805, 90807, 90809, 90811, 90813, 90815, 90817, 90819, 90822, 90824, 90827, 90829. Reimbursement – who can bill? What are the rules governing who can bill for mental health diagnosis/treatment in your state? ● Most states accept physicians (MD), clinical psychologists (CP), licensed clinical social workers (LCSW) ● However, each State has its own rules and many will pay for other professionals Coverage Issues A provider should know what services are covered. Services must be documented and medically necessary in order for payment to be made. Do you, as a provider, know if all services provided are covered? Are you documenting properly, and what about this “medically necessary” bit? How Much are you Paid? Reimbursement ● Reductions in reimbursement rates by provider type Physician ● Clinical Psychologist ● LCSW ● Other ● - not discounted - discounted - further discounted - discounted if covered Reimbursement Issues E&M codes are limited to physicians, PAs, NPs, nurses Same is true for 90805, 90807, 90809 codes An E&M (992XX) and a therapy (908XX) cannot be billed on the same date of service to most Medicaid programs Documentation and Coding: Fraud and Abuse Services MUST be medically necessary (determined by payers based on a review of services billed) Music, game, instrument, pet interaction therapies, sing-alongs, arts and crafts, and other similar activities should not be billed as group or individual activities. Services performed by a non-licensed provider particularly as “incident to” using the PIN of the licensed provider Elements of “Incident To” An integral part of the physician’s professional service Commonly rendered without charge or generally not itemized separately in the physician’s bill Of a type that are commonly furnished in physician’s office or clinic Furnished under the physician’s direct personal supervision Action Steps for Mental Health Coding Improvements T Questions to Answer What criteria must programs (SBHC) meet in order to provide behavioral health services? What providers are eligible to provide behavioral health services? What are your state’s credentialing and licensing requirements for providers of behavioral health services? What credentialing and licensing requirements are necessary for billing in your state? What are the guidelines for billing services as “incident Review Program Services Define the Behavioral/Mental Health Services your students are receiving Determine if there are additional Behavioral/Mental Health Services you want to provide Review and Modify Encounter Form Does encounter form include both diagnostic and procedural codes that would be used for behavioral health when delivered by primary care providers? Mental health providers? Do procedural codes represent all services provided (including those not billed for)? Do diagnostic codes represent all diagnostic categories (including those not billed for)? Review and Modify Documentation Procedures Are diagnostic and procedure codes documented for in each progress note? Are codes for each encounter documented in both the SBHC medical record and mental health chart (if separate)? Are codes entered into database regardless of reimbursement? Understand State Program and Provider Coverage Issues Research State Program Information ● ● www.cms.gov (Medicare Regulations) Search by state by Department of Health or Department of Mental Health to find state specific information Contact State Medicaid Assistance Program and determine specific Behavioral Health Service requirements Invite Medicaid Representatives to your facility or visit them to present Behavioral Health Program and clearly understand the requirements Determine Reimbursement Estimates Obtain reimbursement rates by provider type for state and other programs Understand billing rules by payer, e.g. billing E&M visit same day as Behavioral Health visit, number of visits limits, auth/preauthorizations, etc. Assure you have a complete understanding of program parameters re: Individual Therapy, Case Management, Special Behavioral Health Services, etc. Common Pitfalls in Coding 106 ICD-9 CM (Clinical Modification) Coding Guidelines Order to list ICD-9 codes Coding Order is Important 1. 2. 3. Acute Reason patient is being seen needs to be listed first. Co-morbid diagnosis affecting treatment of principal diagnosis are listed next. List all other documented conditions coexisting at the time of the visit that require or affect patient care, treatment or management. Chronic diseases may be listed as often as they are treated 107 ICD-9-CM Coding Guidelines DO NOT CODE: ● Conditions previously treated that no longer exist. ● Conditions that do not affect treatment or management at the current visit. ● Rule-out, suspected, questionable or probable diagnoses. 