Erin Hurley-Presentation on Health Care Matrix
advertisement

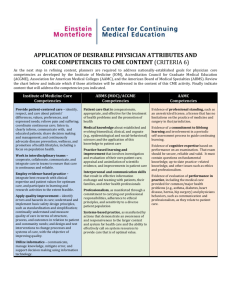
THE HEATLHCARE MATRIX Erin Hurley, PGY 4 June 16, 2020 “Every hospital should follow every patient it treats long enough to determine whether the treatment has been successful, and then to inquire ‘If not—why not?’ with a view to preventing similar failures in the future.” Ernest Codman M.D. , 1914 PATIENT SAFETY Anesthesia coined the term “patient safety” Institute of Medicine (IOM) of the US Academy of Sciences 1999: “To Err is Human” 2001: “Crossing the Quality Chasm” QUALITY CHASM “Health care we have and the care we could have– represents more than a gap, but rather a chasm” Medical education chasm IOM Care of every patient has the potential to improve the care of all patients yet to come Competencies are integrated into the routine practices of daily care Decision making regarding care of the patient is guided by the best evidence available The quality of health care is positively related to the quality of medical education IOM– AIMS FOR IMPROVEMENT Safe Timely Effective Efficient Equitable Patient Centered ACGME The content of graduate education is aligned with the changing needs of health systems Residency programs use sound outcome assessment methods for both residents’ and programs’ achievement of educational outcomes. ACGME COMPETENCIES “Quality of health care is positively related to quality education” CORE COMPETENCIES Patient Care Medical Knowledge Interpersonal and communication skills Professionalism Systems-based practice Practiced-based learning and improvement CORE COMPETENCIES Teaching No prescribed formulas Assessment Interpersonal and communication skills System-based practice Practice based learning and improvement HEALTHCARE MATRIX A formative approach to the presentation of core competencies to residents, which in turn is having an effect on the faculty and their patient care A response to the challenge of linking all six competencies with the realities of the current medical education system– which is focused on acquisition of medical knowledge Healthcare Matrix: Care of Patient (s) with… AIMS Safe Timely Effective Competencies Patient Care Medical Knowledge Interpersonal/ Comm. Skills Professionalism Systems Based Practice IMPROVEMENT Practice-Based Learning /Improvement The Healthcare Matrix, 2004, John Bingham & Doris Quinn, Vanderbilt University Efficient Equitable PatientCentered PATIENT CARE SHOULD BE: Safe: Avoiding injuries to patients from care intended to help them Timely: Reducing waits and sometimes harmful delays for those who receive and give care Effective: Providing services based on scientific knowledge to all who could benefit; refraining from providing services to those likely not to benefit Efficient: Avoiding waste of equipment, supplies, ideas, energy Equitable: Providing care that does not vary in quality because of personal characteristics Patient-Centered: Providing care that is respectful of and responsive to individual patient preferences, needs, values; ensuring that patient values guide all clinical decisions MEDICAL KNOWLEDGE: WHAT MUST WE KNOW? Patient care Safe Timely Effective Efficient Equitable Patient Centered Medical Knowledge “…about established and evolving biomedical, clinical, and cognate sciences, and application of this knowledge to patient care.” INTERPERSONAL/COMMUNICATION SKILLS: WHAT MUST WE SAY? Patient care Safe Timely Effective Efficient Equitable Patient Centered MK Interpersonal & Communication Skills “…that will result in effective information exchange and teaming with patients, their families, & other health professionals.” PROFESSIONALISM: HOW MUST WE BEHAVE? Patient care Safe Timely Effective Efficient Equitable Patient Centered MK ICS Professionalism “…as manifested through commitment to carrying out professional responsibilities, adherence to ethical principles, & sensitivity to diverse patient population.” SYSTEMS-BASED PRACTICE: WHAT IS THE PROCESS? ON WHOM DO WE DEPEND? WHO DEPENDS ON US? Patient care Safe Timely Effective Efficient Equitable Patient Centered MK ICS Prof SystemsBased Practice “…as manifested by actions that demonstrate an awareness of, and responsiveness to, a larger context & system of healthcare and ability to