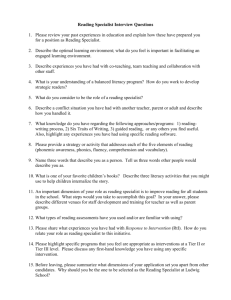
Specialist PSI Exercise Module
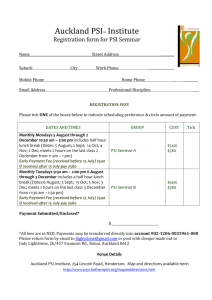
advertisement

EXERCISE FOR THE PREVENTION OF FALLS AND INJURIES IN FRAILER OLDER PEOPLE ‘PSI’ INSTRUCTOR COURSE A SPECIALIST NATIONAL TRAINING INITIATIVE Specialist PSI Exercise Module WHY? • Need for training to: – Support national accident prevention targets – Ensure greater consistency of provision – Ensure best practice • Need for training that is: – Specialist – Evidence-based – Practical – Interdisciplinary – Recognised Specialist PSI Exercise Module WHO? • Department of Health • Merton, Sutton & Wandsworth Health Authority • Advisory Group of National Experts • 1999 first pilot run • To date over 2000 PSI instructors have qualified Specialist PSI Exercise Module Interested Co-workers Specialist PSI Exercise Module WHAT? • First Recognised National Qualification • Postural Stability Instructors (PSIs) • Register of Exercise Professionals (REPS) at Level 4 – CPD at Level 3 • Chartered Society of Physiotherapy (CSP) Endorsed training • Accredited by Queen Margaret University (QMU) • Guidelines and Consensus Recommendations Specialist PSI Exercise Module HOW? • • • • • Underpinning Knowledge Application to Practice Practical Case Study Continuing Professional Development Specialist PSI Exercise Module AN INTERPROFESSIONAL NETWORK • Multifactorial Nature of Falls • Multiprofessional Skills • District Nurse • Family/Carers • General Practitioner • Health Visitor • Chiropodist •A & E • Hospital Doctors • Hospital Therapists • Ambulance Services • Social Services • Community therapy services • Pharmacist • Leisure Services • Professional Liaison • Respecting Boundaries/Building Trust • Patient Centred Specialist PSI Exercise Module ACCIDENT & EMERGENCY AMBULANCE SERVICES PRIMARY CARE GP ROUTES INTO THE FALLS SECONDARY CARE VERY SHELTERED/ RESIDENTIAL HOME/ NURSING HOME EXERCISE PATHWAY SELF REFERRAL SOCIAL SERVICES PRE-EXERCISE ASSESSMENT REHABILITATION EXERCISE PSI CHAIR BASED EXERCISE Specialist PSI Exercise Module THE THREE EXERCISE GROUPS REFERRAL FALLS REHABILITATION GROUP PSI CHAIR BASED EXERCISE GROUP Exercise for the Older Person Sessions Specialist PSI Exercise Module THE EXERCISE REGISTER UK High Risk Specialist Exercise Instructor Clinical Exercise MSc Patient Specialist Exercise Instructor Postural Stability NVQ4 Physically frail housebound/outpatient Independent with assistance/aids/carer Populations Medium Risk Independent with assistance/aids Advanced Exercise Instructor Exercise Referral NVQ4 Advanced Exercise Instructor Exercise for the Older Person NVQ3 Independently mobile older people Special Populations Low Risk OTAGO Exercise Leader Chair-based Exercise Leader NVQ2/3 General Populations Dinan, 1999 Exercise Instructor NVQ2 Specialist PSI Exercise Module While I have been talking….. • 4 older people will have been seriously injured... • 6 older people will have had a minor injury.. …..as a result of a fall at home Specialist PSI Exercise Module While we are here today... • 900 older people will have had a minor injury.. • 122 older people will have been seriously injured.. • 33 older people will never return home… ….as a result of a fall at home Specialist PSI Exercise Module FaME into practice A Four Point Plan to: Improve Balance and co-ordination Increase Functional Capacity Increase Bone and Muscle Mass Increase Confidence (reduce fear of falling) Includes: 7 Evidence Based Activities Specialist PSI Exercise Module 1. Dynamic endurance training for balance Specialist PSI Exercise Module 2. Dynamic balance training Specialist PSI Exercise Module Specialist PSI Exercise Module 3. Targeted resistance training (weights, bands and body weight) including targeted bone loading for leg and ankle strength for arm and back open & closed chain Specialist PSI Exercise Module 4. Backward chaining Specialist PSI Exercise Module 5. Functional floor activities Specialist PSI Exercise Module 6. Flexibility training for leg and ankle, chest, spine Specialist PSI Exercise Module 7. Sustained, three dimensional adapted Tai Chi training Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Prevalence and Consequences of Falls - Injurious falls - Non-injurious falls - Location of falls - Direct and Indirect costs - Fear of falling - Long Lies Specialist PSI Exercise Module 1 person dies every five hours as a result of a fall in the UK • One in three people aged > 65 years fall each year • One in two people aged >80 years falls each year • After the first fall, there is a 60 per cent chance of falling again • No two fallers are the same! • 75-80% of falls are not reported to a health professional Specialist PSI Exercise Module What is a fall? • “an unexpected event in which the participant comes to rest on the ground, floor, or lower level’” (ProFaNE, 2005) • With a layman’s definition of: – ‘. . . have you had any fall including a slip or trip in which you lost your balance and landed on the floor or ground or lower level?’ Includes: tumbling down the stairs, falling up stairs, falling onto a chair, the bed or the floor, sliding out of bed, slipping in the bath Does not include: tripping and correcting yourself, banging into the wall, being knocked or pushed over Specialist PSI Exercise Module Saving Lives - Our Healthier Nation • National Priority: – To reduce the rate of accidents - defined as those requiring a visit to a hospital or consultation with a doctor - by at least a fifth by 2010, from a baseline at 1996. Specialist PSI Exercise Module National Service Framework for Older People 2001 Standard 6: Falls. • To reduce the number of falls which result in serious injury and ensure effective treatment and rehabilitation for those who have fallen Key Interventions: • Prevention – including prevention and treatment of osteoporosis • Improving the diagnosis, care and treatment of those who have fallen • Rehabilitation and long-term support Individualise prevention: • …identifying those most at risk • …balance, gait and mobility problems Specialist PSI Exercise Module NICE CG21 Falls (2004) • • • • Case/risk identifications Multi-factorial falls risk assessment Multi-factorial interventions Education and information for patients and carers • Healthcare staff training Specialist PSI Exercise Module Why? DoH Prevention Package 2009 • Every five hours in England, an older person dies as a result of a fall. • For a primary care trust with a population of around 300,000 this means: – 15,500 older people will fall each year – 2,200 of those will attend A & E or minor injuries clinic, and a similar number will call an ambulance – 1,100 will sustain a fracture • 300 of which will be of the hip Specialist PSI Exercise Module Dept of Health Prevention Package (2009) Hip fracture patients Non-hip fragility fracture patients Individuals at high risk of 1st fragility fracture or other injurious falls Older people Objective 1: Improve outcomes and improve efficiency of care after hip fractures – by following the 6 “Blue Book” standards Objective 2: Respond to the first fracture, prevent the second – through Fracture Liaison Services in acute and primary care Objective 3: Early intervention to restore independence – through falls care pathway linking acute and urgent care services to secondary falls prevention Objective 4: Prevent frailty, preserve bone health, reduce accidents – through preserving physical activity, healthy lifestyles and reducing environmental hazards Specialist PSI Exercise Module Competing priorities? Issues Strokes & TIAs Heart Attacks Fragility Fractures Incidence/ year 110,000 275,000 310,000 Current trend Falling Falling Rising NHS bed days £1.8 m £1.15 m £1.57 m Annual costs £2.8 bn £1.7 bn £1.8 bn Specialist PSI Exercise Module Falls in women over 1 year 25 20 15 % 1 fall 2 falls 3+ falls 10 5 0 65-74 75-85 Age group 85+ Lord 1993 Specialist PSI Exercise Module Age-specific mortality rates-accidents among older people Source: OPCS Rates per million 1600 65-74 1200 75-84 800 85+ 400 0 Men Women FALLS Men Women TRAFFIC Men Women FIRE AND FLAMES Men Women OTHER Specialist PSI Exercise Module Deaths from home accidents in older people Source: Home accident surveillance system, UK, 1987 % deaths from accidents 80 70 65-74 60 75+ 50 40 30 20 10 0 Fracture Concussion Poisoning/ suspected poisoning Foreign Body Burn/ scald Other Specialist PSI Exercise Module Falls Rates per million 1600 1400 1200 Falls Men 1000 800 Falls Women 600 400 200 0 65-74 75-84 85+ Age (years) Specialist PSI Exercise Module How common are falls? • In those aged over 75, falls are the leading cause of death resulting from injury • A third of >65s and a half of >80s fall at least once a year • 10% of all call-outs for London Ambulance Service are for people aged 65+ who have ‘fallen’. – > 40% are not even taken into Hospital. Specialist PSI Exercise Module Reported falling by age and sex 50 40 % fallen 30 in last month 20 Men Women 10 0 75-79 80-84 85-89 90-94 95+ Cambridge City Over 75s Cohort Study, Fleming, 2002 Specialist PSI Exercise Module Reported falling by Residence 50 40 75-84 85+ % fallen 30 in last month 20 10 0 Institutional Care Sheltered Housing House/flat Cambridge City Over 75s Cohort Study, Fleming, 2002 Specialist PSI Exercise Module Time and Location of Reported Falls 100 Men Women 80 % fallen 60 in last three 40 months 20 0 Day Night Indoors Outdoors Cambridge City Over 75s Cohort Study, Fleming, 2002 Specialist PSI Exercise Module Indoor location of falls 35 30 25 % of 20 all falls 15 65-74 75-84 85+ 10 5 0 Level Shower / Getting On Stairs Chair / Surface Bath Out of Ladder Bed Lord 1993 Specialist PSI Exercise Module Reported falling by distance of walking ability 40 30 % 20 10 0 Around town 1 block Garden Gate Only indoors A few steps Cambridge City >75s Cohort, Fleming, 2002 Specialist PSI Exercise Module Reported falling by need for help with walking 50 40 % fallen in last month 30 20 10 0 No aid Stick Frame Someone to help Wheelchair Cambridge City Over 75s Cohort Study, Fleming, 2002 Specialist PSI Exercise Module Types of Injurious falls • One which results in a visit to or by a health professional. • 20% of injurious falls result in fractures requiring hospital treatment. • Other injuries include: – – – – – – Cuts and lacerations, Deep bruises, Soft Tissue Injuries, Dislocations, Sprains Increase in joint pain Specialist PSI Exercise Module Types of ‘fallers’ • FLOF Found Lying On the Floor • FAOP Falling All Over the Place • FBS Fall Back Syndrome • 3F syndrome Fear of Falling Further • 3G syndrome Grabbing Great Grandmother • 3P syndrome Patient with Precocious parking • FNOF Fractured Neck Of Femur Medical Intrinsic Intrinsic Fear Medical & Intrinsic Specialist PSI Exercise Module Changing incidence of fractures with increasing age • 50 to 65 yrs - wrist • 55 to 85 yrs - spine • 75 to 85 yrs - hip (because of poor reaction, coordination and reflexes) Specialist PSI Exercise Module Consequences of Hip Fracture • By Year 2031 = 96,000 hip fractures a year. • Risk of a hip # 10x higher for those in residential settings than in own home • 50% of individuals will die, move into a nursing home or be in hospital within six months of Hip # • 80% do not regain pre-fracture mobility • underlying medical conditions, poor strength, balance and muscle asymmetry all contribute to poor outcome Specialist PSI Exercise Module Consequences to the individual • Falls and instability contribute to 40% of nursing home admissions. • Post-fall syndrome - psychological sequelae • Reduction in independence and social contact • Depression • Frequent fallers (>3 p.a.) have poor outcomes. Nearly a third admitted to hospital, transferred to nursing home or had died one year later (Lord et al., 1992). Specialist PSI Exercise Module Long lies with or without injury • Long lies (> 1-2 hours) lead to an increased risk of: – dehydration – hypothermia – pneumonia – pressure sores – kidney failure – depression – post fall syndrome – death (Tinetti 1993, 1994) Specialist PSI Exercise Module DoH Prevention Package 2009 Counting the cost • Hip fractures cost the NHS in England £1.8 billion a year. • The direct cost to commissioners of a hip fracture is estimated to be £10,000 – plus the cost of local authority social care. • One-third of people who experience a hip fracture are unable to continue to live independently afterwards. • An effective falls and fracture prevention service can make direct savings of £290,708 over five years for a primary care trust with a population of 320,000. Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Physical Activity, Older People and Falls: Research Update • The effects of ageing on performance • Exercise to prevent falls • Holistic benefits of exercise • Inactivity in the UK • Exercise as part of a multifactorial intervention Specialist PSI Exercise Module AGEING AFFECTS ALL OF US 1-2% in functional ability p.a. – Strength – Power – Bone density – Flexibility – Endurance – Balance and co-ordination – Mobility and transfer skills Sedentary behaviour accelerates the loss of performance... Specialist PSI Exercise Module QUADRICEPS STRENGTH Men Women 10 8 6 Threshold level of strength for independence 4 2 70-74 65-69 60-64 Age (years) 55-59 70-74 65-69 60-64 55-59 0 50-54 Strength to be confident of rising from low chair without using arms 50-54 Knee extension strength (N/kg) 12 Specialist PSI Exercise Module FUNCTION FOR LIFE Wash hair comfortably? 20% women & 14% of men > 50 do not have sufficient shoulder flexibility Confident of getting out of a chair without using arms ? 