Nordehn_Diabetes_Clinial_2.8.10
advertisement
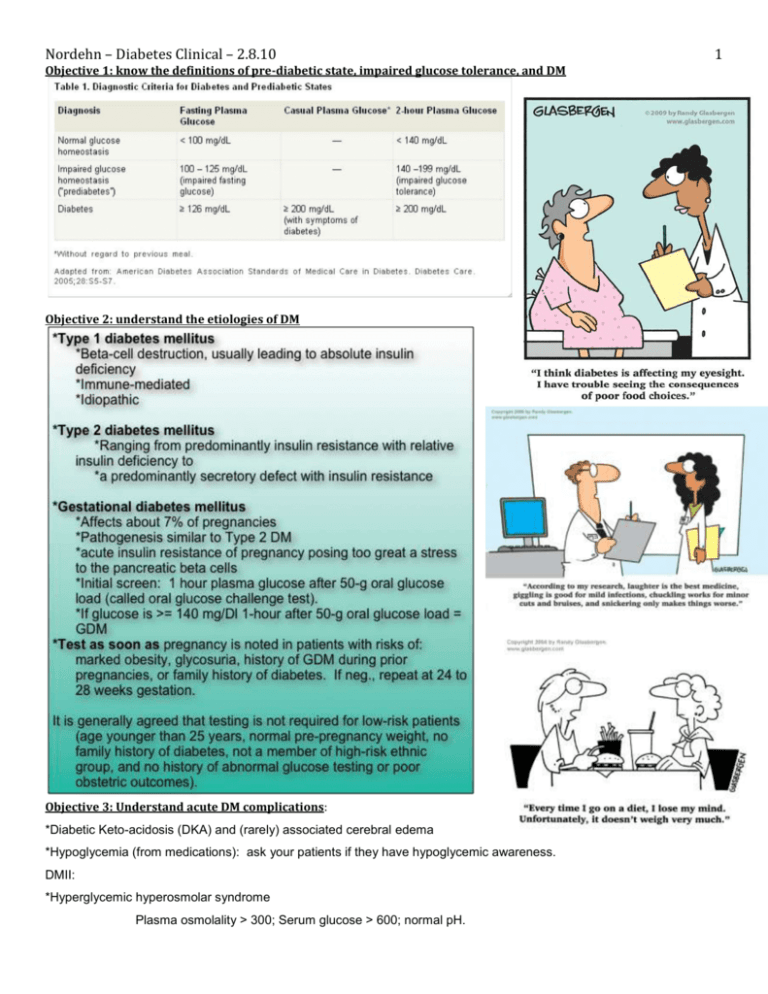
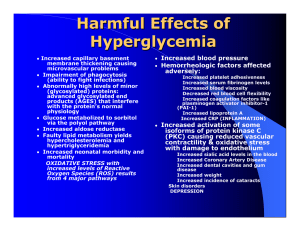
Nordehn – Diabetes Clinical – 2.8.10 Objective 1: know the definitions of pre-diabetic state, impaired glucose tolerance, and DM Objective 2: understand the etiologies of DM Objective 3: Understand acute DM complications: *Diabetic Keto-acidosis (DKA) and (rarely) associated cerebral edema *Hypoglycemia (from medications): ask your patients if they have hypoglycemic awareness. DMII: *Hyperglycemic hyperosmolar syndrome Plasma osmolality > 300; Serum glucose > 600; normal pH. 1 2 Nordehn – Diabetes Clinical – 2.8.10 Often associated with precipitating events: MI, infection, new renal insufficiency. *Hypoglycemia (from medications). Symptoms of hypoglycemia: Personality change, Cognitive impairment, Loss of consciousness, Seizure, Coma Irreversible brain injury Objective 4: understand the complications of chronic DM. Microvascular disease *Diabetic nephropathy: *Period of glomerular hyperfiltration and intraglomerular hypertension. *DM is the most common cause of renal failure world wide. peripheral nerve (Less common) *Autonomic neuropathy: *Orthostatic hypotension, *erectile dysfunction, *gastroparesis, *diabetic diarrhea, *Abnormal albumen excretion is an early sign. *atonic bladder. *Aggressive hypertension control, ACE inhibitor *Cardiac: therapy, and glucose control can slow progression. *Diabetic retinopathy: *DM is the cause of most legal blindness in US. *Background diabetic retinopathy *Hard exudates, microaneurisms, minor hemorrhages *Proliferative retinopathy *Neovascularization *Significant retinal hemorrhages *loss of physiological cardiac response to physiological stimuli (valsalva, standing, deep breathing) *Macrovascular disease, involving: *Coronary, carotids, *cerebral, *aorta, *arteries to the legs *Leads to: MI DM is associated with 2 to 4 fold increase in risk of *Macular edema MI (associated with hyperlipidemia and *Cotton wool spots - indicate retinal infarcts hypertension; controlling glucose does not help) *Keep: BP < 130/80; LDL < 100. *OTHER COMPLICATIONS: Impaired wound healing Increased post operative infection Sleep apnea (related to obesity) Venous thrombosis Osteoporosis Dementia Depression Peripheral neuropathy: *Stocking glove distribution *Paresthesias or painful dysthesia *Mononeuropathies: radiculopathy, cranial nerve Cancers: colorectal carcinoma, endometrial carcinoma Cause unknown; mitogenic effects of insulin in hyperinsulinemic pt is suspected. Nordehn – Diabetes Clinical – 2.8.10 Objective 5: Understand quality improvement markers of DM (just for context, no asterisk on this objective) His Summary: Questions: 1. Define pre-diabetic state 2. Define Impaired glucose tolerance 3. Define Diabetes Mellitus 4. A patient with Diabetes Mellitus is defined as having a fasting plasma glucose greater than what? 100 mg/Dl 125 mg/Dl 140 mg/Dl 5. Diabetes Mellitus is defined as a casual plasma glucose > 199 if accompanied by what symptoms? 