108 ICD-9-CM Coding Guidelines Review of Systems Documentation Cannot say “all other negative” Must list pertinent and negative findings Must have a way to determine which systems were reviewed A check list is acceptable 109 About Time With the Patient Do not base your level of service on time spent with patient. Time only comes into play if you are billing for counseling within an acute visit or if all you are doing is counseling 110 Sports Physicals They are not meant to be comprehensive physicals – their focus is different Check www.aafp.org for an appropriate form You can bill for a complete PE and a sports PE within the same year 111 Acute Problems within a Comprehensive Physical When doing a preventive health visit (V20.2) and there is a separate health acute problem – you can list both the preventive health visit code (first) and the acute visit code (second) – BUT THERE MUST BE ICD-9 CODES THAT JUSTIFY BOTH (the billing department must add a modifier) 112 Be sure to know the Reason for the Visit Reason for Visit Preventive Visit Acute Visit Counseling Visit 113 Late Effects of Burns Late effects means the burn has healed. There should not be dressing changes. 114 Counseling Visits Counseling visits are when client comes in to discuss a problem only. No hands are laid on the patient. 115 Example Dietary Surveillance & Counseling There must be a dietary problem in order to justify this code. 116 Be Specific with the codes you use 117 784.1 Throat Pain EXCLUDES: ● Dysphagia 787.2 ● Neck pain 723.1 ● Sore throat 462 ● Chronic 472.1 118 AGAIN - About Over-coding and Under-coding CPT and ICD-9 codes must always relate The first ICD-9 code you use drives the relationship to the CPT code 119 Coding Compliance Audit 120 Poor example incorrect coding for documentation See Handouts of Completed Note Sample 10a (handout 9) & Encounter Form 10a (handout 10) 121 122 123 Analysis of incorrect coding for documentation 124 Coding Audit Cheat Sheet Top half of form PATIENT IDENTIFIER____10a CODING AUDIT CHEAT SHEET TYPE OF SERVICE PROVIDED: Preventive Health – New patient ______ Preventive Health – Established patient ______ Counseling Services– No Physical Complaint Is time recorded in chart? YES _____NO _____ Is a counseling code used? YES _____ NO _____ Evaluation / Management Visit: where counseling determines time Is the total time of the visit recorded YES _____NO _____ Is the time spent in counseling recorded YES _____ NO _____ Is a counseling code used? YES _____ NO _____ Evaluation / Management Visit – NEW PATIENT Evaluation / Management Visit – ESTABLISHED PATIENT CPT & ICD-9 CODES USED CPT CODES: 99203 ICDE-9 CODES: 625.3 DO THE CPT/ICD-9 CODES CORRELATE? YES __X___NO ______ 125 Coding Audit Cheat Sheet Bottom Half of Form HISTORY AND EXAMINATION New Established 99201 99211 99202 99212 99203 99213 99204 99214 99205 99215 HPI ROS PFSH 0 0 0 1 0 0 1 1 0 4 2 1 4 10 2 EXAM 0 1 4 5 8 CHART AUDIT LEVELS FOR E/M VISITS HPI, ROS, PFSH 3 EXAMINATION 2 2 NEW PATIENT LEVEL Lowest level supports level ESTABLISHED PT LEVEL ____ 2 of 3 or middle level supports level MEDICAL DECISION MAKING 3 126 Medical Decision Making Section I: Diagnosis or Management of Problems 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 One selflimited or minor problem Two or more selflimited or minor problems -One stable chronic condition -Acute uncomplicated illness One or more chronic illnesses with complications Two or more stable chronic conditions Undiagnosed new problem w/uncertain prognoses Acute illness with systemic symptoms Acute complicated injury One or more chronic illness with severe complications Acute or chronic illness or injury that is life or limb threatening Abrupt change in neurologic status 127 Medical Decision Making Section II: Diagnostic Procedures 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 Lab X-ray EKG UA Ultrasound, etc. Venipuncture KOH Physiologic tests not under stress Pulmonary Function Barium Enema Arterial puncture Skin biopsies Physiologic tests under stresscardiac stress tests Diagnostic endoscopies with no risk factors Deep needle or incisional biopsy Obtained fluid from body Cardiovascular imaging with contrast Cardiovascular imaging with contrast Invasive diagnostic tests Cardiac Electrophysiological tests Diagnostic endoscopies with identified risk factors Discography Other levels of Diagnostic procedures do not usually apply to SBHC, but you only128 need to have 2 of the 3 areas of medical decision making to agree. Medical Decision Making Section III: Treatment or Management Options 99201 99202 99203 99204 99205 99211 99212 99213 99214 99215 Rest Gargles Elastic bandages Dressings OTCs Minor surgery PT OT IVs without additives Minor surgery with risk factors Elective major surgery— no risk factors Prescription drug management IV fluids with additives Closed facture or dislocation treatment w/o manipulation Therapeutic nuclear medicine Elective Surgery with identified risk factors Emergency major surgery Parenteral controlled substances Drug treatment requiring intensive monitoring Decision not to resuscitate or deescalate care because of poor prognosis 129 Unfortunately – Because of this documentation/coding error - you will not get paid for this visit. This is why it is very important to verify that charting supports all levels of coding decision making. 130 Questions & Answers 131