25% women & 7% men aged 70 – 74 do not have sufficient leg strength Ease of stair use? 47% women aged 70 – 74 do not have sufficient leg power Walk comfortably at a 20 minute a mile pace? Nearly 10% men & over 35% women aged 50 – 74 do not have sufficient aerobic capacity 35% men and 80% women aged 70 – 74 Specialist PSI Exercise Module Sedentary vs active lifestyles • >3 hrs per week targeted exercise – myocardial infarct - 3 x less likely – Osteoporosis - 2 x less likely – Fall-related injuries & Hip fracture - 2 x less likely • WHO, 1996 “regular physical activity helps to – “preserve independent living” and – “postpone the age associated declines in balance and co-ordination that are major risk factors for falls” – WHO, 2011 “physical activity (for 65+ year olds) – improves cardiorespiratory and muscular fitness, bone and functional health, and reduces the risk of NCDs, depression and cognitive decline” Specialist PSI Exercise Module Exercise to Prevent Falls Exercise could help fallers in a number of ways: • Reducing Falls (or injurious falls) • Reducing known Risk Factors for Falls • Reducing Fractures (or changing the site of fracture) • • • • Increasing Quality of Life & Social Activities Reducing Fear Reducing Long Lies Reducing Institutionalisation Specialist PSI Exercise Module Fracture Prevention Triangle Exercise can increase BMD and alter bone properties Exercise can reduce falls FALLS FRAGILITY FRACTURE Exercise can increase muscle strength (padding) and improve reaction times FORCE Specialist PSI Exercise Module Specificity of Exercise to Reduce Falls Province, 1995 Group and individual balance and strength training >65’s Wolf, 1996 Group Tai Chi >65’s (NOT >70’s at risk, Wolf 2003) Campbell, 1997 Home-based exercise >80’s Robertson, 2001 Home-based exercise >65’s and >80’s Day, 2002 Group exercise >70’s at risk Barnett, 2003 Group exercise >65’s at risk Lord, 2003 Group exercise >60’s retirement village Means, 2003 Group exercise >65’s, psychosocial effects Liu-Ambrose, 2004 Group exercise for >75s with low bone mass Skelton, 2005 Group exercise >65’s frequent fallers Specialist PSI Exercise Module Not “ALL” Exercise works to Prevent Falls Effective Ineffective to prevent falls but effective on falls risk factors………… Barnett 2003 Lord 2003 Morgan 2004 Skelton 2005 Buchner 1997 Campbell 1997 Campbell 1999 Cornillon 2002 Day 2002 Robertson 2001 Wolf 1996 Bunout 2005 Campbell 1999, 2005 Carter 2002 Ebrahim 1997 Latham 2003 Lord 1995 McMurdo 1997 Mulrow 1994 Pereria 1998 Reinsch1992 Schnelle 2003 Steinberg 2000 Wolf 2003 • Insufficient tailoring • Insufficient duration • Too much time seated • Not an emphasis on strength and balance • Not delivered by trained personnel • Not progressive • Not intensive enough Specialist PSI Exercise Module Effective Duration of Exercise Provision / Benefit • Strength, Power, Static balance, Gait 8-12 wks • Dynamic balance, Endurance 12-24 wks • Bone strength (hip, spine and wrist) 36+ wks • Dizziness and Postural Hypotension 24+ wks • Transfer skills 24+ wks • Mood, Depression, anxiety, self-esteem 12+ wks • Falls 15-52 wks Specialist PSI Exercise Module Interventions in the community • Update of 2009 review • • 159 trials with 79,193 participants • most common interventions tested Group and home-based exercise programmes, and home safety interventions delivered by an occupational therapist reduce rate of falls and risk of falling. • Multi-factorial assessment and – exercise as a single intervention programmes reduce rate of intervention (59 trials) falls but not risk of falling; – Multi-factorial programmes • Tai Chi reduces risk of falling. (40 trials) Gillespie et al. Interventions for preventing falls in older people living in the community. Cochrane Library 2012 Specialist PSI Exercise Module Exercise interventions • Multiple-component group exercise significantly reduced rate of falls (RaR 0.71; 16 trials) and risk of falling (RR 0.85; 22 trials) • Multiple-component home-based exercise (RaR 0.68; 7 trials; and RR 0.78; 6 trials). • Multiple-component exercise (balance and strength training) embedded in activities of daily living in people with a history of falls significantly reduced rate of falls (RaR 0.21; 1 trial) but not risk of falling. • Tai Chi, the reduction in rate of falls bordered on statistical significance (RaR 0.72; 5 trials) but Tai Chi did significantly reduce risk of falling (RR 0.71; 6 trials). Gillespie et al. Interventions for preventing falls in older people living in the community. Cochrane Library 2012 Specialist PSI Exercise Module New Zealand RCTs - OTAGO Individually tailored programme: Campbell, BMJ 1997 -80+ years, n=233, home-based, physiotherapist -1 year, falls 32%, injuries 39% Nurse delivered programme at home: Robertson, BMJ 2001 -75+ years, n= 240, home-based, district nurse -1 year, falls 46%, serious injuries and hospital costs Nurse programme at GP centres: Robertson, BMJ 2001 -80+ years, n=450, home-based, general practice nurse -1 year, falls 30%, injuries 28% Visually Impaired Older People: Campbell, BMJ 2005 -1 year, home-based. Only effective with full compliance, falls 28% 6 month programme: Liu-Ambrose, JAGS 2008 -70+ years, home-based, cognitive function improvements after 6 months and after 1 year falls 47% Specialist PSI Exercise Module FaME – Group & Home-based • Randomised controlled trial – Exercise Only • Women aged 65+, > 3 falls last year • Exercise-only intervention – 9 months • Falls decreased by 60% • Injurious falls decreased by 75% • Skelton et al. Age Ageing 2005 Co-workers: O.Rutherford and S.Dinan Specialist PSI Exercise Module STRENGTH / POWER / ASYMMETRY Significant isometric and isokinetic improvements in the exercise group: • Ankle Plantarflexion 60% • Ankle Dorsiflexion 40% • Ankle Inversion 25% • Ankle Eversion 30% • Hip Flexion 20% • Lower Limb Power 25% • Asymmetry reduced 15% Specialist PSI Exercise Module BALANCE & MOBILITY Mean % change (from baseline) post-training 120 Exercise Group Control Group 80 40 0 -40 Balance-eyes open (secs) Balance-eyes closed (secs) Functional Reach (cm) Timed Up and Go (sec) Floor rise (sec) Specialist PSI Exercise Module BONE Significant difference with time and group for L2-L4 spine and Wards Triangle (F=3.46, p<0.05). Exercisers n=32, Controls n=14. Time between visit 1 and visit 2 = mean 10.9 (sd 2.7) months Specialist PSI Exercise Module FALLS DURING INTERVENTION controls (RR 1.19) • less likely to have injurious fall (RR 0.51) DURING FOLLOW UP • Exercisers had half the risk of falls compared to controls (RR 0.53) • 1.8 1.6 1.4 Exercisers slightly increased risk of falls Relative Risk • compared to 1.2 1 0.8 0.6 0.4 0.2 0 Intervention Follow-up ++ less likely to have injurious falls (RR 0.39) THREE YEARS FROM BASELINE • 10% of exercisers had died, were in Hospital /in a nursing home vs 33% of controls Specialist PSI Exercise Module QUALITY OF LIFE • Improvements in ALL domains of SF36 • Self-reported improvements in – – – – – – Caring skills Playing with grandchildren Bathing instead of showering Using public transport again Reduced anxiety and fear Confidence • Fallen Angels Club – Meet every two months in Starbucks, Oxford Street, London, UK! Specialist PSI Exercise Module MORBIDITY AND MORTALITY 80% of over 80’s would rather be dead than suffer the loss of independence that moving to a nursing home would bring (Salkeld, 2000). • It’s NEVER TOO LATE (Fiatarone, 1990) Specialist PSI Exercise Module Can exercise prevent fractures? • Fractures more common in sedentary people • Cochrane Review suggests that exercise does reduce risk of fractures (2009 & 2012) • It is possible to increase BMD in older people (Welsh 1996; Kohrt 1995; Verschueren 2004) • It is possible to increase BMD in fallers (Skelton 2005; Liu Ambrose 2004) Specialist PSI Exercise Module Author, year Effect size (95% CI) Barnett, 2003 Bunout, 2005 Buchner, 1997 Campbell, 1997 Campbell, 1999 Campbell, 2005 Carter, 2002 Cerny, 1998 Day, 2002 Ebrahim, 1997 Faber, Functional walking, 2006 Faber, Tai Chi, 2006 Green, 2002 Hauer, 2001 Korpelainen, 2006 Latham, 2003 Li, 2005 Lin, 2007 Lord, 1995 Lord, 2003 Liu-Ambrose, Resistance, 2004 Liu-Ambrose, Agility, 2004 Luukinen, 2007 McMurdo, 1997 Madureira, 2007 Means, 2005 Morgan, 2004 Mulrow, 1994 Nowalk, Resist./Endurance, 2001 Nowalk, Tai Chi, 2001 Protas, 2006 Reinsch, 1992 Resnick, 2002 Robertson, 2001 Rubenstein, 2000 Sakamoto, 2006 Schoenfelder, 2000 Schnelle, 2003 Sihvonen, 2004 Skelton, 2005 Steinberg, 2000 Suzuki, 2004 Toulotte, 2003 Voukelatos, 2007 Wolf, Tai Chi, 1996 Wolf, Balance, 1996 Wolf, 2003 Woo, Tai Chi, 2007 Woo, Resistance, 2007 Overall (I-squared = 61.5%, p = 0.000) 0.60 (0.36, 0.99) 1.88 1.22 (0.70, 2.14) 1.67 0.61 (0.40, 0.94) 2.21 0.68 (0.52, 0.89) 3.13 0.87 (0.36, 2.10) 0.88 1.15 (0.82, 1.61) 2.74 0.88 (0.32, 2.41) 0.70 0.87 (0.17, 4.29) 0.31 0.82 (0.70, 0.97) 3.80 1.29 (0.90, 1.83) 2.64 1.32 (1.03, 1.69) 3.31 0.96 (0.76, 1.22) 3.34 1.34 (0.87, 2.07) 2.21 0.75 (0.46, 1.25) 1.89 0.79 (0.59, 1.05) 3.05 1.08 (0.87, 1.35) 3.46 0.45 (0.33, 0.62) 2.87 0.67 (0.32, 1.41) 1.13 0.85 (0.57, 1.27) 2.38 0.78 (0.62, 0.99) 3.38 1.80 (0.67, 4.85) 0.72 1.03 (0.36, 2.98) 0.65 0.93 (0.80, 1.09) 3.85 0.53 (0.28, 0.98) 1.48 0.48 (0.25, 0.93) 1.34 0.41 (0.21, 0.77) 1.40 1.05 (0.66, 1.68) 2.04 1.26 (0.90, 1.76) 2.75 0.96 (0.63, 1.46) 2.27 0.77 (0.46, 1.28) 1.88 0.62 (0.26, 1.48) 0.88 1.24 (0.77, 1.98) 2.04 0.71 (0.04, 11.58)0.11 0.54 (0.32, 0.91) 1.84 0.90 (0.42, 1.91) 1.11 0.82 (0.64, 1.04) 3.34 3.06 (1.61, 5.82) 1.40 0.62 (0.38, 1.00) 1.98 0.38 (0.17, 0.87) 0.98 0.69 (0.50, 0.96) 2.81 0.90 (0.79, 1.03) 3.97 0.35 (0.14, 0.90) 0.80 0.08 (0.00, 1.37) 0.10 0.67 (0.46, 0.97) 2.56 0.51 (0.36, 0.72) 2.67 0.98 (0.71, 1.34) 2.86 0.75 (0.52, 1.08) 2.58 0.49 (0.24, 0.99) 1.22 0.78 (0.41, 1.48) 1.41 0.83 (0.75, 0.91) 100.00 .25 .5 Favours exercise 1 2 % Weight Systematic Review of Exercise and Falls But would you want to be in these sessions? 17% reduction in falls Sherrington et al., 2008 and 2011 4 Favours control Specialist PSI Exercise Module What makes the difference? • Greatest effects of exercise on fall rates from interventions including: – Highly challenging balance training – High dose (50+ hours) – No walking programme Sherrington et al., JAGS 2008, NSWPHB 2011 Specialist PSI Exercise Module Conclusion of 2011 Systematic Review – Best Practice Recommendations: • Exercise must provide a moderate/high challenge to balance • Sufficient exercise dose (50 hours) • Ongoing exercise • Target general community as well as those at high risk • Brisk Walking should not be prescribed to high risk individuals • Strength training may be included in addition to balance Sherrington et al., 2011 Specialist PSI Exercise Module WHAT’S THE DIFFERENCE? Gardening • Physical Activity – any bodily movement produced by skeletal muscles that results in energy expenditure. DIY Housework Bowling • Exercise – planned, structured and repetitive bodily movement undertaken to improve or maintain one or more components of physical fitness. Bouchard 1990 Walking Cycling Exercise class Sports Specialist PSI Exercise Module THE BENEFITS OF EXERCISE Prevention of : disease Coronary Heart Disease, Osteoporosis, Obesity, Stroke, Depression, Type 2 Diabetes, Hypertension, Some Cancers disability Arthritis, Intermittent claudication, Angina, Sleep, Low back pain complications of immobility Constipation, Deep vein thrombosis, isolation Socialisation, Self-efficacy, Confidence dependence Functional ability, Falls, Autonomy, Dignity, Caring skills Oedema, Pressure sores Specialist PSI Exercise Module BENEFITS OF REGULAR PHYSICAL ACTIVITY IMPROVES OR MAINTAINS • • • • • Good posture & body image Intake of nutrients and immunity to infection Cerebral function, mood, memory Sleep pattern and duration Social contacts INDEPENDENCE AND QUALITY OF LIFE REDUCES OR PREVENTS • • • • Falls risk and fear of falling Breathlessness, fatigue Incontinence, urinary urgency Anxiety, Depression, Stress DEPENDENCE AND ISOLATION Specialist PSI Exercise Module New CMO Guidelines for Older adults (Start Active, Stay Active 2011) • Older adults should aim to be active daily. Over a week, activity should add up to at least 150 minutes of moderate intensity activity in bouts of 10 minutes or more. • Older adults should also undertake physical activity to improve muscle strength on at least two days a week. • Older adults at risk of falls should incorporate physical activity to improve balance and co-ordination on at least two days a week. • All older adults should minimise the amount of time spent being sedentary (sitting) for extended periods. 82 Specialist PSI Exercise Module A VISCIOUS CYCLE OF INACTIVITY Physical deterioration - Heart disease - High blood pressure - Aches and pains - Osteoporosis Further decrease in physical activity Social / psychological ageing - Feeling ‘old’ - ‘Acting’ one’s age - Increased stress - Anxiety, depression - Low self-esteem Increasing age Less exercise Decreased physical abilities - Increased body fat - Sagging muscles - Decreased energy Specialist PSI Exercise Module UK’S SEDENTARY WAYS • 40% of people aged 50 or over in the UK are sedentary • 60-85% are sedentary in ethnic minority groups Half of the sedentary over 50’s and 2/3 of over 70’s believe they take part in enough physical activity to keep fit. Specialist PSI Exercise Module Inactivity related disease? • Disuse rather than disease? • 1 wk bed rest strength by ~ 20% • 1 wk bed rest spine BMD by ~1% • Nursing home residents spend 80-90% time seated or lying down to ‘Inactivity related of their - leading disability’ Specialist PSI Exercise Module Walk with me ! • Walk from Home - Keighley Mary Moffat - 93 – Referred by physio after a fall – Loss of confidence and fear of falling – Isolated and lonely and dependent upon others to get out Specialist PSI Exercise Module BUT not all physical activity is safe for fallers! • RCT Increasing physical activity in people with previous upper arm fracture (Ebrahim 1997) • Intervention: Brisk walking • Control: exercise of upper arm • Falls risk ↑ (Brisk walking > control) • Fracture risk ↑ (Brisk walking > control) NICE 2004 & Sherrington 2011 do not recommend brisk walking! • Beware unsafe pavements! • PA / Exercise has a complicated relationship with falls – more activity increases exposure to risk…. Specialist PSI Exercise Module Physical Activity vs Falls • Brisk walking correlates with better postural stability in postmenopausal women (Brooke-Wavell 1998). – Yet a brisk walking intervention in fallers caused an increased incidence of falls and fractures (Ebrahim 1997) • Most falls occur at periods of maximal activity (Luukinen 1994) – Yet, Hip fractures are less common in active people (Gregg 1998) • U-shaped relationship in amount of physical activity and number of falls (Gregg 1998) • Community dwelling frequent fallers are less habitually active than nonfallers (Skelton 2002) Specialist PSI Exercise Module Unsupported forward flexion may be risky for those with previous spinal fractures……. Type of Exercise Reoccurrence of Fracture • Back extension 16% • Flexion (abd. curls) 89% • Combined 53% • No exercise 