Screening of Pooled Platelets
advertisement

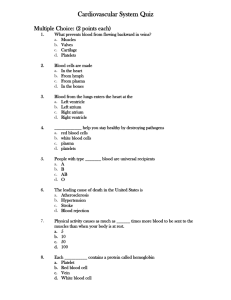
Bacterial Contamination and Screening of Platelet Concentrates James X. Gray, BSc(Hons), PhD, MD Haematology Registrar The Alfred Hospital Case from SHOT annual report 2004 A 75 year old female patient with chronic lymphatic leukaemia developed rigors, vomiting and pyrexia following transfusion of a 5-day old pooled platelet unit. The transfusion was terminated and the patient recovered. An identical strain of S.epidermidis was isolated from the transfused platelet pack and from the venepuncture site of one of the four contributing donors. However, the organism was not isolated from the recipient following the reaction. This is evidence of bacterial contamination of a platelet pool from a donor's arm and suggests arm cleansing was inadequate. Although transmission to the recipient was not confirmed it would seem likely. Differential Centrifugation and Separation Whole Blood + Preservative (450 ml +/- 45 ml) Specific Gravity RBC 1.08 – 1.09 Platelet 1.03 – 1.04 Plasma 1.023 Hard Spin Red Cells Buffy Coat Plasma Pooled x 4 Soft Spin Pelleted Red Cells Platelets Blood Product Testing Sydney Red Cross(TGA accreditation) Pathogen Screen test window / d Risk HIV 1+2 serology only 22 1 in 2.4 x 106 HIV serology + NAT 09 1 in 7.3 x 106 HCV serology only 66 1 in 330,000 HCV serology / NAT 07 1 in 3.7 x 106 HBV serology 45 HTLV I&II serology 51 <1 in 2.4 x 106 CMV serology Syphilis serology Malaria serology vCJD questionairre none reported Bacterial culture of Platelets (20%) Quality Control Specifications Platelet Concentrates: pooled x 4, leukodepleted TGA requirements (Council of Europe Guidelines): Parameter Volume Specification Acceptance 160-240 ml Sampling 75 % 1% Platelets (per unit) > 240 x 109 75 % 1% Leucocytes (per unit) pH < 0.8 x 106 90 % 1% 6.8 – 7.4 75% 1% Microbial contamination Negative 5% Bacterial Detection of Platelets: Current Problems and Possible Resolutions Morris A. Blajchman, Erik A.M. Beckers, Ebbe Dickmeiss, Lilly Lin, Gillian Moore and Ludo Muylle McMaster University and Canadian Blood Services, Hamilton, Ontario, Canada Sanquin Blood Bank South West Region, Rotterdam, The Netherlands Copenhagen Blood Transfusion Service Center, Rigshospitalet, Copenhagen, Denmark Cerus Corporation, Concord, CA Queen Elizabeth Hospital, King's Lynn, UK Red Cross-Flanders Blood Service, Mechelen, Belgium University of Antwerp, Antwerp, Belgium Transfusion Medicine Reviews Volume 19, Issue 4 October 2005, Pages 259-272 Limitation Of Routine Bacterial Screening of Platelets With the BacT/ALERT System: A 30-Month Experience From the Sanquin Blood Bank Southwest Region of the Netherlands EAM Beckers Sanquin Blood Bank Southwest Region, Rotterdam, Netherlands Beckers, (Holland) Transfusion Medicine Reviews, vol 19 (4) Donor questionnaire Disinfect venesection site Diversion pouch of 30 ml Pooled buffy coat units (5 donors) Leukoreduction filtration Automated culture Bact T/alert 100% screening Beckers, (Holland) Transfusion Medicine Reviews, vol 19 (4) Positive cultures 0.76% 172 units (58%) already issued 155 units already transfused Reported transfusion reactions – Nil Serious septicemia reported in 2 patients, who received culture negative platelets Bacterial Screening of Platelet Concentrates: A 4-Year Experience in Belgian Blood Centers L Muylle Red Cross-Flanders Blood Service, Mechelen, and University of Antwerp, Antwerp, Belgium Muylle, (Belgium) Transfusion Medicine Reviews, vol 19 (4) Arm disinfection Closed system for platelet preparation Pooled (5-6 patients) Apheresis platelets No diversion Automated culture - Bact T/alert 100% screening 108,000 platelet concentrates over 4 years Test Results of the Bacterial Screening