effectively call on system resources to provide care of optimal value.” PRACTICE-BASED LEARNING & IMPROVEMENT: WHAT HAVE WE LEARNED? WHAT WILL WE IMPROVE? Patient care Safe Timely Effective Efficient Equitable Patient Centered MK ICS Prof SBP Practice-Based Learning & Improvement “…involves investigation & evaluation of residents’ (program’s, or institution’s) own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care.” VALUE OF THE MATRIX Healthcare Matrix: Improving Care by Linking Outcomes to Competencies Over 100 matrix presentations at Vanderbilt Guide learners in analyzing the care of their own patients by using Core competencies to identify opportunities for improvement Change the environment of case presentations and MM conferences from one of blame to one of system analysis and quality improvement EFFECTIVENESS Provides a learning format that is part of daily education and delivery of care by residents Addresses the multidisciplinary culture in which residents practice Being used by many health professions besides residents Provides a solution that is standardized so that multiple programs and institutions can have a common framework to teach the competencies and learn from each other EDUCATIONAL ENVIRONMENT The matrix allows transformation of the educational environment Team learning Patient care– structures and systems Collaborative decision-making Collective analysis and improvement Connections/trends between cases MATRIX AT VANDERBILT 100 matrices were analyzed to look at safety concerns across institutions Four major themes identified Communication Teamwork “workarounds” (circumventions of a system) Inadequate or poor documentation CEDARS-SINAI MEDICAL CENTER Using the healthcare matrix to teach and improve patient safety culture in an OB/GYN residency training program Utility of healthcare matrix in teaching about safety and improvement of care METHODS HCMC is held at least once monthly in our residency education program The selected resident chooses the case & develops a draft matrix under faculty supervision A multidisciplinary team is invited based on the case The matrix is presented at conference and a consensus action plan for implementation is generated after discussion METHODS Two years after the initiation of the program, the residents completed an anonymous 15-item survey about their perception of the program using a 5 point Likert scale RESULTS 26 HCMC were held from 2007 to 2009 PGY-4 residents prepared & conducted 77% sessions Case Distribution (n=26) Management concerns Medication errors/concerns Bleeding complications Clinical distribution 42.3% 23.1% 34.6% Gynecology cases 46.2% Obstetrical cases 53.8% SUB-OPTIMAL CARE BY IOM AIMS 100% 96% 80% 65% 60% 50% 46% 40% 19% 20% 23% 0% Safe Timely Effective Efficient Equitable Patient Centered SUB-OPTIMAL CARE BY ACGME COMPETENCIES System-based Practice 77% Professionalism 46% PBL & Improvement 100% Patient Care 96% Medical Know ledge & Skills 69% Interpersonal & Communication Skills 65% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Residents perception of the utility of the Healthcare Matrix Figure 1: *Residents perception of the utility of the Healthcare Matrix (n=21) Should be interdisciplinary 100% Effective for teaching ACGME competencies & IOM Aims 81.00% Would use in my clinical practice in future 57.10% 47.60% Preparation is time consuming Great, continue to use Should be canceled 95.20% 0% Improved ability debrief 90.50% Improved my communication skills 38.10% Useful for quality improvement 95.20% Helped analyze a complex situation 100% Changed my practice Felt awkward presenting errors of my superiors Review errors in blame free environment Helped assess errors Fosters learning 0.00% 85.70% 28.60% 71.40% 95.20% 90.50% 10.00% 20.00% 30.00% 40.00% 50.00% 60.00% 70.00% 80.00% 90.00% 100.00% RESULTS- RESIDENTS’ SURVEY Effective, fosters learning, and should be continued Improved their ability to debrief, was useful for quality improvement, helped analyze a complex situation, changed their practice, and helped assess errors Some felt awkward presenting medical errors made by their superiors, but the majority felt that the HCMC provided them with a blame free environment to discuss errors CONCLUSION Residents can use the healthcare