67% Sinaki & Mickelson 1982 Specialist PSI Exercise Module Patients in Hospital • Tai Chi + reaching + stepping + transferring chair to chair • 1 physiotherapist to max 4 patients, 3 x p/w, 45 mins. • 173 patients, 82 yrs, sub-acute ward • Halved the number of falls (participant days in hospital) Haines et al. Clin Rehab 2007 Specialist PSI Exercise Module Exercise alone? In high risk 7% reduction in fall rate in residential care settings but this was not statistically significant (p=0.446) Sherrington et al, 2011 BUT interventions which provided a challenge to balance, a high dose of exercise and no walking were close to significant SO….same recommendations apply Specialist PSI Exercise Module Part of a multi-factorial intervention…care homes Reduces falls - Becker et al. JAGS 2003 Improves mobility - Jensen et al. Aging Clin Exp Res 2004 Reduces falls risk factors - Dyer et al. Age Ageing 2004 Works better in those with cognitive impairment!!! – Rapp et al. 2008 Specialist PSI Exercise Module Population Approaches including increasing physical activity Do they work? • Significant decreases or downward trends in fall-related injuries reported in five large studies • Relative reduction in fall-related injuries 6 to 33% • All Interventions included – Education, advice, medication use, footwear, home hazard reduction, promotion of physical activity • Some included – public lighting, public roadways, housing planning McClure et al. 2005 Systematic Review Specialist PSI Exercise Module Comparison to NICE guidance 100 90 80 70 60 NICE Assessment Intervention Direct 50 40 30 81% run strength and balance training classes BUT Average duration 8 weeks and frequency once per week! 20 10 0 Bone Health Vision Gait & Balance Lamb et al, SDO report, 2007 Specialist PSI Exercise Module Royal College of Physicians Report March 2012 • Audit on NHS exercise provision in falls services across the UK • First, the good news! – Over 1,700 older people - 96% felt the exercises were beneficial/quite beneficial, and 95% were satisfied/very satisfied with their exercise programme • Now, the not so good news! – 86% low frequency (once per week) – 29% of patients used ankle weights for resistance training – 52% of patients - exercise programme had been progressed – 81% of patients - classes had lasted 12 weeks or less – 73% of patients - home programme lasted for 3 months or less – Only 54% of sites had PSI trained staff and 41% of sites had Otago trained staff Specialist PSI Exercise Module “Man does not cease to play because he grows old. Man grows old because he ceases to play” George Bernard Shaw If I’d known I was going to live this long, I’d have taken better care of myself Dubey Blake Specialist PSI Exercise Module Risk Factors for Falls (and injuries) - intrinsic - extrinsic - modifiable with exercise Specialist PSI Exercise Module A Risk continuum ? • Over 200 risk factors documented in the literature D A 80 70 60 Drugs and alcohol Age related physiological changes M Medical E Environment 50 % Falling (12 months) 40 30 20 10 0 0 1 2 3 4+ Specialist PSI Exercise Module Intrinsic vs Extrinsic - we are all ‘trippers’ • Over HALF the falls experienced in the home are due to environmental hazards - trips, slips, unsafe or unlit stairways • A decline in a person’s intrinsic risk factors (declining function and balance) mean that the extrinsic risk factors (loose mats, slippery floors) no longer just cause a correctable trip - they cause an injurious fall Specialist PSI Exercise Module D - Drugs and Alcohol • Cumulative effect of medication / time of day • Prescribed medications / multiple drug regimes – Analgesics – Sedatives – Diuretics - Antidepressants - Antipscyhotics - ANY 4 OR MORE MEDICATIONS • Heavy drinkers (>7 units per week) (Campbell et al., 1989, O’Loughlin et al., 1993) • Mixing medications with alcohol Specialist PSI Exercise Module A - Age related physiological changes • Deterioration in physical functions and systems (strength, power, endurance, coordination, reaction, balance, proprioception and neural control, asymmetry) • Decrease in functional capacity, mobility and activity • Deterioration in feet (bunions, corns, circulation, neuropathies) • Increase in cognitive impairment and depression Specialist PSI Exercise Module Psychological risk factors • Fear of falling • Avoidance of activity • Reduced quality of life • Increased anxiety Specialist PSI Exercise Module M - Medical • Acute Infections • Cardiovascular control - postural hypotension, drop attacks, heart disease, stroke, tia’s • Dementia, Alzheimer’s Disease • Parkinson’s Disease • Thyroid dysfunction Peripheral Neuropathies or myopathies Malignancies Impaired hearing or vestibular function (Menieres Disease, Tinnitus) Impaired vision (macular degeneration, glaucoma, cataracts, visual acuity, contrast sensitivity, adaptation to dark) Specialist PSI Exercise Module M - Medical 2 • Foot deformities – pain, bunions, corns, hard skin, arthritis, oedema Urinary incontinence or urgency Receiving community health or social services Recent discharge from hospital Use of assistive walking aids - cane, zimmer • Malnutrition / Anaemia - Nutritional recommendations are 10-20g rda Vitamin D and 1,000mg rda calcium, Vit B12 deficiency leads to sensory abnormalities Specialist PSI Exercise Module E - Environment Personal risk factors: • glasses (bifocals and varifocals) • footwear and clothing Outdoors: Indoors: • Poorly lit pathways • Loose carpets • Uneven pavements • Wires and cables • Slippery leaves • Unstable furniture • Rubbish, building materials, obstacles • Change of level • Bus drivers! • Cold rooms • Poor lighting Sentimentality or “never been a problem before” Specialist PSI Exercise Module Not modifiable with tailored exercise • vision problems • gender • multiple medications • social class • chronic medical conditions • poor housing • hypothermia • poor heating • malnutrition • poor footwear • age exercise may not have a major effect Specialist PSI Exercise Module Modifiable with tailored exercise • • • • • • low strength low power poor gait poor mobility poor balance arthritis • • • • • depression postural hypotension cognitive impairment urinary urgency fear of falling exercise is likely to have a major positive effect Specialist PSI Exercise Module How can we identify older people at high risk of falling? • AGS/BGS guidelines - “get up and go” test as a filter for a full assessment by a specialist clinician for people who have fallen at least once. J Am Geriatr Soc 2001; 49: 664 – 672. • Falls Risk Assessment Tool (FRAT) – 5 questions to assess risk. J Public Health 2004; 26:138- 143. ?? Usefulness in residential/nursing settings Specialist PSI Exercise Module FRAT - Assessment of falls risk in older people Is there a history of any fall in the previous year? How assessed? Ask the person. Is the patient / client on four or more medications per day? How assessed? Identify number of prescribed medications. Does the patient / client have a diagnosis of stroke or Parkinson's Disease? How assessed? Ask the person. Does the patient / client report any problems with their balance? How assessed? Ask the person. Is the patient/client unable to rise from a chair of knee height? How assessed? Ask the person to stand up from a chair of knee height without using their arms. Specialist PSI Exercise Module PROFET: targeting risk factors (Close et al. Lancet 1999) • Medical assessment • • • • • • General medical Postural hypotension Visual acuity Balance Cognition and affect Corotid sinus syndrome • Occupational Therapy • • • • Function Physical handicap Psychological handicap Environmental hazards • Referral / intervention – – – – – Day hospital GP O/P Optician Social services – Supply minor equipment The rate of falls was reduced by 60% Specialist PSI Exercise Module Tinetti (1994) - Multifactorial Risk factor Intervention Postural hypotension (N) - postural exercise (ankle pump) - medication review and adjust Use of sedative-hypnotic medication (N) - taper-off and discontinue - non-pharm. treatment of sleep problems Use of 4+ medications (N) - medication review and adjustment Unsafe bath or toilet transfers (N) - transfer training - environmental adjustment Gait / balance impairment (P) - gait, balance and/or strength exercise - use of aids Less than full range of motion against resistance (P) - resistance exercises The rate of falls was reduced by 30% Specialist PSI Exercise Module Posture & Postural Training Practical Specialist PSI Exercise Module Specialist PSI Exercise Module Specialist PSI Exercise Module Ideal Posture Specialist PSI Exercise Module poor habitual posture • poor bio-mechanical alignment • poor muscle balance • adaptive soft tissue shortening • compression & stretch of nerves & blood vessels • abnormal movement • affects balance mechanisms • increased risk of injury & disease • fear of challenging situations • inactivity • Isolation, depression Specialist PSI Exercise Module Specialist PSI Exercise Module Specialist PSI Exercise Module Seated Posture • Position of head, eyes, chin • Position of arms, shoulders, elbows, wrists • Position of spine - cervical/ thoracic/ lumbar • Position of pelvis • Position of legs, hip, knee & foot • Overall tone • Forward Flexion Specialist PSI Exercise Module Checklist for Standing Posture Assessment • Front – – – – – – – – Eyes Chin Clavicles Ribs Hips Knees Ankles Arch of feet • Side • Back – Angle of head / jaw / spine – Shoulder – Pelvis – Hand – Back of knee – Angle of spine / jaw – Shoulder – Scapulae / Sacro-iliacs – Back of knees – Ankles – Heels and arch of feet Specialist PSI Exercise Module Muscle, Endocrine and Nervous Systems A bit on structure and function (but not a lot!) Effects of Ageing Differences in fallers Effects of Training Specialist PSI Exercise Module Main Communication Systems • NERVOUS SYSTEM – rapid communications (seconds) – Nerve Fibres • ENDOCRINE SYSTEM – Slow transmissions (mins to hours) – Hormones • CO-ORDINATION – Nerves stimulate and inhibit hormones – Hormones can stimulate/inhibit nerve electrical impulses • ACTION – Muscles ! Specialist PSI Exercise Module Function of Nervous System Control Activation Integration Modification Sensory Input Central Processing Motor Output Specialist PSI Exercise Module Nervous System Structure • Central – Spinal Cord – Brain • Peripheral – Spinal (31) and cranial (12) nerves • Myelinated (faster) and unmyelinated – Somatic (voluntary) – Autonomic (involuntary) • Sympathetic (speeding up) • Parasympathetic (slowing down) • Sensory nerves – ‘Away’ from receptors TO CNS • Motor nerves – ‘Exiting’ CNS TO produce response Specialist PSI Exercise Module Bridging the gap between nerve cells and other cells Synapses - ‘the connectors’ Action Potential crosses synaptic cleft via chemical neurotransmitter release Acetylcholine, Noradrenaline, Dopamine - ‘neurotransmitters’ Specialist PSI Exercise Module SIMPLE OR REPETITIVE MOVEMENTS Spinal reflexes - Reflex Arc (brain still informed!) COMPLEX MOVEMENTS Brain-stem reflexes - complex reflexes Balance Specialist PSI Exercise Module Cortex Cerebellum Basal Ganglia Brainstem Spinal Cord Multi-linked Musculoskeletal System Multi-sensory Information Vestibular Visual Proprioceptive Cutaneous Environment Specialist PSI Exercise Module Sensory Input Stability Three main sources of input • Visual information • Vestibular information • Proprioceptive information Specialist PSI Exercise Module Functions of ENDOCRINE SYSTEM • Affects bodily activities by releasing hormones into the bloodstream – target organ or system function (metabolism) – regulates chemical composition and volume – responds to emergency situations • Coordinates activities with the nervous system – – – – nerves stimulate / inhibit hormones hormones stimulate/ inhibit nerve impulses nervous control = seconds hormones = minutes to hours • Tightly regulated Specialist PSI Exercise Module Endocrine System • Central nervous control – hypothalamus produces ‘releasing’/’inhibiting’ chemical secretions • Endocrine glands (eg. pituitary, thyroid, adrenals) • Hormones bloodstream target organs • Anabolic ( – Catabolic ( tissue growth) tissue loss) Specialist PSI Exercise Module Anabolic Hormones • Growth Hormone • maintenance of muscle and bone in adulthood • decreased levels - loss of muscle and bone and increase in fat • Insulin • influences blood sugar levels • allows storage of sugars in muscle and fat cells • Type I Diabetes Mellitus - insulin replacement – Short term - ‘hypos’, muscle fatigue, neural control – Long term - peripheral nerve damage Specialist PSI Exercise Module Anabolic Hormones • Thyroid Hormones • affect metabolic rate • too much - hypersensitivity, weight loss, eventual bone loss • too little - lethargy, weight gain • Oestrogens and Androgens control – our gender – the growth of muscle and bone – the maintenance of muscle and bone in later life – ‘menopause’ • Parathyroid hormone (covered in Bone lecture) Specialist PSI Exercise Module CALCIUM REGULATING ANABOLIC HORMONES • Major controllers – Parathyroid Hormone (PTH) and active form of Vitamin D – control serum levels of calcium - excitability – ‘retrieve’ calcium from bone and absorption in kidney • Vit D from diet and sunlight – produced in kidney – absorption of calcium from gut – mineralisation of bone • Vit D = PTH released – Long term PTH release leads to bone loss Specialist PSI Exercise Module Catabolic Hormones • Cortisol (in excess) – reduces inflammatory reactions – increases blood glucose levels – produced as a response to stress – causes muscle and bone loss – causes fat gain – central effects - depression Specialist PSI Exercise Module CALCIUM / VIT D INTAKE • Essential for – Muscle contraction – Bone density – Teeth and nails • The course recommendations for participants – Calcium 1000 mg/day, Vit D 20g/day • See foods handout Specialist PSI Exercise Module Muscular System • Functions – Motion – Maintenance of posture – Immune Function – Heat production • Types – Skeletal - striated and voluntary – Cardiac - striated and involuntary – Smooth - non striated and involuntary Specialist PSI Exercise Module – Muscle bundle – Muscle Fibres – Connective Tissue – Sarcomeres – Sarcoplasmic reticulum (Calcium) – Cross-bridges – Protein filaments Structure • actin (thin) • myosin (thick) – Mitochondria – Rich blood and nerve supply