of Platelet Units for 5 days using BacT/alert detection Number Tested Screening Positives False Positives Confirmed Positives Pooled (n = 5 or 6) buffy coat platelets 75 829 793 (1.05%) 140 (0.18%) 622 (0.82%) Single-donor apheresis platelets 31 998 237 (0.74%) 41 (0.13%) 181 (0.57%) Total 107 827 1030 (0.96%) 181 (0.17%) 803 (0.74%) Muylle, (Belgium) Transfusion Medicine Reviews, vol 19 (4) 803 units were positive 446 units already transfused 314 units confirmed positive on repeat culture 203 follow-up reports from clinicians 12 transfusion reactions - sepsis x 2 fever hypotension rigors rash x6 x1 x1 x2 Bacterial Screening of Buffy Coat–Derived Platelet Concentrates Findings From a Danish Blood Bank E Dickmeiss Copenhagen Blood Transfusion Service Center, Rigshospitalet, Copenhagen, Denmark Results of the Initial Routine Screening of Pooled Buffy Coat Platelet Concentrates in the Danish (Copenhagen) Study No. of buffy coat pooled (n = 4) platelet concentrates monitored 22 165 No. of positive on BacT/ALERT tests 50 No. of positive BacT/ALERT tests with sterile platelet concentrates 16 No. of positive BacT/ALERT tests with bacterial culture– positive platelet concentrates 34 (0.15%) Time elapsed between seeding of the BacT/ALERT flask and the appearance of a positive signal 22 h (median range, 10-60 h) No. with a positive culture in 1 of the corresponding RBC units 10 (0.05%) No. with all corresponding RBC units sterile 24 (0.11%) Bacteria found in the 34 confirmed positive routine cultures, 6 already transfused Coagulase-positive Staphylococcus species 28 cases Corynebacteria 4 cases B cereus 2 cases Results from the Copenhagen Study Day 3 Screening (All Units had Tested Negative Upon Initial Screening) No. of day 3 platelet concentrates screened 2472 No. of confirmed contaminated platelet concentrates 6 (0.24%) Time elapsed between seeding of the BacT/ALERT flask and the appearance of a positive signal 16 h (median range, 10-25 h) No. with positive culture in 1 of the corresponding RBC units 1 (0.04%) No. with all corresponding RBC units sterile 5 (0.20%) Bacteria found in the confirmed positive cultures Coagulase-negative Staphylococcus species 5 cases Corynebacteria species 1 case Discussion Points 1 Late appearance of positive signal, often after unit is issued and transfused, suggests that the degree of contamination or bacterial load is probably low and often w/o clinical consequence. Six culture-positive units had already been transfused w/o complication. BacT/Alert culture system relies upon detection of CO2. Sensitivity is highly dependent upon: i) Timing of platelet sampling (day 1 or day 3) ii) Sample volume. Discussion Points 2 Utility of 100% screening False positives result in unnecessary wastage, False negative results are generally unacceptable Blocking of platelet units with high bacterial loads Pathogen inactivation is proactive, can improve blood safety further and potentially permit a longer shelf-life Improving the bacteriological safety of platelet transfusions Morris A. Blajchman , Mindy Goldmanc and Federico Baezad a Departments of Pathology and Medicine, McMaster University, Hamilton, Ontario, Canada b Canadian Blood Services, Hamilton, Ontario, Canada c Canadian Blood Services, Ottawa, Canada d Baxter Transfusion Therapies Europe, Madrid, Spain Transfusion Medicine Reviews Volume 18, Issue 1 January 2004, Pages 11-24 Pre-transfusion Bacterial Detection Methods Transfusion Medicine Reviews January 2004 Visual inspection – swirling and colour Automated bacterial culture - detection of CO2 Pall BDS (O2 consumption) DNA/RNA Fluorescent antibody labeling Specific peptidoglycan components of cell wall Dielctrophoresis Endotoxin detection Microscopic detection Automated Bacterial Cultural Systems