How learning the skills of EBM relates to the pediatrics milestones
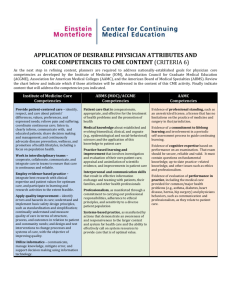
advertisement

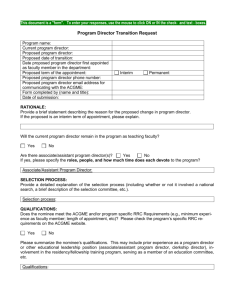
Not Just “MK-1” How learning the skills of EBM relates to the pediatric milestones Martha S Wright, MD, MEd Rainbow Babies and Children’s Hospital I have documented no financial relationships to disclose or Conflicts of Interest (COIs) to resolve. I am… • An EBM Teacher • Committed to helping learners develop these skills both for • Direct patient care • Life-long learning • A Program Director • Responsible for adhering to requirements • Mindful of competing demands and time limitations 3 Objectives • At the end of this session, you will be able to… – Describe how and where EBM skill development fits into the current paradigm of residency training requirements and performance assessment – Develop innovative curricula that integrate EBM training into current and emerging educational models 4 A brief history of “Competency-based Medical Education (CBME)” The ACGME Outcomes Project Pre-1999 1999 Relatively few actual requirements No duty hour restrictions ACGME/ABMS Adopt 6 Core Competencies And Sub-competencies 5 A brief history of “Competency-based Medical Education (CBME)” The ACGME Outcomes Project Pre-1999 1999 No duty hour restrictions Relatively few actual requirements 2002-2008 Residencies required to integrate The Competencies into their curricula ACGME/ABMS Adopt 6 Core Competencies And Sub-competencies 6 Core Competencies • Attempted to define what physicians should know and be able to do • Skills and tasks organized into 6 domains • Required us to find ways to teach, assess AND DOCUMENT resident performance in these domains 7 1999-2008: Job Security for EBM teachers EBM Skill development part of the PBLI competency From the ACGME Core Program Requirements: “Residents must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and lifelong learning. Residents are expected to develop skills and habits to be able to meet the following goals: locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems…” (ACGME 2003, 2007) 8 1999-2008: Job Security for EBM teachers Sackett, et al. publish Evidence-based Medicine: How to Practice and Teach EBM Explosion of GME Curriculum development Journal Clubs (traditional, guided) Stand-alone workshops, seminars On-line educational modules “On-the-job” training Morning report sessions Dedicated rotation blocks 9 Challenges for The Competencies • Did not result in assessments that documented resident ability “to practice independently” – Context independent – Assessment tools never fully developed – Assessments still process-focused • “Describe (a) how and by whom residents are taught to access, appraise, and apply knowledge and (b) how and by whom they are evaluated in so doing. • Describe (a) the evidence-based medicine exercise that residents complete during training and attach the tool used for assessment as Appendix B; and (b) if residents are given the option of choosing from more that one type of activity to fulfill this requirement, describe each one briefly. If no options exist, enter “NO” for (b).” 10 A brief history of “Competency-based Medical Education (CBME)” The ACGME Outcomes Project Pre-1999 1999 No duty hour restrictions Relatively few actual requirements The ACGME Milestones Project 2002-2008 2012 Residencies required to integrate The Competencies into their curricula ACGME/ABMS Adopt 6 Core Competencies And Sub-competencies 2014 Residencies report data on 21 Milestones to ACGME ABP publishes 48 Pediatric Milestones 11 2012: What the milestones added • Descriptions of level-specific learner behaviors along a developmental continuum • Prompted for a longitudinal approach to teaching and assessment of skill from knowledge to bedside application • Required observation-based assessments 12 Pediatricians Understand Milestones 13 MK-1: “The EBM milestone” 14 Teaching and Learning EBM Skills Acquire knowledge and skills Longitudinal experiences Use and practice at the bedside 15 Teaching and Learning EBM Skills • Acquire knowledge and skills – Didactics – E-learning modules – Small group activities – Computer labs • Longitudinal experiences – Journal Clubs – CATs – On-going didactics • Use and practice at the bedside – Role modeling – Educational prescriptions – Medical librarian on rounds – Blogs, wikis – Mobile devices, Apps 16 Pediatric Milestones PC1: Should I get a CXR on this asthmatic? PC4: Which antibiotic should I choose for this soft tissue infection? PBLI 2: What would be the best source to read about CAP? Challenges of the Milestones • Do not assess learners holistically – Milestones can help us assess where the learner is along the continuum of individual skill development: • “gather accurate information about a patient” • “locate evidence related to their patient’s health problems” – They don’t tell us whether someone can put it all together to take care of a patient 18 A brief history of “Competency-based Medical Education (CBME)” The ACGME Outcomes Project Pre-1999 1999 No duty hour restrictions Relatively few actual requirements The ACGME Milestones Project 2002-2008 2012 Residencies required to integrate The Competencies into their curricula