Specialist PSI Exercise Module Type 1 Type 2 Slow Fast Non-fatiguable Fatiguable Oxidative Non-oxidative Specialist PSI Exercise Module Power • Product of strength (Type 2 fibres) and speed • Functionally relevant • Affected by temperature changes • Asymmetry in lower limbs of fallers Specialist PSI Exercise Module Sedentary behaviour • Immobilisation reduces muscle mass, muscle strength and power (Appell 1990) • Lower limb muscles and faster Type 2 muscles fibres are particularly vulnerable (Broomfield 1997) • 27 days of bed rest has lead to the loss of 0.9% of bone mineral density per week (Frost, 1990). Specialist PSI Exercise Module active, strength-trained The same size difference is seen between 30 yr old and 80 yr old 70 yr old females sedentary (Adapted from Sipilä & Suominen Muscle Nerve 1993;16:294) Specialist PSI Exercise Module Ageing, falling…what are the effects ? • Effects of ageing • Differences in fallers Specialist PSI Exercise Module Effects of Ageing on the Nervous System • Neurones (somatosensory, vestibular and visual) • Spinal Cord Axons • Speed of transmission • Speed of central processing • Changes in sensory input – Mass and strength in eye muscles, Elasticity in lens, Hydration of the eye, Eye Infections – Viscosity of fluid in inner ear, medications that affect vestibular system – number and efficiency of Proprioceptors, medications that reduce efficiency of proprioceptors, oedema Specialist PSI Exercise Module Functional Consequences of an ageing nervous system • Poorer short term memory • Slower learning and performance • Poorer kinesthetic awareness • Poorer reaction / coordination integration • Poorer complex task performance • Difficulty comprehending floor patterns/textures • Simple movement tasks, repetition and rehearsal • Longer transition times • Effective verbal and visual cueing • Functional moves Specialist PSI Exercise Module EFFECTS OF AGEING on the ENDOCRINE SYSTEM • Hormones – less well regulated – Some glands produce less hormone • Target tissues and organs – less responsive, poor circulation • System becomes more catabolic – Calcium intake reduced and sunlight exposure reduced ↓ anabolic hormone production ↑ Cortisol – Cortisol release – Less anabolic hormone production • Metabolism and hormone diseases more prevalent • Side effects of medication (eg. Secondary osteoporosis) Specialist PSI Exercise Module FUNCTIONAL CONSEQUENCES of an AGEING ENDOCRINE SYSTEM • Musculo-skeletal injuries • Fatigue • Dizziness / Fainting • Arrythmias • ‘Hypos’ • Dehydration • Longer warm up and warm-down • Fartlek training approach • Observation Specialist PSI Exercise Module Effects of Ageing on MUSCLE • No. & size of muscle fibres – Preferentially type 2 fibres • Muscle mass • No. motor units & size of remaining motor units (therefore loss of fine control) • Turnover of contractile proteins • No. and size of mitochondria • Proprioception in muscle and tendon • Connective tissue and fat • heat production • Susceptibility to injury and damage Specialist PSI Exercise Module Functional Consequences of Ageing of the Muscle System • Weaker muscles • Slower muscles • Fatigue • Poorer temperature maintenance • Poorer immune function • Poorer functional reserve • Target major functional muscle groups • Time for rest • Fartlek training approach • Effective warm-up, warm-down and stretches Specialist PSI Exercise Module Differences in Fallers NERVOUS SYSTEM / SENSORY INPUTS • Visual impairment a risk factor – – – – Contrast sensitivity Depth Perception Visual Field Visual acuity • Cognition a major risk factor – Dementia – Alzheimers – Dehydration Fallers have: Worse balance Larger sway Worse gait Difficulty in dual tasking • Nervous System control of movement – Parkinsons Disease – Stroke • Vestibular impairment = more falls • Peripheral neuropathy (eg. Lack of proprioceptive feedback) = more falls Specialist PSI Exercise Module Differences in Fallers ENDOCRINE SYSTEM / DISEASE • Those with metabolic / endocrine diseases are more likely to fall – Diabetes – Hypothyroid • Those with secondary bone loss due to endocrine disease more likely to fracture if they do fall Specialist PSI Exercise Module Differences in Fallers MUSCULAR SYSTEM – STRENGTH • Community dwelling frequent fallers have weaker ankle dorsiflexion strength than non-fallers (Skelton 2002) • Community dwelling fallers have reduced hip extensor and adductor strength, they tend to weigh more and have increased medio-lateral sway standing on foam (Quinn 2003) • Nursing home fallers are weaker in quadriceps and hamstring strength than non-fallers (Whipple 1987) Specialist PSI Exercise Module Differences in Fallers MUSCULAR SYSTEM - POWER • Explosive muscle power declines faster with increasing age than isometric quadriceps strength • Community dwelling frequent fallers are less powerful in their lower limbs than non-fallers (Skelton 2002) – Fallers more asymmetrical in lower limb power than non fallers – Average fallers power/kg is below the threshold level to step confidently onto a 30cm step – Power more predictive of risk of falls than strength Specialist PSI Exercise Module But…the good news is… • Training can help reduce the ravages of age and sedentary behaviour….. Specialist PSI Exercise Module Effects of Training on balance and sensory inputs • Practice of specific functional movements and complex tasks = – dynamic balance – static balance – righting reflexes – proprioception – vestibular function – simple and complex reaction and movement times – visual function ? – body awareness – posture and gait Specialist PSI Exercise Module Effects of Training on the Endocrine System • Improves – circulation – intake of nutrients (calcium, vitamins and proteins) – cerebral function • Releases growth hormone – stimulates muscle and bone growth • Improves insulin sensitivity • Alters medication doses over time (insulin / thyroxine) • Decreased cortisol production in response to stress – strength-training Specialist PSI Exercise Module Effects of Training on Muscle • At any age – Neural improvements in first 12 weeks then muscle growth (Hypertrophy) so training has to be of >12 weeks duration to improve muscle size – strength (size of fibres, activation, increase in protein turnover, speed of contraction, relaxation time, agonist and antagonist coactivation etc) – power – posture and gait – blood supply – insulin sensitivity 0 3 6 9 12 15 Weeks Muscle strength Muscle size – neural control of movement Specialist PSI Exercise Module • In over 75’s three months of strength training rejuvenates up to 20 years worth of lost strength. (Skelton, 1994) Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module CARDIOVASCULAR SYSTEM • Main transport system – – – – – – Gases Food Waste Hormones Minerals Medications • Heart rate - controlled by autonomic nervous system Specialist PSI Exercise Module • Circulation –Pulmonary (to lungs) –Systemic (to body) –Coronary (to heart muscle) • Blood vessels “tubes” –Arteries - from heart to body –Veins - from the body to the heart –Capillaries - interchange of gases, food and waste Specialist PSI Exercise Module CONTRACTION OF HEART MUSCLE • Heart muscle contracts automatically – spontaneous discharge of pacemaker cells • Sino-atrial node - heart’s pacemaker located in right atrium. Impulses travel through atria to ventricles via A-V node. • Heart muscle cells are connected Specialist PSI Exercise Module CONTRACTION OF HEART • Parasympathetic activity slows the heart • vagus nerve releases Acetylcholine • Sympathetic activity quickens the heart • release of Adrenaline and neurotransmitters • Blood Pressure • cardiac output flowing into vascular system influences systolic pressure • resistance of blood vessels influences diastolic blood pressure Specialist PSI Exercise Module VOLUMES • Stroke Volume • Blood per beat • Cardiac Output • Blood per minute • Maximal O2 Uptake • Amount of oxygen that can be used in one minute – ml/kg/min Specialist PSI Exercise Module 40 Men % VO2 max 100 Maximal Oxygen Uptake (ml/kg.min) 75 Stair Climbing (slowly) Walking (3mph) 20 50 25 % VO2 max 100 Making the bed 75 Dressing 50 25 0 0 30 Age 80 Specialist PSI Exercise Module EFFECTS OF AGEING At rest no major changes to heart rate, stroke volume or cardiac output due to age alone BUT when the system is challenged then there are age-related deficits – compounded by sedentary behaviour • stiffness of heart wall (collagen) • Maximal H.R. • Maximal stroke volume • Maximal cardiac output • Maximal aerobic power – 10% per decade • systolic blood pressure • incidence of postural hypotension (failure of venous return) Specialist PSI Exercise Module Fallers vs Non-fallers • Cardiac symptoms can affect falls – – – – Syncope Arrythmias TIAs Postural Hypotension • Cardiac medications not a major risk except in combination with other medications (>4) Specialist PSI Exercise Module FUNCTIONAL CONSEQUENCES • Tasks will require % of maximum in older person • Unable to sustain submaximal activities • Postural hypotension can lead to blackout / drop attack / injury • Fartlek training approach • Circulation re-booster on major postural transitions Specialist PSI Exercise Module EFFECTS OF TRAINING • Increased time in Diastole ( heart health) • Maximal aerobic power can be by – Muscle oxidative enzymes – Muscle capillarisation – Stroke volume and cardiac output • Relative increases similar to young people • Everyday tasks require % of VO2 max • Everyday tasks can be performed for longer with greater ease • Hypertension and Postural Hypotension in some Specialist PSI Exercise Module PULMONARY SYSTEM • Main transport system for gases – Oxygen – Carbon Dioxide • Ventilation controlled by Nervous System – normally automatic (respiratory centres in brain stem) – some voluntary control (cortex overides respiratory centres) Specialist PSI Exercise Module Structure • • • • • Nasal passages Larynx Trachea Bronchi Bronchioles • Terminal Bronchioles • Alveolar Ducts • Alveoli • Gas exchange takes place rapidly in alveoli - large surface area surrounded by dense capillaries Specialist PSI Exercise Module VENTILATION Inspiration is active volume of thoracic cavity by contraction of intercostal muscles and diaphragm Expiration (at rest) is passive volume returned to resting values Specialist PSI Exercise Module LUNG VOLUMES Specialist PSI Exercise Module EFFECTS OF AGING • Stiffness of chest wall • Strength of respiratory muscles • Elastic recoil in lung • Residual dead space • Functional area of lung • Cartilaginous support • Thickening of mucosal lining • Sensitivity of respiratory centres Specialist PSI Exercise Module FUNCTIONAL CONSEQUENCES System still adequate for sub-maximal activity • Respiratory work • Oxygen costs of many activities • Breathlessness may reduce tolerance of exercise • maximal voluntary ventilation • mechanical efficiency of movement • posture Specialist PSI Exercise Module EFFECTS OF TRAINING • maximal voluntary ventilation • mechanical efficiency of movement • posture Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Joints Effects of Ageing - 1 • Dehydration (62% @ 25 yrs, 53% @ 75 yrs, synovial fluid less runny and fewer, larger villi) • Joint changes (85%, only 50% OA) • Number of cross links between collagen fibres • Length of life of collagen molecules • Visco-elastic properties (25-60 yrs 50%) • Disc compression ( length spine 3-4% @ 70 yrs) • Flexibility ( 25-30% @ spine, 50% @ hip) Specialist PSI Exercise Module Effects of Ageing - 2 • Calcification (cartilage tougher, more fibrous and brittle) • Hairline fractures • ROM (change in rebound energy exchanges during walking, tendon calcium in stretch phase) • Stride length • Single leg support • Cautious gait • Sway - wider stance, trunk and knee flexion • Efficiency of response to balance problems • Changes with physical inactivity Specialist PSI Exercise Module Joints in Osteoarthritis Specialist PSI Exercise Module Functional Consequences • Stiffness • Stability • Comfort • Ease of movement • Energy cost • Proprioception Specialist PSI Exercise Module Effects of Training • Length of life of collagen molecules • Viscoelastic properties • Regular/Lifetime maintain length in spine • Stride Length • Rhythm • Sway • Correction efficiency • Confidence in movement Specialist PSI Exercise Module BONE BASICS • Function • Structure • Architecture • Production • Maintenance • Ageing • Training Specialist PSI Exercise Module Trabecular or spongy bone Cortical or compact bone 4 Components Tough resilient collagen fibres More brittle mineral material Bone Marrow Bone cells + Blood vessels Specialist PSI Exercise Module BONE: ARCHITECTURE • Cylinders of compact bone - long bones • Varied symmetrical, contoured trabecular bone vertebrae and ends of long bones Comparison of fragile osteoporotic bone with strong, dense bone • Skeleton 1/10th body weight • Bone in constant turnover Strong, dense bone Fragile, osteoporotic bone Figure 3 Specialist PSI Exercise Module BONE: PRODUCTION • 10% renewed per annum • osteoclasts - resorption • osteoblasts - formation • osteocytes - bone monitors and signallers • peak bone mass 20-40 years • 40-45+ 0.5-1% per year • post menopause 1 > 6% per year Specialist PSI Exercise Module Main fracture sites: Spine Wrist Hip Change of fracture site with increasing age Specialist PSI Exercise Module BONE: RISK FACTORS • Genetics • Hormone levels •Anorexia •Overtraining •Endocrine disease • Bone loading activity • Calcium and Vitamin D Specialist PSI Exercise Module Risk Factors for Fracture • • • • • • • • • • Female Tall height Previous fracture or family history of fractures History of falling Poor self rated health Lack of weight gain since age 25 Early menopause Spending less than 4 hours a day on their feet Smoking, high caffeine intake, low calcium intake Nil childbearing Specialist PSI Exercise Module EFFECTS OF AGEING • oestrogen/progesterone/ testosterone Effect of age on bone mass • mineralisation • resilience of collagen density • renewal Bone Mass • bone density and bone mass • growth hormone 0 10 200 30 40 50 60 70 Age (years) • muscle mass Figure 4 • physical activity Specialist PSI Exercise Module Young healthy spine Osteoporotic spine Specialist PSI Exercise Module Specialist PSI Exercise Module Functional Consequences • Fracture risk • Pain • Disability and Discomfort • Exercise Cost • Postural Instability Fear, anxiety, loneliness • Physical Activity Confidence • Field of Vision • Integrity of the Spine Specialist PSI Exercise Module EFFECTS OF TRAINING Exercise can slow or reverse age related bone loss provided it is: •Weight resisted - weight training - impact - loading •Site specific - wrist, hip, spine •Peak Strain - hold the movement •Fast Strain - effective and brief •Error Rich - tennis, squash, fitness class Strategy = short periods of site specific, high strain rate in unusual relationships Specialist PSI Exercise Module High intensity strength training. 