VO 2 max - Belgian Working Group Heart Failure and Cardiac
advertisement

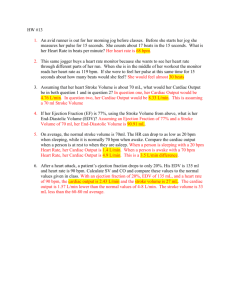
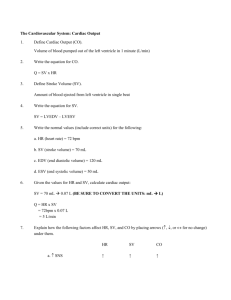
Working Group of Heart Failure and Cardiac Function Second Annual Symposium, Woluwe, 14th of October 2006 HEART FAILURE: WHAT CAN A PHYSIOLOGIST TELL THE CLINICIANS? Robert Naeije Erasme University Hospital, Brussels, Belgium What is heart failure We define heart failure as a state in which the heart is unable to meet the demands for blood flow without excessive use of the Frank-Starling mechanism, that is the increase in stroke volume associated with increased preload Sagawa, Maughan, Suga, Sunagawa. Cardiac Contraction and the Pressure-Volume Relationship. Oxford University Press, 1988 Definition of Heart Failure 1. 2. Excessive use of the Frank-Starling mechanism: dilated cardiomyopathy and congestion – adaptation vs maladaptation or decompensation Inability to meet peripheral demand: decreased aerobic exercise capacity – decreased VO2max (or maximum average running speed), because of a limitation in cardiac output O Frank 1865-1944 Isometric contractions of a frog ventricle at increasing filling pressures O. Frank, Z Biol 1895; 32:370 Ventricular PV curves during ejecting vs non-ejecting beats Isobaric end-systolic PV relationship positioned to the right of the isovolumic end-systolic PV curve indicating strong historydependence of the endsystolic PV curve – But in canine and human hearts, both curves are superposed Frank O. Die Grundform des arteriellen Pulses Z Biol 1899; 37:484-526 Frog ventricle Dog ventricle Squelettal muscle Isovolumic diastolic and systolic PV relationships Length-tension relationship applied to the intact ventricle Pressure Sequential P-V loops Contractility Emax Pes/Ves Afterload = PxV or: Pes/SV Decreased venous return Preload = EDV SV Volume EH Starling in his laboratory, at work on his heart-lung preparation - 1910 Patterson et al, J Physiol (London) 1914; 48:357 Stroke volume increases with end-diastolic volume Patterson et al, J Physiol (London) 1914; 48:357 An increase in preload increases stroke volume SV ~ EDV EF = SV / ED increased Stroke work increases with end-diastolic volume Patterson et al, J Physiol (London) 1914; 48:357 An increase in blood pressure decreases stroke volume (1) which is restored by a an adaptative increase in EDV (2) SV is initially decreased, then restored with adaptative EF to increased afterload A decrease in contractility decreases stroke volume 1: increased contractility 2: decreased contractility Starling ’s law of the heart Now here are two conditions in which the work of the heart is increased and in which this organ adapts itself by increasing the chemical changes in its muscle at each contraction to the increased demands made upon it. It is evident that there is one factor which is common to both cases, and that is the increased volume of the heart when it begins to contract. So we may make the following general statement. Within physiological limits, the larger the volume of the heart, the greater are the energy of its contraction and the amount of chemical change at each contraction. EH Starling. The Linacre lecture on the law of the heart. London: Longmans, Green, 1918 Heterometric vs homeometric autoregulation of the heart After 60 s of increased loading conditions, return to initial state is associated with decreased EDV and ESV, suggesting increased contractility Patterson et al, J Physiol (London) 1914; 48:357 Heterometric vs homeometric autoregulation of the heart Source: Rosenblueth et al. Arch Int Physiol 1959; 67: 358 Limitations to Starling’s law of the heart • Frank-Starling’s law of the heart states that ventricular stroke work increases as a function of end diastolic volume • This is valid for the rapid adaptation of flow output to changing loading conditions • Otherwise, the essence of ventricular adaptation to loading conditions is homeometric (systolic function, Anrep’s relationship) rather than heterometric (change in dimensions, Starling’s relationship) What is heart failure We define heart failure as a state in which the heart is unable to meet the demands for blood flow without excessive use of the Frank-Starling mechanism, that is the increase in stroke volume associated with increased preload Sagawa, Maughan, Suga, Sunagawa. Cardiac Contraction and the Pressure-Volume Relationship. Oxford University Press, 1988 Heart failure Type 1: increased loading Type 2: altered inotropic state Type 3 altered lusitropic state Sagawa, Maughan, Suga, Sunagawa. Cardiac Contraction and the Pressure-Volume Relationship. Oxford University Press, 1988 Definition of Heart Failure 1. 2. Excessive use of the Frank-Starling mechanism: dilated cardiomyopathy and congestion – adaptation vs maladaptation or decompensation Inability to meet peripheral demand: decreased aerobic exercise capacity – decreased VO2max (or maximum average running speed), because of a limitation in cardiac output VO2 = Q x (CaO2 – CvO2) • A VO2max is achieved on a bicycle with about half of body’s muscles • Minimum CvO2 is constant – cf HbO2 dissociation curve, and chronic disease (except sepsis?) does not affect O2 extraction • VO2max is determined by maximum O2 delivery, or cardiac output VO2max ~ Qmax x CaO2 Fleg et al, AHA advisory Circulation 2000;102:15917 Aerobic exercise capacity is determined by O2 delivery Q x CaO2 Source: Saltin and Strange, MSSE 1992; 24: 30-37 Linear increase in VO2 and Q as a function of workload Exercise testing: linear relationship between VO2 (or cardiac output) and running speed (workload) VO2max and the Cooper test (12 min run) Cooper et al, JAMA 1968; 203: 201-4 Six-min Walk Distance and CPET in heart failure Miyamoto et al, AJRCCM 2000; 161: 487-492 VO2/HR = SV Rationale for exercise testing to evaluate heart failure - Linear relationships between VO2, cardiac output and workload, or average running or walking speed - VO2max or 6MWD exclusively determined by maximum cardiac output, - or the ability of systolic function to cope with increased afterload - This is why the 6MWD is correlated to functional class, survival, and clinical state, and is sensitive to therapeutic interventions Fleg et al, AHA advisory Circulation 2000;102:15917 Conclusions • A sound definition of heart failure rests on the notion of changes in loading conditions and/or relative insufficiency of systolic/diastolic adaptation, as a cause of insufficient flow output (O2 delivery, Q x CaO2) to peripheral demand (VO2) • Associated changes in ventricular dimensions and diastolic function may be a cause of congestion • Heart failure is a continuum, with uncertain significance of clinical notions of compensation or decompensation