matrix in a multidisciplinary setting to evaluate and improve patient care. HCMC allows the IOM Aims to become a framework for reviewing patient safety culture. Allows residents to integrate the ACGME Competencies as part of their routine clinical practice. CONCLUSION Timeliness, medical knowledge, & communication issues were major contributors to patient safety concerns. Residents’ survey highlights areas that need more attention. Healthcare matrix provides a foundation for systematic transformation in patient care, medical education, and team dynamics that could be useful for residency training programs. MATRIX 2007 Healthcare Matrix: Care of Patient with uterine atony after D+E with DIC AIMS Competencies SAFE TIMELY EFFECTIVE EFFICIENT (Avoiding injury from care intended to help) (Reducing delays for pts and providers) (Evidence-based medicine, avoiding underuse and overuse) (Avoiding waste of equipment, supplies, ideas, and energy) EQUITABLE PATIENT-CENTERED (Care does not vary based on race, (Care with respect for ethnicity, gender, SES) preference, needs, values) Assessment of Care No - patient nearly died from hemorrhagic shock No - Life saving treatment was No – intrauterine ballon, delayed at several levels uterotonics and fluid resuscitation ineffective. Yes No – resources such a blood products, mobilization of staff not utilized in efficient manner. PATIENT CARE (Overall Assessment) Yes/No Ensure oxygen delivery, support BP, aggressive IV MEDICAL rescuscitation, treat cause KNOWLEDGE and SKILLS (What must we know?) Debriefing of all teams INTERPERSONAL involved even if ICU is closed AND COMMUNICATION SKILLS (What must we say?) Do no harm PROFESSIONALISM (How must we behave?) System should ensure that SYSTEM-BASED appropriate consultants notified such as anaethestiologist for PRACTICE (What is the process? intubation, On whom do we depend? Who depends on us?) Yes – Patient and family informed at all times. Patient desired to avoid hysterectomy at all costs. Prompt diagnosis, recognize urgency, initiate therapy, timely transport to OR. Urgency to treat delayed. Treatment of uterine atony – Aggressive IV resuscitation, uterotonics, intrauterine ballon repletion of blood products, correction of DIC used. Delayed decision to hysterectomy. N/A N/A Blood results – stat should be available sooner than 3 hrs. Crossmatched blood should be available sooner. More effective communication Private MD patient involve faculty MD between team members. Better communication better ICU and gyn residents. N/A Good communication with patient and family for intended intervention. Professional duty to Mobilize team members to accompany critically ill patient collect blood products. to the OR, to ensure safety and to expedite therapy. N/A Preserve patient autonomy D+E should be done in a Crossmatch in life-threatening tertiary facility so that blood can situations should be a priority. be mobilized as soon as possible. Availability of lab medicine, physician, timely transport of blood, expertise of gyn, anesthesiology should not vary from time of day/night SUMMARY--CREATING AND REINFORCING A CULTURE OF LEARNING The matrix is intended to help consider patient care in terms of the IOM Aims and the ACGME Core Competencies Enhance learning for every resident Team learning/ team dynamics Collaborative decision Resident– part of a system of care Common framework for evaluating and improving patient care across disciplines Integrate the ACGME Competencies as part of their routine clinical practice Improve quality of care THANK YOU The End Erin Hurley, PGY 4 June 16, 2020 REFERENCES Institute of Medicine: Crossing the Quality Chasm. Washington D.C.: National Academy Press, 2001 Using a Healthcare Matrix to Assess Patient Care in Terms of Aims of Improvement and Core Competencies. Journal on Quality and Patient Safety, February 2005 Quinn D , The Healthcare Matrix: Improving Care by Linking Outcomes to Competencies. MedEdPORTAL; 2007. Using the Healthcare Matrix to teach and improve patient safety culture in an OB/GYN residency training program Steven Rad, Connie Chung, Jessica Y. Hsu, Carolyn Alexander, and Dotun Ogunyemi. APGO 2010 Shine, K.: Crossing the quality chasm: The role of postgraduate training Am J Med113: 265–267, Aug. 15, 2002