3 p=0.02 p=0.04 % Change in BMD 2 1 0 Exercise Control -1 -2 -3 Femur Spine -4 Nelson et al, 1994 Specialist PSI Exercise Module % Change Aerobic class with step and site specific impact in over 50s 2.5 2 1.5 1 0.5 0 -0.5 -1 -1.5 -2 o k c Ne f Exercise Control ur m Fe T r e t an h roc Welsh & Rutherford, 1996 Specialist PSI Exercise Module EFFECTS OF TRAINING ALSO • Bone strengthening + bone protection + fall prevention • Exercise + HRT = more beneficial • Exercise + calcium = more beneficial • Exercise + Vit D = more beneficial Specialist PSI Exercise Module Get Practical Bone Loading Workshop Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Fear of Falling and Motivation to Exercise Fear of Falling Stages of Behaviour Change Listening and Talking about exercise Specialist PSI Exercise Module Fear of Falling • Prevalance (Tinetti 1994) – 30-60% in people over age of 65 – 50-65% in previous fallers • Fear and lack of confidence in balance predict – Deterioration in physical functioning (Arfken 1994, Vellas 1997) – Decreases in physical activity, indoor and outdoor (Arfken 1994, Finch 1997) – Increase in fractures (Arfken 1994) – Admission to Institutional Care (Cumming 2000, Vellas 1997) Specialist PSI Exercise Module Adherence to exercise regimens • Fear of activity – avoidance of activity that might lead to a fall • High refusal to uptake exercise interventions to prevent falls – >50% common – Lord study (2002) • Invited 11,000 responded 1,967 (18%) • Low adherence once started – Lord study (2002) • Randomised 1107, 74% started, 60% attended >50% of sessions • But FaME (Skelton 2004) in frequent fallers • Randomised 50 • 100% started, 10% dropped out of classes • 79% Attended >75% of sessions Specialist PSI Exercise Module Increasing Motivation and Adherence – how ? 1. Assessing motivation towards physical activity 2. Helping to overcoming the barriers 3. Support strategies Specialist PSI Exercise Module Pre-exercise assessment • Health • Function • Readiness to exercise (Later Life Training Manual) How do we assess readiness to exercise among participants in PSI classes ? Specialist PSI Exercise Module Lifetime model of physical activity Specialist PSI Exercise Module Key questions to ask (exploring thoughts) • Importance question - I wonder how important being active is for you ? • General questions - What kinds of physical activity do you do at the moment ? • Benefits question - Imagine if you did more, what benefits would you expect to see ? • Barriers question - What things prevent you from being more active ? • Concerns question - What things worry you about being more active ? Specialist PSI Exercise Module Change is more likely when …. • Perceived benefits (of physical activity) outweigh the costs (decisional balance) • Leads to social approval (significant others) not disapproval • Consistent with highly valued, broader life goals (values and motives) • Outcomes are within one’s personal control (self efficacy) • There are few obstacles in the way (barriers) • Opportunities and access (to physical activity) are high (Sport England 2005) Specialist PSI Exercise Module Evidence about strength and balance classes - the barriers • Health problems (actual and perceived interference) • No observed positive effects when tried programme • Not liking social contacts in classes (peers or leader!) • Unpleasant experiences (fatigue, pain etc.) or not enjoyable • Low motivation or perceived relevance • Other priorities (caring for dependents, holidays, other appointments, housework) (Yardley et al 2005a) Specialist PSI Exercise Module Perceived positive factors and benefits • Noticeable benefit/improvement (restoring/maintaining fitness and functioning, better health –blood pressure, dizziness, diabetes) • Feel and look good (less stiff, less pain, more mobile, strong, energetic, better balance, mood, weight loss) • Able to do more things (walk, do without stick, climb stairs, travel, go out alone, go shopping, ADLs) • Maintaining and increasing independence • Social contact (bond formed through prolonged contact with group) • Confidence/pride in achievement (general increase in self- Specialist PSI Exercise Module motives for older people to take up strength and balance training • thinking you are the kind of person who should do these activities (self-efficacy) • thinking other people think you should do these exercises (peers, family, partners) • believing that these activities would be enjoyable • concern about the risk of a future fall • (NOT having recent falls, or risk factors for falls) (Yardley et al 2005a) Specialist PSI Exercise Module Don’t mention the F-word! Understanding older people’s views of falls prevention advice (Yardley et al. 2005,2006) Communication / Motivation important in encouraging uptake and adherence to falls prevention interventions and the pre-exercise assessment is an ideal place to discuss their attitudes / barriers / motivators Specialist PSI Exercise Module Increasing engagement with exercise ? 60 people attending A & E as a result of a fall. When offered choice on an intervention to prevent a future fall • 72% reluctant to take up exercise programme • 28% reluctant to take osteoporosis medication But when asked if likely to take up an intervention to prevent a worsening health state • 63% said they would take up exercise! • 93% would take osteoporosis medication (Whitehead 2006) Specialist PSI Exercise Module During assessment and intervention.. To encourage people to exercise: • Emphasise immediate benefits for them (rather than reduction of risk) • Promote positive social image (rather than simply rational advantages) • Ensure patients have positive but realistic expectations • Use psychological techniques to encourage adherence (monitoring and reinforcement, modelling, explicit commitment etc.) • Ensure early experiences of sessions arerecommendations, positive ProFaNE Yardley (through graded goal setting, social reinforcement etc.) 2007 Specialist PSI Exercise Module Engaging older people in preventative health care • Raise awareness in the general population that undertaking specific physical activities has the potential to improve balance and prevent falls. • When offering or publicising interventions, promote benefits which fit with a positive self-identity. • Utilise a variety of forms of social encouragement to engage older people in interventions. • Ensure the intervention is designed to meet the needs, preferences and capabilities of the individual • Encourage self-management rather than dependence on professionals by giving older people an active role • Draw on validated methods for promoting and assessing the processes that maintain adherence, especially in the longer-term. Yardley et al (2005) Specialist PSI Exercise Module Support strategies • All literature provides strong evidence that they are effective (NICE, HDA, CDC, Campbell, FAME) • Communication strategies - follow up using technologies, phone, diaries, email • Social support activities (events and buddies) • Educational programmes Which are the “best buys” and why ? Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Detection and Assessment: Theory and Guidelines - Finding fallers…in different settings: - Pre-exercise assessment - Health, Function and Motivation - Ongoing assessment - Triggers for referral to medical setting - Triggers for referral between exercise settings Specialist PSI Exercise Module Targeting Intervention Identify high risk from a general population Identify what more in depth assessment is required Identify modifiable risk factors for each individual Target Intervention Specialist PSI Exercise Module NICE Falls CG: “Safety net” service model Specialist PSI Exercise Module NICE Falls CG: specialist integrated service model Specialist PSI Exercise Module What tool or test ? It needs to be: Reliable same result in same person over short intervals of time Consistent same result whoever assesses Valid for the age and functional capacity of the individual • Plus functional and understandable to the older person Specialist PSI Exercise Module The role of pre-exercise assessment • Assessment – is the cornerstone of rehabilitation – identifies health status (safety and warning signs) – identifies areas of limitation (pre-exercise) – influences subsequent treatment/intervention (tailoring) – gauges efficacy of treatment (ongoing) Specialist PSI Exercise Module Pre-exercise Assessment • Assessment should be: – what they can do and build upon …..NOT. …. what they cannot do – an education tool (fitness vs health symptoms) – relevant (age, medical condition and functional capacity of the participant) Specialist PSI Exercise Module TRIGGERS Referral back to Rehab Exercise Setting • Onto therapy setting (or stay within chair-based setting) – – – – – cannot stand for more than 30 seconds without excessive sway cannot transfer weight from one leg to another without concern cannot take a step backwards unassisted chronic or acute pain on walking marked deformities, severe asymmetry, marked weakness Functional Grid • ticks mainly 6’s Specialist PSI Exercise Module Ongoing Assessment • ? Every 3 / 6 / 9 months or if participants health or functional condition deteriorates • Essential for – updating health or functional status information – assessing effectiveness of programming – comparing goals with actual gains – improving motivation • Continually assess – environment and safety – ‘appearance’ of participants – correct intensity (Borg) Specialist PSI Exercise Module TRIGGERS Ongoing assessment - 1 • Sudden onset of symptoms of illness – Dizziness, inner ear infections, excessive tiredness, weight loss, loss of appetite or shortness of breath, anxiety, unidentified or uncontrolled pain • Worsening of existing medical condition – Frequency of transient ischaemic attacks increases, swelling of an OA knee following the session or a longer than usual walk • Onset of dizziness with current or new medications or concerns about whether correct pills are being taken at the correct time or dose • Sudden onset of pain in joints – Osteoarthritis of the knee, swollen joints, limping Specialist PSI Exercise Module TRIGGERS Ongoing assessment - 2 • Deterioration of functional capacity or balance – Now needs walking aid, progressive difficulty with walking on the flat, fatigues more quickly, transfers becoming difficult • Increase in frequency of falls or increase in injury due to falls – Starts to fall at home in repeat areas of the house or doing certain tasks, can no longer rise from the floor, injuries not healing properly, arrives with a black eye and has not been to see the GP after the last fall yet • Distinct changes in vision – Depth perception, missing steps, light-headedness on walking downstairs with bifocals • Distinct changes in hearing – Wax removal, inner ear infection Specialist PSI Exercise Module The value of assessment • You get to know your participants • Good time to discuss exercise history, likes, dislikes and perceptions of exercise and of falling • You’re safe and so are they • You know where to start and where to adapt • You know if you are getting it right • Funder’s know you are getting it right • Participants feel informed Specialist PSI Exercise Module Case Study Guidelines • Find a person at risk of falls or with a falls history that would be able to join a PSI led class • Perform functional assessments and do the health / QoL / fear of falling questionnaires with them • Write up – 1500 words • Include tailor / adapt the FaME phases of training for that individual • Present the written case study on Day 6/7 • See Case Study Guidelines in your pack Specialist PSI Exercise Module Practical / Case Study Guidelines • Pre-exercise Assessment – – – – – – – – Readiness to exercise Health Falls Risk (FRAT) Fracture Risk (Black) Fear of Falling (FES-I ) Confidence in Maintaining Balance (ConFBal) Health outcome (EQ-5D) Functional Assessments - GRID Specialist PSI Exercise Module Selection Criteria -Is your participant at risk of falls? Each individual should have one or more of the following: • Fear of falling • Feeling unstable (balance problems) • History of falls (injury or not) • Low bone density (and/or family history of osteoporotic fracture) Specialist PSI Exercise Module Readiness to Exercise • Stage of Health Behaviour Change – – – – – – Considering Preparing Currently Active <6 Months Regularly Active >6 Months Relapse Unknown • Gauge from a conversation with them about exercise history and current participation Specialist PSI Exercise Module Health Assessment Referred or self-referred • Health status must be checked with / acknowledged by participants GP • Complete a health questionnaire with them that will identify their medical conditions and medications • Use to ensure your know if someone has any conditions which are contraindicated and need specific feedback from GP before they can continue in the class • A health questionnaire is in your case study pack but when you qualify you may use one that has been developed by your service. Specialist PSI Exercise Module Contraindications to the ‘Prehab’ Class People with the following: • Uncontrolled angina • Uncontrolled resting BP > 180/100 mmHg Significant drop in BP during exercise Uncontrolled tachycardia > 100 bpm Unstable or acute heart failure Uncontrolled acute systemic illness • • • • • • • • • Uncontrolled visual or vestibular problems Unable to maintain seated upright position Recent injurious fall without attention Impaired cognition Place others and themselves at risk should not take part until their GP advises that their condition permits safe participation Specialist PSI Exercise Module History of Fall • Number in last 6 months • Last one – – – – – – – – Location Time Doing what? Reason? Loss of consciousness? Or dizziness