Detection of CO2 produced by the growing bacteria; eg. BacT/Alert. Culture medium is inoculated with a blood sample, incubated, continuous readings for CO2 production Smaller inoculums require longer incubation periods and are more likely to give false negative results. Larger inoculums waste precious resource. Threshold of detection: 10 CFU/ml Slow growing bacteria (eg. S. epidermidis) may need 6 to 7 days, Propionibacterium acnes even longer. Given the need for some incubation periods to be longer than the shelf life of the unit and the likelihood that the unit will already be transfused, underscores the need for a robust communication pathway and audit practice. Pall Corporation BDS (Bacterial Detection System) Measures the consumption of O2 by contaminating bacteria, in the absence of platelets or leukocytes. A 2 – 3 ml sample of platelet concentrate. In-line filtration to remove leukocytes and platelets, not the bacteria. Contained within a non-gas-permeable pouch and incubated. Positive reading when O2 concentration falls. Detection sensitivity 97% after 24 hrs, when bacterial inoculum 100-500 CFU/ml. Only a single reading per sample. Nucleic Acid based detection systems Detection of bacterial DNA or rRNA Highly conserved bacterial rRNA sequences, although several probes are required to cover all desired organisms. PCR based technology In reported literature ~104 CFU/ml (4-5 days of storage) Threshold of bacterial load desired 102 CFU/ml Detection systems based on changes in metabolic parameters during storage. Abnormal glucose concentrations Low pH Significant variations of normal High levels of bacterial contamination are needed for reliable reproducibility. Fluorescent Antibiotic Labeling Antibiotics labeled with fluorescent markers Binding specificities for bacterial molecular components. Several may be required. Detection by Flow Cytometry Threshold ~105 CFU/ml Detection of specific peptidoglycan components of bacterial cell walls Bacterial load required ~103 – 104 CFU/ml Dielectrophoretic Method Bacteria move in an electric field and platelets don’t Bacterial load required ~105 CFU/ml Microscopic examination of stained samples Bacterial load required ~106 CFU/ml Endotoxin detection Pathogen Inactivation 1 The only approach to achieve absolute bacteriological safety. L-Carnitine in platelet storage medium, results in a modest inhibition of coag. Neg. Staph. Gamma Irradiation GVHD is prevented at doses of 25 – 30 Gy Bacteria are inactivated at 100 – 150 Gy Platelet function is compromised at doses above 75 Gy. Riboflavin plus UVA Demonstrated utility in in vitro assays against strains of Staph. epidermidis, S. aureus, Pseudomonas, Klebsiella, E. coli. No clinical trials to date. Amotosalen HCL plus UVA light Synthetic psoralen intercalates with DNA helices and covalent bonds form in presence of UVA Demonstrated utility, in RCCT, with bacteria, viruses and malarial parasites. INTERCEPT Blood System, Cerus Corp, USA Reducing Risk of Platelet Contamination 1 Improve donor screening Donor questionnaire for subclinical bacteremia Improve venepuncture site disinfection Antiseptic - quality - quantity - mode of application Diversion Pouch – 13.5 ml to 30 ml 40%, 72%, 90% Reducing Risk of Platelet Contamination 2 Platelet storage most TA septic events occur with units > 3d early use while bacterial load is sub-clinical. Universal Leukoreduction (also removes bacteria) Apheresis derived platelets 8 std units from a single procedure Reducing transfusion triggers Clinical Practice Guidelines Optimizing Transfusion Indications Audits of blood component usage Audits by Transfusion Committees Audits of blood component use have indicated that blood products, both cellular and plasma, are often inappropriately used.