6. Type 1 DM is caused by destruction of what type of cells? 7. Type 1 DM is which of the following? A secretory defect with insulin resistance. A disease with a pathogenesis similar to type gestational DM. Always associated with obesity. Immune-mediated 8. Type 2 DM etiology: 3 Nordehn – Diabetes Clinical – 2.8.10 9. Gestational DM affects what percent of pregnancies? 10. The pathogensis of Genstational DM is similary to: Type I DM Type II DM Varies between Type I and Type II DM 11. Describe the initial screen you should administer to assess for gestational DM 12. Gestational DM is defined as a glucose greater than [fill in the blank] after a 50-g oral glucose load? 13. When should a woman be tested for GDM? 14. Should all pregnancy women be tested for gestational DM? If not, who should not be tested? 15. Complications of DM I include? 16. The frequency of cerebral edema as a complication of DKA is: 17. What most often causes hypoglycemia in patients with DM I? 18. A hyperglycemic hyperosmolar syndrome is associated with a plamsa osmolality of more than________? 19. In hyperglycemic hypersomolar syndrome, the pH is _____? 20. list the Sx of hypoglycemia. 21. What is the most common cause of renal failure world wide? 22. Agressive control of blood pressure and use of what type of antihypertensive therapy can slow progression of DM complications? 23. Hard exudates and microaneurisms are considered: Background diabetic retinopathy Proliferative retinopathy Both background and proliferative retinopathy 24. Neovascularization, macular edema, and cotton wool spots are considered (use #23 options) 25. What is the distribution (anatomically) of diabetic peripheral neuropathy? 26. list 4 autonomic neuropathies associated with DM. 27. DM is associated with a how many fold increase in risk of MI? 28. In patients with DM, BP should be kept at less than: Answers: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. fasting 110-125 mg/dl glucose of 140-199 mg/dL 2 hours after 75-g oral glucose load fasting glucose >126 mg/dL or 2 hour glucose >200 mg/dL 125 mg/Dl polyuria, polydispia and blurred vision beta cells Immune-mediated Ranges from predominantly insulin resistance with relative insulin deficiency to a predominantly secretory defect with insulin resistance. 7% Type II DM 50-g oral glucose challenge test 140 Right away if family hx of diabetes, obese, history of GDM during past pregnancy, or glycosuria. Retest at 24-28 weeks. No. Mothers should be tested if they have prior GDM Hx, Family Hx, are obese, have glycosuria. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. Diabetic Keto-acidosis (DKA) and (rarely) associated cerebral edema Hypoglycemia Rare Medications 300 normal Personality change, Cognitive impairment, Loss of consciousness, Seizure, Coma, Irreversible brain injury DM ACEi Background DR Proliferative DR Stocking glove 26. Orthostatic hypotension, *erectile dysfunction,*gastroparesis*diabetic diarrhea, *atonic bladder *Cardiac: 27. 2-4 fold inc 28. 130/80 4