prior? Any injury? Could they get up again? Did they see GP or go to Hospital? Specialist PSI Exercise Module FRAT – Falls Risk Assessment Tool Multi - professional guidance for use by the primary health care team, hospital staff, and social care workers Is there a history of any fall in the previous year? How assessed? Ask the person. Is the patient / client on four or more medications per day? How assessed? Identify number of prescribed medications. Does the patient / client have a diagnosis of stroke or Parkinson's Disease? How assessed? Ask the person. Does the patient / client report any problems with their balance? How assessed? Ask the person. Is the patient/client unable to rise from a chair of knee height? How assessed? Ask the person to stand up from a chair of knee height without using their arms. Specialist PSI Exercise Module Risk of Fracture Tool • Black 2001 – High risk Score 7-10 – Moderate risk Score 5-6 – To use in your case study Specialist PSI Exercise Module Fear of Falling Scale – FES-I • Long Version – 16 Qs – Yardley et al. 2006 • Short Version – 7 Qs – Kempen et al. 2008 – To be used for your case study – Scoring • 7 (no concern about falling) to • 28 (severe concern about falling). ProFaNE recommended Specialist PSI Exercise Module Confidence in Maintaining Balance • Simpson et al. 2004 • 10 Qs • Scoring – 10 confident – 30 unconfident • Use for your case study Specialist PSI Exercise Module EQ-5D – heath outcome measure • Page 1 So this would score as: 1,2,3,4,5 Specialist PSI Exercise Module EQ-5D • Page 2 Specialist PSI Exercise Module Functional assessment Seated shoulder external rotation flexibility Denote L and R arm in box(es) Seated shoulder internal rotation flexibility Denote L and R arm in box(es) Seated hamstring flexibility Denote L and R arm in box(es) 180 degree turn Number of steps: ______ Functional Reach Use of walking aid? Cm:____ Timed Up and Go Use of walking aid? Time (seconds):_____ No Limitation Can reach over their shoulder to between their shoulder blades 1 Can reach to behind the back to touch their shoulder blades 1 Able to reach to midcalf of the extended leg 1 Able to turn safely in 4 steps or less 1 Reaches greater than 35 cm 1 Able to rise from the chair easily, walk unaided, turn without dizziness or stumbling. Faster than 8 seconds 1 Severe Limitation Can reach to the back of the neck 2 Can reach to behind the back to touch just below the shoulder blades 2 Able to reach just past knee of the extended leg 2 Able to turn safely in 6 steps or less 2 Reaches between 25 and 34 cm 2 Able to rise from the chair without arms, walk unaided, turn without stumbling. Between 9 and 15 seconds 2 Can reach behind the head to level of ears 3 L Can reach behind to mid-back level 3 L Able to reach to knee of the extended leg 3 Able to turn safely in 8 steps or less 3 Reaches between 16 and 24 cm 3 Difficulty on rising from chair, walks aided or unaided but takes between 16 and 24 seconds 3 Can reach the top of their head 4 R Can reach behind to waist level 4 R Able to reach to mid thigh of the extended leg 4 Needs close supervision and verbal cueing for safety. Takes 912 steps 4 Reaches between 10 and 15 cm 4 Difficulty on rising from chair, walks aided or unaided but takes between 25 and 40 seconds 4 Can reach above shoulder level but not touch the top of their head Unable Unable to reach above shoulder level without pain or movement limitation 5 6 Can reach behind to buttock level Unable to reach behind their back, pain or movement limitation 5 6 Able to reach to knee but unable to complete with correct technique 5 LR Needs assistance from one person or furniture to turn 5 Reaches less than 10 cm 5 Difficulty on rising from chair, needs walking aid, unconfident or dizzy on turning - or takes over 40 seconds 5 Unable to reach forward because of pain, deformity or fear of falling 6 Needs assistance from two people to turn 6 Unable or afraid to reach forward 6 Unable to rise from the chair, walk or turn without help 6 Specialist PSI Exercise Module FLOW DIAGRAM FOR PROSPECTIVE PARTICIPANTS IN EXERCISE SESSIONS TO IMPROVE POSTURAL STABILITY AND REDUCE FALLS AND INJURIES Referrer Selection Criteria Functional Assessment Grid Exercise Groups Mostly ticks SELF – REFERRED 1 2 DYNAMIC ‘PREHAB’ PSI 3 4 GP – PRIMARY CARE Those meeting inclusion criteria and having no exclusion criteria 5 6 PHYSIOTHERAPY REHABILITATION SETTING CHAIR – BASED (maybe PSI led or chair adaptations) P R O G E S S W I T H T I M E ‘REHAB’ – THERAPY (one to one or small group) Specialist PSI Exercise Module Final thoughts on case study • You need to tailor the phases of the FaME programme to your participants abilities – – – – Any limitations (adaptations) Any confidence issues (buddying) Are they particularly good at anything (so can progress faster) Asymmetry (homework) • In your judgement would they progress through any of the phases faster/slower? • Consider the main points of this individual you would want a cover teacher to know? – Medications – Limitations Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module DAYS 3 & 4 – OVERVIEW • Programming, Theory and Practice I and II • Teaching Practice Workshop • Assessment Briefing • Medical Conditions, Medications and Exercise Management • Health and Safety • Progression and Adaptation Workshop • Implementation in Community Programmes Specialist PSI Exercise Module PROGRAMMING THEORY & PRACTICE • AIMS - Making the case for PSIs - Types of exercise sessions in falls exercise provision - FaME - Exercise programming theory - Applying theory to practice - Practical Manual 2 Section 3 Specialist PSI Exercise Module Making the case for PSIs 4 Types of Opportunities, Phase IV: • PSI • Exercise for the Older Person • 1 to 1 Personal Training / Physiotherapist • Active Lifestyle 4 Advantages 4 Drawbacks Specialist PSI Exercise Module Types of exercise sessions in falls exercise provision: 3 Settings, 3 Session Structures • Rehab PSI Approaches Phase 3 • Prehab PSI Phase IV • Chair “Holding Group” Functional Strength 3 Common 3 Distinct Activities Activities (one per session) Manual 2 Section 3 Specialist PSI Exercise Module FaME PHASES 1. 2. 3. Phase names and corresponding weeks Content of each phase Manual 2 Section 3 Your practical assessment is week 15 – 20 (training gains / phase 2) – See Manual 2 Section 3 for session planner Specialist PSI Exercise Module SAFETY FIRST PSI Session Structure + Content Warm Up CIRCULATION BOOST; JOINT MOBILITY; STRETCH Workout 5 (of 7) EVIDENCE-BASED ACTIVITIES Cool Down CIRCULATION LOWERER; FLEXIBILITY; TAI CHI Tea + Chat and re-energise Manual 2 Section 3 Specialist PSI Exercise Module EXERCISE PROGRAMMING THEORY • Principles Specificity Progressive Overload Rest & Recovery Individual Difference • Variables (recap) FITTA Manual 2 Section 3 Specialist PSI Exercise Module PSI = EXERCISE for OLDER PEOPLE – Best Practice Guidelines + SPECIAL CONSIDERATIONS for Older People with HIGH RISK OF FALLS – Best Practice Guidelines Manual 2 Section 3 Specialist PSI Exercise Module EXERCISE GUIDELINES COMPONENTS OF FITNESS WORKSHOP BALANCE: STRENGTH: FLEXIBILITY: ENDURANCE What is it ? Older Person Guidelines Special Considerations For Fallers Examples of exercises F Definition I Only 3 please! T T A Specialist PSI Exercise Module STRENGTH Older Person Guidelines What is it ? Working F Resistance I 12 –15 reps to begin 1 – 3 sets progress up to 70-80% 1RM 6-8 reps Postural and bone-load for back extensors T 20 mins –1hr 6-9 secs per Isotonic Rep 5 Secs Isometric Specific Targeted Muscles: Hip, Knee, Ankle T Body weight / Weights Open/closed chain Isometric / isotonic To Gain Stronger Muscles And Bones To Make Everyday Activities Examples of Exercises 2 – 3 Times / week Functional abdominal work Muscle + Bones Against Special Considerations for fallers FaME: seated leg press, seated upper back strengthener, prone back extension Otago: standing knee flexion, standing hip abduction Easier Fun / Relaxed A Variety Safe Warm Social Manual 2 Specialist PSI Exercise Module The Borg Scale Rate of perceived exertion 0 0.5 NOTHING AT ALL VERY VERY LIGHT NB. 1 VERY LIGHT 2 FAIRLY LIGHT 3 MODERATE 4 FAIRLY HARD Evaluation 0 – 10 scale in Dynamic Endurance Component 5 HARD Research 6 – 20 scale 6 7 VERY HARD 8 VERY TIRING Community Session Endurance Component before mid point + post 9 10 VERY VERY HARD Manual 2 Section 3 EXHAUSTING Specialist PSI Exercise Module Resistance Training Continuum Endurance 15 Strength 12 10 8 6 30% 50% >60% >70% of IRM of IRM of IRM of IRM Low weight High Reps >80% of IRM Heavy weight Low Reps Manual 2 Section 3 Specialist PSI Exercise Module ENDURANCE Older Person Guidelines What is it ? Stamina: Work muscles harder & longer (in order to increase the pulse rate, breathing rate) F I Special Considerations for fallers Marching 3 – 5 days per wk - Focus on coordination and balance Moderate, 30-75 % VO2 Max Examples of Exercises - Chair based initially then chair support Side-stepping Gait training Toe taps - Simple / repetitive / stable T 30 – 60 mins. T Aerobic Fartlek A Longer build up and build down Avoid steps that could cause a trip Manual 2 Section 3 Specialist PSI Exercise Module BALANCE What is it ? Maintaining upright posture during position change (eg. Standing up and to prevent falls) Older Person Guidelines F 3 x per week Special Considerations for fallers Start with ‘win win’ tasks (eg – seated ball games) Examples of Exercises Functional reach while sitting Toe & heel walking I T T Increase slowly – graded to group 10 mins – building up to 1 hour. Ensure appropriate ratio of supervision for each task Explain benefits Method of using support Tandem walks calf raises Flamingo swings Picking objects off the floor Dynamic balance i.e weight transference Backward walking . A Varying activities & weaning off support slowly – vary positions Manual 2 Section 3 Specialist PSI Exercise Module FLEXIBILITY What is it ? Best optimal range of movement available at a joint or joints Older Person Guidelines F I Special Considerations for fallers Examples of exercises 2 – 7 days a week Mild muscular tension No Pain T Maintenance: 1 x 8 – 10 secs Developmental: 2-3 x 11-40 secs T Static and active Developmental + Maintenance A “Reward” Relaxing Remain seated 2 – 3 mins following work (stretches) in lying Targeted stretches Alignment is paramount Tai Chi Precise instructions – step by step Functional Activities Yoga Manual 2 Section 3 Specialist PSI Exercise Module BACKWARD CHAINING FLOOR WORK • Strength • Balance / Co – ordination • Flexibility • Coping strategies TAI CHI Manual 3 Specialist PSI Exercise Module EDUCATION and PREPARATION OF PARTICIPANTS INDUCTION SESSION WHEN EXERCISE SHOULD Manual 2 - NOT HAPPEN Manual 2 - BE DISCONTINUED - BE CONTINUED FALLS SPECIFIC EDUCATION / COPING STRATEGY MONITORING Manual 2 BORG, TALK TEST, observing co-ordination & technique = comfortably challenged Manual 2 Specialist PSI Exercise Module How To Avoid Spending A Long Time On The Floor After A Fall FALL OVER Remain still. Avoid panic and wasting energy on ineffective struggling. NO Have any serious injury? Any movements limited? Any pain? Will help arrive soon and this person will summon help or use a lifting cushion Can you get up without help? NO OK YES NO YES YES OK Plan how to summon help OK YES If you are wearing an alarm button or you can reach one – then do so! NO Simpson J. 1998 Manual 2 Carry out your previously worked out plan to summon help by alternative methods and while waiting for help to arrive carry out your plan to avoid any consequences of being on the floor for a long time. Specialist PSI Exercise Module PROGRESSION + ADAPTATION • Seated Adaptations for: – Trunk rotation, calf stretch, upward side stretch – Double side step, wide-based sway, march – Heel raise and toe walk, toe raise and heel walk, flamingo swing, tandem stand – Backward chaining – Prone back extension, side lying leg raise, prone hip extension – Working the oar Specialist PSI Exercise Module Exercise Management of Patients with Chronic Illness / Conditions STEP 1 The Individual Difference Principle • Liaison with Health Professionals • Liaison with Patient • Liaison with Leisure Professionals Manual 1 Specialist PSI Exercise Module Exercise Management of Patients with Chronic Illness / Conditions STEP 2 • • • • • • • • • • • Type of condition Site of condition Stage of condition Functional Limitations Disease Specific Effects Disease Specific Effects to the individual Medication Effects Exercise performance limitations Risk stratification Prognosis SMART goals – Specific; Measurable; Agreed; Realistic; Timed N.B. SMART - Not in manual / not assessed but an important tool. Specialist PSI Exercise Module DISEASE Do’s Don’ts Adapts Benefits FREQUENCY (How Often) INTENSITY (How Hard) TIME (How Long) TYPE (+ Activities) ‘Which type’ eg Strength / Endurance Isometric / Isotonic Continuous/Interval APPROACH/ ADHERENCE (Variety, Individual interests etc) Specialist PSI Exercise Module HEALTH & SAFETY 1. The Environment / Facility 2. The Equipment 3. The People Specialist PSI Exercise Module ASSESSMENT INSTRUCTIONS Formative Assessment of Tai Chi: On Day 5 (afternoon) you will have your teaching skills for delivering the Tai Chi section of a class formatively assessed. 