Module 5: Assessment Skills

Module 5: Assessment Skills
Objectives
• Develop a rationale for assessment
• Be able to describe the attitudes and values for assessment of dual diagnosis
• Be able to identify key skills for dual diagnosis assessment
• Be aware of confidentiality issues within your workplace regarding discussion of substance use and other illicit behaviours
Dual Diagnosis Capabilities
• Recognise Needs (Integrated Assessment): In partnership with the service user, perform a triage assessment of mental and physical health, substance use, and social functioning and offending; identifying both needs and strengths. As a result of this assessment, the worker should be able to identify where those needs are best met by local services (Dual Diagnosis
Capability 9; level 2)
• Non-Judgemental Attitude: Be aware of ones own attitudes and values in relation to dual diagnosis and be able to suspend judgement when working with service users, and carers. Challenge others’ attitudes in an appropriate and useful manner. Dual Diagnosis Capability 4 level 2
• Engagement: Be able to develop an effective therapeutic relationship and be able to work flexibly with this client group. Dual Diagnosis Capability 6 level 2
• Ethical, Legal and Confidentiality issues: to be aware of and adhere to the organisation policy on confidentiality and to be able to effectively communicate this to the service user. To be able to seek advice about a potential breach of confidentiality, or legal issue. To be able to manage ethical and moral dilemmas that arise out of working with people with dual diagnosis. Be aware of confidentiality limits and be able to resolve potential breaches of confidentiality in consultation with the service user, their carers and other professionals .
(Dual Diagnosis Capability 11 level 1 and 2)
Exercise 1:
Take 10 minutes to consider the following:
• What is the purpose of assessment?
• We all assess as a part of our roles, but what do we do with all the information?
• How does this process involve the service user?
• What do they gain from participating in the assessment process?
Purpose of Assessment
• To gather baseline information about the types of difficulties that a person is experiencing (i.e. what is the problem?).
• the impact of those difficulties on their life.
• an understanding of how they developed.
• What factors maintain the difficulties, and what factors moderate them.
• Motivation to change, or intention.
• Future goals and roadblocks to achieving those goals.
• Assessment of strengths and changes already achieved
Assessment
Levels:-
• Brief 10 minutes informal chat
• Semi-structured interviewing/ questioning
• Use of structured exercises
• Use of validated tools
• Physical tests:- liver enzymes, urine and blood tox. Screens
• Corroborative information- past notes, family, other professionals
Maximum detection times for drugs in urine
• Amphetamine2-3 days
• Ecstasy30-48 hours
• Cannabis:
– Single use- 3 days
– Moderate use- 4 days
– Heavy use- 10 days
– Chronic heavy use- 36 days
• Methamphetamine-
48 hours
• Cocaine6-8 hours
• Methadone7-9 days
• Codeine24 hours
• Heroin1-2 days
Essential Skills
• Attitudes and values
• Collaboration/ working in partnership with service users and carers
• Structuring session and use of agenda
• Open and closed questioning
• Reflection and summarising
• How not to:
• Worker: “Right John, we’ve got to do this timeline thing so we better make a start as I am really busy today”
• Service user: “ok, but I have something to tell you...”
• Worker: “well, that’ll have to wait; we have to do this, as I’m pushed for time”
• Worker: “So, the first drug you used was cannabis, right?”
• Service user: “yeh”
• Worker: “Did you like it?”
• Service user: “yeh it was good”
• Worker “Were you at school when you used it?”
• Service user “yeh”
Exercise 2:
Using the “How not to” example, spend 10 minutes (preferably in pairs)
• Generating some open-ended questions that could have been asked to elicit more information form the person
• What else was wrong with the start of the session? How could it be improved?
Exercise 3:
Practising reflection. In Pairs (10 minutes)
• Each person takes turns to talk for 5 minutes about their favourite TV show.
• The other person listens and reflects back what the person is saying.
• At the end of 5 minutes the listener summarising the main points of the conversation.
• Write down each summary
• Discuss how accurate that summary is.
Exercise 4:
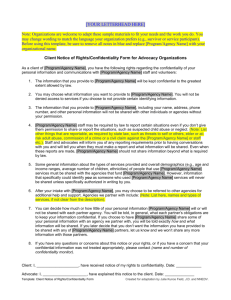
Confidentiality:Take 10 minutes to consider:
• What are the boundaries of confidentiality within your role around the disclosure of substance use?
• At what point would you breach confidentiality, and how would this be communicated to the service user?
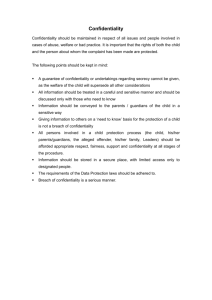
Confidentiality
• Doesn’t mean secret!
• Be up front about who gets access to information and why.
• Illegal activities may have to be reported to the police
(dealing drugs, threats of violence, serious crimes)
• Child protection issues will need to be reported.
• Respect peoples’ right to privacy within limits.
• Carers want and need information, and this should be shared only with full consent of the service user unless there are safety/legal issues.
• Carers may have important information for the care of the person
• Balance needs of individual against safety of others
• Fully explain why confidentiality may be breached.
• May have to re-engage person at a later stage.