ACGME/ABMS Adopt 6 Core Competencies And Sub-competencies 2015 2014 Residencies report data on 21 Milestones to ACGME 48 Pediatric Milestones published by ABP ABP “finalizes” Pediatric EPAs 19 Entrustable Professional Activities (EPAs) • Describe routine activities of a pediatrician in specific contexts • Require “workplace-based” application and assessment of skills (e.g. “OPAs” Observed Practice Activities) 20 1. Provide consultation to other health care providers caring for children 2. Provide recommended pediatric health screening 3. Care for the well newborn 4. Manage patients with acute, common diagnoses in an ambulatory, emergency, or inpatient setting 5. Provide a medical home for well children of all ages. Pediatric EPAs 6. Provide a medical home for patients with complex, chronic, or special health care needs. 7. Recognize, provide initial management and refer patients presenting with surgical problems 8. Facilitate the transition from pediatric to adult health care 9. Assess and manage patients with common behavior/mental health problems 10. Resuscitate, initiate stabilization of the patient and then triage to align care with severity of illness 11. Manage information from a variety of sources for both learning and application to patient care 12. Refer patients who require consultation 13. Contribute to the fiscally sound and ethical management of a practice (e.g. through billing, scheduling, coding, and record keeping practices) 14. Apply public health principles and quality improvement methods to improve care and safety for populations, communities, and systems 15. Lead an interprofessional health care team 16. Facilitate handovers to another healthcare provider either within or across settings 17. Demonstrate competence in performing the common procedures of the general pediatrician 21 1. Provide consultation to other health care providers caring for children 2. Provide recommended pediatric health screening 3. Care for the well newborn 4. Manage patients with acute, common diagnoses in an ambulatory, emergency, or inpatient setting 5. Provide a medical home for well children of all ages. Pediatric EPAs 6. Provide a medical home for patients with complex, chronic, or special health care needs. 7. Recognize, provide initial management and refer patients presenting with surgical problems 8. Facilitate the transition from pediatric to adult health care 9. Assess and manage patients with common behavior/mental health problems 10. Resuscitate, initiate stabilization of the patient and then triage to align care with severity of illness 11. Manage information from a variety of sources for both learning and application to patient care 12. Refer patients who require consultation 13. Contribute to the fiscally sound and ethical management of a practice (e.g. through billing, scheduling, coding, and record keeping practices) 14. Apply public health principles and quality improvement methods to improve care and safety for populations, communities, and systems 15. Lead an interprofessional health care team 16. Facilitate handovers to another healthcare provider either within or across settings 17. Demonstrate competence in performing the common procedures of the general pediatrician 22 EPA Title Care for the normal well newborn The functions of this activity include: Performing a physical examination to look for congenital anomalies Identifying and applying key evidence based guidelines for care of the newborn Caring for common problems that develop primarily in the nursery Using judgment to know when common problems can be handled at home and arrange for discharge and follow-up Assessing maternal/family readiness to care for the infant post discharge Transitioning care to the community practitioner Demonstrating confidence that puts new parents at ease Link with Domains of Competence Critical Competencies _X_ Patient Care ___ Medical Knowledge _X_ Practice-based Learning and Improvement _X_ Interpersonal & Communication Skills ___ Professionalism ___ Systems-based Practice _X_ Personal & Professional Development PC 3: Transfer of care PC 5: Physical exam MK 2/PBLI 6: EBM ICS 1: Communicate with patients PPD 7: Self-confidence 23 (updated ABP 3/11/14) Integration of EBM learning, practice and assessment into the Clinical Environment • Demonstration of skills with direct observation in the “workplace” 1998 2015 24 Opportunities • Assessment of EBM skills by direct observation in the clinical environment • Observation tool development • Educator development • Use of clinical decision tools in bedside decision making • Life-long learning curricula • The Art of “Keeping Up” • High Value, Cost-Conscious Care • Requires understanding of guidelines, systematic reviews, diagnostic testing, therapy/harm • The next EBM frontier 25 Summary • In 2015 there is still a place in residency training for teaching and learning EBM skills • EBM curricula should focus on the continuum from knowledge acquisition to application in the clinical environment • Educators will need to: – integrate educational activities into the existing/evolving clinical workflow – create authentic opportunities for learners to demonstrate and teachers to assess EBM skill application 26 Questions???? 27