1. THEORY PAPER • ON DAY 5 • 2 Hours • 5 short answer questions and 30 multiple choice • 70% pass mark • 5 mins reading time • Let us know before if special needs requiring additional support Specialist PSI Exercise Module TIPS for Theory Paper • LEARN YOUR PPTs! • In the Manual • If its in bold its important • If its in a box its VERY IMPORTANT • If its in a box + bold its VERY IMPORTANT Specialist PSI Exercise Module ASSESSMENT INSTRUCTIONS 2. PRACTICAL • On Day 6 or 7 (whichever you signed up for) • Plan 1 hour week 15-20 PSI Session – bring 2 copies of plan - ie. assessed on planning Refer to Manual 2 Session Planner; Use sesson plan proformas provided; Only teaching points necessary ie. not instructions • Approx 30 mins teaching to your peers – ie. assessed on teaching Equipment provided = therabands, chairs, mats; Moved on by assessor – plenty of time / prompts; Assessment checklist will be used by assessor; Consider lifting technique e.g. for mats. Chair alternatives but Not Chair focus; Notes can be used if necessary – or assessor prompt Specialist PSI Exercise Module ASSESSMENT INSTRUCTIONS 2. PRACTICAL cont’d • No Pass Mark for Practical delivery, only Pass/Refer and action points given • Receive peer evaluation • Write up self- evaluation – ie. assessed on evaluation Practice with people - not just in front room! Specialist PSI Exercise Module ASSESSMENT INSTRUCTIONS 3. CASE STUDY Ensure meets Criteria for PSI intervention and is at risk of falls • Complete all paperwork - (questionnaires + functional grid) in assessment pack • Complete 1500 word ‘write up’ – see case study guidelines in Summative Assessment Pack • Submit on day 6/7 • Pass mark 70% All results (case study, practical and theory paper) in post (8-10 weeks later) Specialist PSI Exercise Module PSI Workshop Warm Up 1. Circulation Exercise 2. Mobility 3. Stretch Workout 5. Dynamic Endurance 6. Dynamic Balance 7. Resistance Bands 8. Backward Chaining 9. Floorwork Cool Down 10. Circulation Lowerer 11. Flexibility 12. Tai Chi Specialist PSI Exercise Module Teaching Workshop Feedback Guidelines pace Appropriate to component and evidence-based transitions 1. Content 2. Teaching What Where When - Position - T. Instruction - T. Points How - 1 - 1 observing analysing, solution, communicating 3. Personal Performance - Attire, Organised, Technique, Voice, Communication Specialist PSI Exercise Module Medical Conditions and Medications Impacting on Falls, Injury and Capacity to Exercise With thanks to Dr Rob Morris (contributions also by Drs J Close, J Treml, A Carr and S Shah) Specialist PSI Exercise Module Introduction Why bother with this? Medical conditions (diseases and disorders), and the medications used to treat them, both have potential influence on postural stability and the capacity to exercise effectively Older People: More diseases/conditions – accumulated deficits More susceptible to drug toxicity (side effects) More disease = More drugs + More types of drugs = Greater potential for falling Specialist PSI Exercise Module Question • Identify any condition common among older people Consider: – Does it increase risk of falls and why – Does it limit exercise capacity – Risks and Benefits of Exercise Specialist PSI Exercise Module Contents Part 1 – Medical Conditions Cardiovascular disease Ischaemic heart disease Peripheral vascular disease Cerebrovascular disease - Stroke Hypertension Arrhythmias Heart Failure Respiratory disease Asthma Chronic Obstructive Pulmonary Disease Brain disease Parkinsonism and Parkinson’s disease Depression Dementia Specialist PSI Exercise Module Musculoskeletal Disorders Osteoarthritis Rheumatoid arthritis Endocrine and Metabolic Disorders Diabetes Osteoporosis Sensory system abnormalities & Nervous System Integration Cataracts Glaucoma Age-related macular degeneration Ménières disease Specialist PSI Exercise Module Part 2 – Medications (drugs) • Drugs for high blood pressure (Antihypertensives) • Drugs used in angina • Drugs used to reduce clots (Antiplatelet drugs & anticoagulants) • Drugs for abnormal heart rhythms (Antiarrhythmic drugs) • Drugs used in respiratory disease • Drugs for Parkinson’s disease • Drugs acting on the brain (Psychotropic drugs) • Drugs for arthritis and connective tissue disorders • Drugs for diabetes • Drugs for osteoporosis Specialist PSI Exercise Module Cardiovascular Disease Specialist PSI Exercise Module Ischaemic Heart Disease Definition Impairment of blood flow to heart muscle caused by narrowing of coronary arteries Symptoms Chest pain/tightness on exertion and relieved by rest – angina (pectoris) Concern Can ultimately lead to heart attack – myocardial infarction Management Medication or invasive procedures, including angioplasty (balloon dilatation), stent & coronary artery bypass grafting (CABG) Relevance for exercise Should always consult with GP prior to exercise program Specialist PSI Exercise Module Angioplasty Specialist PSI Exercise Module Coronary Artery Bypass Surgery Specialist PSI Exercise Module Peripheral Vascular Disease Definition Impairment of blood flow to the peripheries (legs mainly) caused by narrowing of blood vessels Symptoms Cramp like pain in legs on exertion, relieved by rest Concern May deter people from exercising. Often co-existent with ischaemic heart disease (which may be silent) Management Angioplasty (balloon dilatation) or stent, if narrowing is in larger blood vessels, or bypass surgery Relevance for exercise Will limit exercise capacity. Need to encourage to work into, but not through, pain (which may lead to opening of collateral vessels) Specialist PSI Exercise Module Stroke Definition Damage to part of the brain from either blockage to a blood vessel or bleeding from a blood vessel (15%) Symptoms Depends on area damaged in brain - Face, Arm, Leg, Speech, Vision Concern Increased risk of falls: may also affect comprehension or speech Management Thrombolysis, rehabilitation, and address risk factors for recurrent stroke. Occasionally carotid artery angioplasty Relevance for exercise Increased risk of falls due to weakness, impaired co-ordination of movement, loss of visual field, sensory neglect or confusion. Nonetheless have potential to benefit from exercise. Need to be aware of language, memory or sensory problems. Specialist PSI Exercise Module Stroke – CT Scan Specialist PSI Exercise Module Carotid Artery Angioplasty Before After Specialist PSI Exercise Module Hypertension Definition High blood pressure Systolic pressure > 140 and/or Diastolic pressure > 80mmHg Symptoms Usually no symptoms Concern Increased risk of stroke or heart attack Management Usually controlled on medication long term, also diet and exercise Relevance for exercise Not an exclusion for exercise. Some studies have shown that exercise lowers BP (Tai Chi). Client responsibility to ensure BP is checked regularly and liaise with GP Specialist PSI Exercise Module Arrhythmias Definition Abnormalities of the heart rhythm Symptoms Palpitations, dizzy spells (rare), collapse. May be asymptomatic. Determined by site in heart where disturbance originates. Concern Risk of exercise inducing abnormal rhythm Management Once type of rhythm disturbance is identified, then medication is usual treatment Relevance for exercise Be aware of any precipitating factors Client responsibility to liaise with GP Specialist PSI Exercise Module Heart Failure Definition A complex syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the heart to function as a pump to support a physiological circulation Symptoms Severe tiredness, breathlessness or swelling of the ankles and feet Concern Development of heart failure is associated with poor prognosis but careful exercise can improve heart function and symptoms Management Dependent upon cause. Drugs form the mainstay of management in most cases. Relevance for exercise Depending on severity may limit exercise capacity significantly Specialist PSI Exercise Module Pacemakers and Defibrillators Definition Pacemakers are electrical implants used to treat certain disorders of cardiac rhythm, usually where the heart goes too slowly. Defibrillators are implanted to treat more serious rhythm disorders, particularly paroxysmal ventricular tachycardia or fibrillation. Symptoms Usually the presence of a pacemaker or defibrillator is asymptomatic Concern Patients with exercise-induced arrhythmias may find that their defibrillator is triggered. Pacemakers should not be a concern. Relevance for exercise Pacemakers should not preclude exercise, though clients should check with their GP or pacing clinic. Should not exercise within 6 weeks of a new pacemaker. Clients with defibrillators must check with their specialist clinic and should avoid exercising to maximum heart rate. More sustained, lower intensity exercise is preferable. Specialist PSI Exercise Module Respiratory Diseases Specialist PSI Exercise Module Asthma Definition Reversible airflow limitation due to constriction of airways Symptoms Shortness of breath, wheeze, cough Concern Can be induced by exercise or limit exercise capacity Management Inhaled medication for the majority Some will take oral medications Relevance for exercise Not a contra-indication to exercise but may limit exercise capacity. Clients should bring inhalers with them and use at beginning of session Specialist PSI Exercise Module Airways in Asthma Specialist PSI Exercise Module COPD/Emphysema Definition Irreversible airflow limitation usually caused by smoking Symptoms Shortness of breath on exertion Concern Reduced exercise capacity Management Similar to that of asthma although less responsive Relevance for exercise Can limit exercise capacity, but exercise may improve this. Specialist PSI Exercise Module Case Study 1 • 74 year old male with history of COPD and a myocardial infarction 6 months ago – What is the likely causal link between the two conditions? – What are the benefits of physical activity for this patient? – What may limit his activity? Specialist PSI Exercise Module Brain Diseases Specialist PSI Exercise Module Parkinson’s Disease Definition Deficiency of neurotransmitter dopamine in the brain Symptoms Resting tremor, bradykinesia (slowness of movement), rigidity, postural instability, shuffling gait and reduced facial expression Concern Increased risk of falls Management Managed with drugs. Rarely surgery Relevance for exercise Likely to be slow to initiate movement and exhibit postural instability May be embarrassed No specific exercise programme has proven benefit Specialist PSI Exercise Module Definition Low mood Depression Symptoms Sad, low self-esteem, loss of appetite, weight loss, concentration and memory problems, sleep problems, anxiety, somatic symptoms etc. Concern Increased risk of falls, may be increased fear of falling Management Medication or psychology Relevance for exercise Postural instability, due to deconditioning or drugs Participation may be poor and will need encouragement etc. Specialist PSI Exercise Module Dementia Definition Progressive decline in cognitive ability and other brain functions. Alzheimer’s disease is commonest cause, followed by vascular disease Symptoms Impairment in short term memory, alteration in ability to sequence tasks, disorientation, reduced risk-awareness, ?impaired balance Concern Increased risk of falls Management Depends on cause but largely supportive, drugs of limited benefit Relevance for exercise May have difficulty following commands May get agitated or disorientated Some can benefit from supervised exercise May be better to have carer present Specialist PSI Exercise Module Osteoarthritis Definition Degeneration of joints with loss of cartilage. Affects most commonly used joints knees, hips, lower back, shoulders and hands Symptoms Pain, stiffness and swelling of joints. Instability of knees. Reduced mobility. Concern Pain in joints may be worsened by exercise. Unstable knees can give way. Management Analgesia is mainstay of management. Consideration of joint replacement. Strength training has proven benefit - may protect joint from excess wear. Relevance for exercise Will limit exercise tolerance through affected joint. This may be helped by taking analgesia prior to exercising. Specialist PSI Exercise Module Rheumatoid Arthritis Definition Inflammatory disorder of joint lining and tendon sheath lining Symptoms May be similar to OA, but different joints affected - hands, wrists, neck Inflammatory changes and swelling more common, especially in the morning Concern As with OA. Joints need protection when acutely inflamed Management Usually controlled with variety of analgesic agents and disease modifying drugs. Sometimes joint replacement. Relevance for exercise Ensure adequate analgesia, may be less stiff in afternoon Specialist PSI Exercise Module Joints in Rheumatoid Arthritis Specialist PSI Exercise Module Diabetes Definition Impaired production of, or reduced sensitivity to, insulin causing high blood sugar. Associated with abnormal lipids, high BP, obesity. Symptoms Weight loss, thirst, passing a lot of urine, blurred vision Concern Hypoglycaemia if prolonged fast or excessive exercise (only if treated with tablets or insulin) Management Can be managed with diet, oral tablets and/or insulin Relevance for exercise Peripheral neuropathy causes impaired foot sensation, altering balance Should carry dextrose tablets for classes Exercise training has proven benefit in reducing blood sugar Specialist PSI Exercise Module Osteoporosis Definition Progressive loss of bone (all bones) and disruption of bone architecture leading to a weak & fragile skeleton that is prone to fractures - particularly spine, hip & wrist. Symptoms Low trauma fractures Concern Risk of injury from fall. Pain Management Usually treated with drugs, including calcium and vitamin D Relevance for exercise Increased risk of fracture in the event of a fall Weight-bearing exercise may increase bone density Might be a group to consider for hip protectors??? Specialist PSI Exercise Module Nervous System Integration Specialist PSI Exercise Module Nervous System Integration Vestibular system Balance Brain stem Basal Ganglia Movement control Spinal cord Relay of signals Cerebrum Cerebellum Coordination Autonomic Nervous System Pulse, BP control Peripheral nerves Motor - muscles Sensory - skin sensation - proprioception Specialist PSI Exercise Module Nervous System Integration Vision Vestibular Pain/Temperature Proprioception/Vibration Pressure Light touch Motor Autonomic Blood pressure Heart rate Specialist PSI Exercise Module Nervous System Integration Diseases affecting sensory input Vision Age-related refractive error (long sight) Age-related macular degeneration Glaucoma Cataracts Stroke causing visual field defect Proprioception Diabetic neuropathy Vitamin B12 deficiency (uncommon) Syphilis (very rare) Degenerative joint disease, especially of neck and ankles Vestibular Age-related middle and inner ear changes Chronic ear infections Perforated ear drum? Labyrinthitis Benign paroxysmal positional vertigo Specialist PSI Exercise Module Nervous System Integration Diseases affecting central processing Cerebrum Cerebrovascular disease (stroke, small vessel disease) Dementia Brain tumour (benign & malignant) Cerebellum Cerebrovascular disease (stroke) Long term alcohol misuse Basal ganglia Cerebrovascular disease (stroke) Parkinson’s disease and related conditions Brain stem Cerebrovascular disease (stroke) Atherosclerosis (narrowing of blood vessels supplying the brain) Postural hypotension Specialist PSI Exercise Module Nervous System Integration Diseases affecting Effector response Spinal cord and nerves Any condition causing narrowing of spinal cord Neuropathy Motor neurone disease Multiple sclerosis Foot drop (common peroneal nerve palsy) Muscles Cerebrovascular disease (stroke) Motor neurone disease Muscular dystrophy (unlikely in older adults) Multiple sclerosis Polymyalgia rheumatica Polymyositis Hypothyroidism Vitamin D deficiency (osteomalacia) Diabetes (diabetic amyotrophy) Muscle disuse following fracture, injury or prolonged immobility Joints Osteoarthritis Rheumatoid arthritis Other Foot deformities Poor fitting shoes Specialist PSI Exercise Module Case Study 2 • • • • • • 75 year old woman 20 year history of diabetes poorly controlled by diet. High blood pressure and angina. Hip osteoarthritis Smokes 20/day What are the potential medical problems which may limit exercise ability/capacity? Specialist PSI Exercise Module Medications • 4/5 aged 75 or over prescribed at least one medication • Over one third on four or more • One drug may have a number of indications • Potential Impact on – Risk of falls – Exercise Capacity Specialist PSI Exercise Module For all Medication • Consider – – – – – – – Indications Main effects Side-effects including falls and exercise ability/capacity Idiosyncratic adverse effects Contra-indications Interactions with other drugs Compliance – Eg Atenolol Specialist PSI Exercise Module Common Indications • Cardiovascular Drugs •High blood pressure (Antihypertensives) •Angina •Abnormal Heart rhythms (Antiarrhythmic drugs •Drugs used to reduce clots (Antiplatelet/Anticoagulant drugs) • Drugs for diabetes • Drugs used in respiratory disease • Drugs for Parkinson’s Disease • Drugs acting on the brain (Psychotropic drugs) • Drugs for arthritis and connective tissue disorders • Drugs for osteoporosis Specialist PSI Exercise Module Drugs for high blood pressure • β – Blockers (atenolol, metoprolol etc) • Diuretics (Thiazide) • Calcium Channel Blockers (Nifedipine, Verapamil etc) • ACE Inhibitors (& Angiotensin receptor blockers) (Captopri, Enalarpril etc) • Often in combination • Not contraindicated for exercise Specialist PSI Exercise Module Drugs used in angina • β – Blockers • Nitrates (GTN and long acting) • Calcium Channel Blockers • Potassium Channel Openers (Nicorandil) • Often used in combination and statins (cholesterol lowering) also prescribed • • If patient has GTN, they should keep it with them when exercising and may consider using it prior to exercise. If patient forgets their GTN, recommend gentle exercise only Specialist PSI Exercise Module Drugs used in heart failure • Diuretics • ACE-Inhibitors • β – Blockers • Vasodilators • • Patients may have reduced exercise tolerance Patients may omit diuretics if going out, which may further reduce their exercise capacity - they should be advised to continue all medications Specialist PSI Exercise Module Antiplatelet drugs • After heart attacks, strokes, or when risk of clots • Antiplatelet -Aspirin (Acetyl Salicylic Acid – ASA) -Dipyridamole (Persantin) -Clopidogrel (Plavix) • Anticoagulant -Warfarin • Not a contraindication to exercise, but may increase risk of bleeding in the event of a fall, particularly if on both Aspirin and Clopidogrel Specialist PSI Exercise Module Anticoagulants • Warfarin • (Phenindione - rare) • Not a contraindication for exercise, but will increase risk of bleeding if patient falls Specialist PSI Exercise Module Antiarrhythmic drugs • • β – Blockers •Atenolol, Bisoprolol, Sotalol Calcium Antagonists •Verapamil, Diltiazem Digoxin • Amiodarone • Drugs for ventricular arrhythmias •Quinidine, Flecainide, Mexiletine, Disopyramide • • Patients on Digoxin or Amiodarone should be able to exercise Patients treated for Ventricular arrhythmias should only exercise with medical advice • Specialist PSI Exercise Module Drugs used in respiratory disease Inhaled therapy β2 Agonists Salbutamol (Ventolin), Terbutaline (Bricanyl) Long acting Salmeterol (Serevent, Seretide), Formoterol Anticholinergics Ipratropium Bromide (Atrovent), Tiotropium (Spiriva) Steroids Beclometasone (Becotide, Becloforte) Budesonide (Pulmicort), Fluticasone (Flixotide) Patients should have short-acting β2 Agonists with them when exercising Oral Therapy β2 Agonists Salbutamol (Ventolin) - rarely used Theophyllines Uniphyllin, Phyllocontin Steroids Immunomodulator Prednisolone Monteleukast, Zafirlukast - rarely used in older adults If on a course of steroids for acute exacerbation, not advisable to exercise Specialist PSI Exercise Module Drugs used in Parkinson’s disease L-Dopa Co-careldopa - Sinemet Co-beneldopa - Madopar Dopamine agonists Ergot-based - Pergolide, Cabergoline Bromocriptine - rarely used Non-Ergot - Pramipexole, Ropinirole COMT inhibitors Entacapone Other drugs MAO(B)-inhibitor - Selegiline Amantadine Anticholinergics - Trihexyphenidyl, Procyclidine Apomorphine injection - used in late disease Ability to exercise will depend on stage of disease and time of day Drug regimes can be complex - should not miss doses Specialist PSI Exercise Module Psychotropic drugs Anti-depressants Tricyclic - Amitriptyline, Dosulepin, Lofepramine SSRI’s - Citalopram, Sertraline, Fluoxetine SNRI - Venlafaxine Sedatives Benzodiazepines - Temazepam, Nitrazepam, Diazepam ‘Z drugs’ - Zopiclone, Zolpidem Phenothiazines Nausea - Prochlorperazine, Metoclopramide Agitation (usually acute) - Haloperidol New agents - Risperidone, Quetiapine All can cause sedation or confusion and increase falls risk Anti-dementia Donepezil (Aricept), Rivastigmine, Galantamine Despite modestly improving cognitive function, do not reduce falls risk Specialist PSI Exercise Module Drugs for arthritis and connective tissue disorders Analgesics Combination analgesics Paracetamol, Codeine, Tramadol Co-codamol, Co-dydramol Co-proxamol has been withdrawn Anti-inflammatory drugs Aspirin (only over the counter) NSAID’s - ibuprofen, diclofenac Disease-modifying drugs Immunosuppressants Steroids (e.g. Prednisolone) Azathioprine, Methotrexate, etc. Ensure patient has taken pain relief, or has it with them for after exercise Avoid exercise during acute flare-ups Specialist PSI Exercise Module Drugs for diabetes Oral hypoglycaemic agents Biguanides - Metformin Sulphonylureas - Gliclazide, Tolbutamide Glitazones - Pioglitazone, Rosiglitazone Insulin Human (recombinant, analogue) Beef or Pork (rarely used now) Long-acting - Insulatard, Glargine, Detamir Intermediate Acting - Mixtard, Novomix Short-acting - Actrapid, Humalog Glucose Dextrose tablets Glucogel (Hypostop) Specialist PSI Exercise Module Drugs for osteoporosis Calcium + Vitamin D Adcal D3, Calcichew D3 Forte, Cacit D3 Vitamin D insufficiency is common in older people Causes reduced bone and muscle strength Treatment reduces fractures by about one third in housebound or institutionalised older women, may also reduce falls Bisphosphonates Alendronic acid (Fosamax), Risedronate Build bones by slowing resorption. Robust evidence of fracture reduction (approx 50%) Other drugs Strontium ranelate, Teriparatide, Raloxifene HRT no longer recommended for osteoporosis due to adverse effects. Slows postmenopausal bone loss. Effect lost once withdrawn. Some concerns over increased risk of breast cancer. Specialist PSI Exercise Module Case Study 1 - Mrs A (age 75 years) History: Two falls Hypertension Type 2 diabetes Angina Sleep problems Glaucoma Medications: Zopiclone GTN spray Gliclazide Aspirin Atenolol Adcal D3 Questions: • • • Why is she on each medication? Which medications may be contributing to her falls? Are there any exercise considerations with these medications? Specialist PSI Exercise Module Case Study 2 - Mr. B (age 80years) Medications: Aricept Becotide Captopril Citalopram Co-dydramol Furosemide Salbutamol Questions: • • • What medical conditions might he have? Could any of these medications be contributing to his falls? Are there any exercise considerations of the medications? Specialist PSI Exercise Module If someone is prescribed the following drug(s), what conditions are they likely to have? a) Alendronic acid b) Diltiazem c) Pergolide and Co-careldopa (Sinemet) d) Mixtard Specialist PSI Exercise Module Useful Information Sources • www.prodigy.nhs.uk (patient and professional) • www.bnf.org.uk (need to register) • www.merck.com/mmpe (professional) • www.merck.com/mmhe (patient) • www.besttreatments.co.uk (patient) Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Notes Specialist PSI Exercise Module Implementation Making it work and making it sustainable Different models, but similar principles Specialist PSI Exercise Module IDEALLY - An Integrated Falls and Fracture Prevention Service • multi-professional Medical and Nursing staff, Therapists, Social Workers, Exercise Professionals • multi- agency Local health authority, Social services. Local authority , Leisure Services, Sports Development Service, Voluntary sector • co-ordinated Working to agreed protocols, Working to agreed pathways, Utilising agreed communication pathways • and integrated service Using a regular mechanism of meeting to agree strategy and review progress towards objectives Specialist PSI Exercise Module What should a service consider? • • • • Aims of Service To provide a seamless service across all agencies To promote personal responsibility for healthy active ageing To pro actively identify those at risk of falls and osteoporosis To ensure appropriate assessment and interventions for those at risk Specialist PSI Exercise Module 3-tiered inter agency assessment process:- 3. Specialist falls assessment 2. Determine risk factors 1. To identify a falls problem Specialist PSI Exercise Module Getting falls and fractures on the map • ? Trigger questions on falls and fractures in – A&E – GPs – Single Assessment process? • Educating others – Pharmacy, Opticians, Chiropodists, Day Centres – etc Specialist PSI Exercise Module Exercise Continuum 3 components:1. Community exercise opportunities that offer varied and progressive programme 2. Specific falls prevention (and injuries from falls) rehab class and 3. home based exercise programme Specialist PSI Exercise Module How? • Clinical Exercise Specialists creating links between health and leisure • Nationally validated courses:- CBE, OEP, PSI available to all professional groups • Additional ‘top up’ training to develop skills and standards of practice across all areas • ‘Code of practice’ – agreed minimum standards for all instructors in both health and leisure • List of approved classes (monitored and evaluated on a regular basis) Specialist PSI Exercise Module Community Exercise Programme Aim: to ensure that all older adults have easy access to a regular, safe and effective local exercise class • community • sheltered housing complex • day centre • residential home Specialist PSI Exercise Module Cambridgeshire Falls Prevention EXERCISE PATHWAY Falls Assessment Identification of a falls problem and screening to determine risk factors Motivation Screening Pathway Home based exercise programme OTAGO OTAGO exercise classes (Community based) Chair Based Exercise Class (Community based) PSI/Rehab based exercise group 12 weeks Exercise Referral Scheme 12 weeks Community based classes for older people Specialist PSI Exercise Module Transport issues……Funding issues • Link in with other services – – – – Exercise Referral Mental Health priorities Social Care funding Leisure Services • Consider self funding after initial period? – Often more valued and attendance better! • Consider ‘buddying’ shemes to aid travel – Going with people on the bus – Providing a lift – Bring along family (and their car!) Specialist PSI Exercise Module Challenges for future • Keeping falls and osteoporosis on agenda (different priorities across primary and secondary care and community) • financial constraints - demonstrating cost effectiveness • ongoing organisational changes • staff - rapid turnover - low morale Specialist PSI Exercise Module Conclusions • Falls and Fracture Prevention Services have come a long way in past 6 years. • In order to ensure ongoing funding locally, we must convince commissioners of cost effectiveness in terms of:- preventing falls related injuries. - maintaining independence and improved QOL for those at risk of falls and fractures (eg. Evaluation!) Be clear about the specific needs of this group of people (Not all exercise is the same!) Specialist PSI Exercise Module Assignments – Day One MANUAL 2 • Remind yourself of – the Selection and Exclusion Criteria for entry into the ‘prehab’ class (Manual 2 – Section 2) – the triggers for referral onto medical or other exercise settings (Manual 2 – Section 2) • Look at the Functional Assessments grid – read the protocols for the six functional tests (Manual 2 – Section 2) Specialist PSI Exercise Module Assignments – Day Two Underpinning Knowledge • Read over content covered in first two days of module • Read medical conditions and medications (Manual 1 Section 4) and exercise programming, theory and practice (Manual 2 Section 3) Specialist PSI Exercise Module Assignments – Day Two Case Study and Practical • Visit a Rehab AND a Prehab postural stability group – if possible! • Identify an individual appropriate for a Case Study and secure their agreement. – Discuss choice and method of approaching individual with therapist/instructor – Schedule start of your Case Study after days 2/3 Specialist PSI Exercise Module Assignments – Day Two Practical Workshop Prepare approximately ten minutes of one of the following: • Warm-up (circulation and mobility or stretch) • Resistance / bone loading (seated) • Dynamic Balance / Endurance • Backward Chaining + floor exercise • Floor work (considering transitions) • Flexibility • Tai Chi to teach as part of a teaching workshop on day 3/4 Specialist PSI Exercise Module Assignments – Day Four PSI Theory Paper • Revision – Do the Mock Theory Paper on the Website (Student Page) – Have a go at the Quiz on the Website (Student Page) – Remember that the PPT handouts cover most but you need to know your exercises and your delivery skills (theoretically) Tai Chi • Revise your Tai Chi skills as these will be assessed on Day 5 formatively Specialist PSI Exercise Module Notes Specialist PSI Exercise Module